Pediatric proximal radioulnar translocation is a rare injury associated with high rates of complications and is essential to identify when present
Dr. Alyssa Barré, Department of Orthopaedic Surgery and Sports Medicine, University of Kentucky, 740 S Limestone, Kentucky Clinic, Floor 1, Wing C, Lexington - 40536, Kentucky, United States. E-mail: alyssa.barre@uky.edu
Introduction: While pediatric elbow dislocations are a common injury, rare variants of this injury exist including translation of the proximal radius and ulna. This injury is associated with high rates of neurovascular injury and delayed diagnosis. This report discusses a case of proximal radioulnar translocation, emphasizes the importance of early detection, and describes a closed reduction (CR) technique, which has not previous been described.
Case Report: A 9-year-old presented to our hospital with a proximal radioulnar translocation with ulnar nerve paresthesias. CR was successful via the technique described in this article. Open ulnar nerve exploration was performed with only bruising to the nerve. The paresthesias resolved and she had full elbow functional range of motion and had returned to gymnastics at her two-year follow-up.
Conclusion: Pediatric proximal radioulnar translocations are a rare injury with less than 30 documented in the literature. Although rare, they have high rates of complications including nerve injuries, and are often missed. Effective CR can lead to a favorable outcome without the need for open surgery. A CR technique is illustrated in this article.
Keywords: Elbow dislocation, proximal radioulnar translocation, closed reduction, pediatric trauma.
Pediatric elbow dislocations are uncommon, accounting for 3–6% of all elbow injuries [1,2] with an average age around 10–11 years [2,3]. They are typically classified based on the displacement of the radius and ulna. Posterior and posterolateral are the most common, but anterior, medial, lateral, convergent, and divergent dislocations also occur. Convergent dislocation involves the translocation of the proximal radius and ulna, while in divergent dislocation the ulna displaces medially and the radius displaces laterally [4]. The first reported case of a convergent dislocation case was documented by Harvey and Tchélébi in 1979 [5]. Since that time, including this report, there have been 27 cases of elbow dislocation with proximal radius-ulna translocation reported in the literature in the pediatric population [1,5-23] and multiple in the adult literature [14,24,25]. No closed reduction (CR) maneuver has been published. This injury is often missed initially or misdiagnosed. Patients will present with elbow pain, swelling, fixed pronation, and occasionally neurovascular injuries. Delayed recognition may lead to poor functional results [5,8,14,19]. The key to diagnosis is early radiographic recognition of disruption of the radiocapitellar relationship. A line through the proximal radius should intersect the capitellum in all radiographic planes. Computed tomography (CT) scan may also aid in diagnosis [20]. This report presents a case of early detection and CR of an elbow dislocation with proximal radioulnar translocation and reviews existing pediatric cases. It also includes a detailed description of the CR technique.
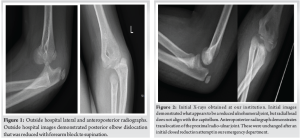
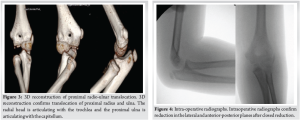
A 9-year-old female fell from a bunk bed onto an outstretched arm, initially diagnosed with a left elbow dislocation at a community hospital (Fig. 1). Despite CR attempts and improvement in flexion and extension, she remained in fixed pronation and was transferred to our hospital for further evaluation. On arrival, three view radiographs of the left elbow were obtained and demonstrated a proximal radioulnar translocation (Fig. 2). CR was again attempted in our emergency department with no change in the radiographic appearance. A CT scan was obtained due to concern for intra-articular fragment blocking reduction. Instead, it more clearly showed a radioulnar translocation. Fig. 3 is the 3D reconstruction of the elbow which shows the ulna articulating with the capitellum and the radius articulating with the trochlea, consistent with this diagnosis.
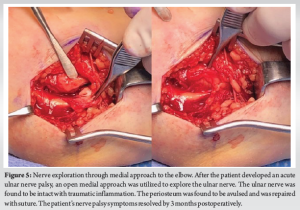
Overnight, the patient developed an ulnar nerve palsy that was not present in the initial evaluation at either hospital. The patient was acutely taken to the operating room for reduction and ulnar nerve exploration. Concentric reduction was achieved via CR using the technique described below. Intraoperative fluoroscopy confirmed reduction with the restoration of the radiocapitellar and ulna-trochlear articulation (Fig. 4). After reduction, the elbow had full passive flexion, extension, pronation, and supination compared to contralateral side. Due to her acute ulnar nerve symptoms, it was felt she then warranted exploration of her ulnar nerve. A medially based incision was made to explore the ulnar nerve which was intact but bruised (Fig. 5). The medial periosteum had been avulsed from the distal humerus and was repaired with suture. Throughout the range of motion, there was no subluxation of the ulnar nerve. The patient was placed into a long arm splint for 2 weeks and subsequently transitioned to a hinged elbow brace.
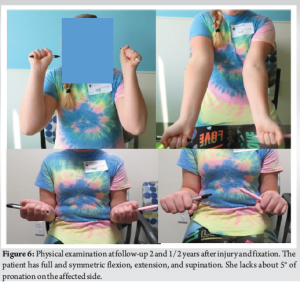
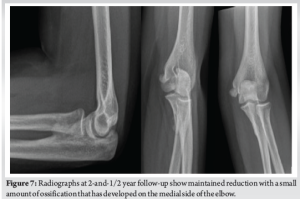
By 3 months postoperatively, her ulnar nerve palsy symptoms had resolved. Radiographs demonstrated maintenance of reduction of the radiocapitellar and ulna-trochlear joints (Fig. 6). At follow-up 2 and 1/2 years after the injury, the patient had resumed her previous level of function. On examination, she had full and symmetric flexion and extension, full supination, and lacked only 5° of pronation when compared to the unaffected side (Fig. 6). She had normal sensation and distal motor function. Radiographs from this follow-up show maintained reduction with a small amount of ossification medially, thought to be due to previous periosteal avulsion from her dislocation (Fig. 7).
CR technique
A key aspect of a successful CR of a pediatric proximal radio-ulnar translocation is the successful identification of the injury before the reduction attempt. Once identified, the following reduction maneuver (Fig. 8a, b, c) can be attempted:
- Position the patient supine with the arm extended
- Reduce ulnohumeral dislocation first if present
- Palpate the head of the radius, noting that it will be medial to its typical anatomic position
- Position one hand around the patient’s distal forearm, and one around the elbow so that the thumb is positioned directly over the radial head (Fig. 8a)
- Using the hand around the distal forearm, apply axial traction through the elbow. At the same time, hyper pronate the patient’s forearm (Fig. 8b)
- Using the hand positioned at the elbow, apply direct pressure over the radial head. At the same time, use the other hand to apply forced supination to the forearm (Fig. 8c).

Elbow dislocations with proximal radioulnar translocations are rate in pediatrics, with 27 cases reported in the literature (Table 1). Proposed mechanisms include axial loading to the proximal radius after a fall onto a hyperpronated and outstretched hand. Isbister proposed that it is due to axial loading with a valgus stress on an outstretched supinated hand [9]. Harvey described it as an iatrogenic injury as a result of traction and pronation during attempted CR without appropriate identification of the injury [5]. The exact mechanism is difficult to determine, however, Keny et al. recently published a cadaveric study illustrating this mechanism on a cadaveric model, showing forearm hyperpronation with a valgus strain on the elbow, causing rupture of the medial collateral ligament, followed by the radial collateral ligament and ulnar insertion of the annular ligament, leading to transposition of the radius and ulna [21]. Identification of the injury in a timely manner is important for restoration of elbow function.
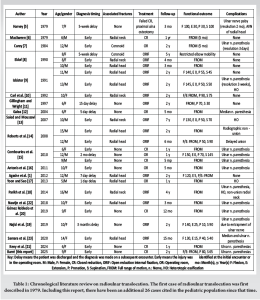
Most cases required open reduction (n = 21, 78%) with or without internal fixation to restore a congruent elbow joint [1,5,7-19,22,23]. Six cases (22%) were successfully treated with CR [6,15,20,21]. Often, these injuries are accompanied by other fractures including the radial head, radial neck, and coronoid process. Fourteen (52%) cases involved a radial head or neck fracture [1,6,8-10,13,14,17,18,22,23]. Two cases (7%) had an associated coronoid process fracture [7,8]. Only eleven cases (41%) had no associated concurrent fractures [5,11,12,15,16,19,20,21]. The most common complication in this review was incomplete ulnar nerve palsy which occurred in 14 cases (52%), all of which recovered within 1 year [5,7,9,15,16,18-23]. Additional complications were ulnar nerve entrapment within the proximal radioulnar joint (n = 1) [19], median nerve palsy (n = 2) [12,23], heterotopic ossification (n = 4) [9,13,17,18], non-union or malunion of the proximal radius after fixation (n = 2) [14,18], and avascular necrosis of the radial head (n = 1) [5]. The injury is often missed or misdiagnosed on presentation. Thirty percent (8) of the injuries were missed, with delay in care ranging from 1 day to 3 months [1,5,8,11,12,15,17,19]. There are a variety of reasons why the injury may initially go unrecognized. First, this injury is rare, and treating providers may be unaware of it and fail to recognize the injury pattern. Second, most commonly reported, during CR a palpable clunk is often felt giving the false sense of reduction [20,22]. Third, the lateral radiograph may appear reduced. Evaluation of the anterior-posterior radiograph is necessary to appreciate the translocation. Fourth, post-reduction, there is an increase flexion-extension arc of the forearm. However, the forearm remains pronated with minimal supination, a term referred to as “pseudoreduction” [1,7,20,22]. To avoid misdiagnosis and a delay in treatment, it is essential to recognize the injury, assess the lateral and the anterior-posterior radiographs with scrutiny, perform CR when possible, and proceed to the operating room when CR is not successful. In our review, 83% of these cases required open reduction.
This report provides a CR technique consisting of axial traction, hyperpronation followed by forced supination, and direct pressure on the radial head to successfully reduce a proximal radio-ulnar translocation when identified early and appropriately.
This case underscores the importance of vigilance in diagnosing complex elbow injuries and highlights the efficacy of timely identification and CR of proximal radioulnar translocations. Despite initial challenges and acute ulnar nerve palsy that underwent exploration, our patient achieved complete functional recovery without the need for an open reduction. The CR maneuver is detailed in this paper. The patient’s ulnar nerve symptoms completely resolve within 3 months. Two years later, they have full range of motion and are actively participating in gymnastics with no limitations. Physicians must maintain a high index of suspicion for these injuries, carefully evaluating radiographs and promptly intervening when indicated.
Pediatric proximal radioulnar translocation is a rare injury that is critical to identify when present, as it is associated with a high rate of missed injury, neurovascular compromise, and need for open reduction. CR is possible and can lead to a favorable outcome without the need for open surgery. A technique is described in this article. This project was undertaken as a case report project at Shriners Hospitals for children and, as such, was not formally supervised by an Institutional Review Board.
References
- 1.Agashe MV, Samant A, Aroojis AJ. Convergent radioulnar translocation with radial head fracture in a child: A case report and review of the literature. J Orthop Trauma 2012;26:e36-9. [Google Scholar | PubMed]
- 2.Hyvönen H, Korhonen L, Hannonen J, Serlo W, Sinikumpu JJ. Recent trends in children’s elbow dislocation with or without a concomitant fracture. BMC Musculoskelet Disord. 2019;20:294. [Google Scholar | PubMed]
- 3.Lewallen L, Elliott ME, McIntosh A, Ho CA. Pediatric elbow dislocations and associated fractures. Children (Basel) 2023;10:993. [Google Scholar | PubMed]
- 4.Waters PM, Skaggs DL, Flynn JM, Andras L, Bae DS, Baldwin KD, et al. Rockwood and Wilkins’ Fractures in Children. 9th ed. Philadelphia, PA: Wolters Kluwer; 2020. [Google Scholar | PubMed]
- 5.Harvey S, Tchélébi H. Proximal radio-ulnar translocation. A case report. J Bone Joint Surg Am 1979;61:447-9. [Google Scholar | PubMed]
- 6.MacSween WA. Transposition of radius and ulna associated with dislocation of the elbow in a child. Injury 1979;10:314-6. [Google Scholar | PubMed]
- 7.Carey RP. Simultaneous dislocation of the elbow and the proximal radio-ulnar joint. J Bone Joint Surg Br 1984;66:254-6. [Google Scholar | PubMed]
- 8.Eklöf O, Nybonde T, Karlsson G. Luxation of the elbow complicated by proximal radio-ulnar translocation. Acta Radiol 1990;31:145-6. [Google Scholar | PubMed]
- 9.Isbister ES. Proximal radioulnar translocation in association with posterior dislocation of the elbow. Injury 1991;22:479-82. [Google Scholar | PubMed]
- 10.Carl A, Prada S, Teixeira K. Proximal radioulnar transposition in an elbow dislocation. J Orthop Trauma 1992;6:106-9. [Google Scholar | PubMed]
- 11.Gillingham BL, Wright JG. Convergent dislocation of the elbow. Clin Orthop Relat Res 1997;340:198-201. [Google Scholar | PubMed]
- 12.Galea A. An unusual case of elbow dislocation in a child: Crossover of radius and ulna. J Trauma 2004;57:1125-6. [Google Scholar | PubMed]
- 13.Saied A, Moussavi AA. Elbow dislocation translocation in a child: A case report. J Shoulder Elbow Surg 2007;16:e17-9. [Google Scholar | PubMed]
- 14.Roberts C, Lee TS, Rooney J, Jovanovic A, Creer R. Convergent dislocation of the elbow: Report of three cases. J Shoulder Elbow Surg 2008;17:e9-13. [Google Scholar | PubMed]
- 15.Combourieu B, Thevenin-Lemoine C, Abelin-Genevois K, Mary P, Damsin JP, Vialle R. Pediatric elbow dislocation associated with proximal radioulnar translocation: A report of three cases and a review of the literature. J Bone Joint Surg Am 2010;92:1780-5. [Google Scholar | PubMed]
- 16.Antonis K, Leonidou OA, Sbonias G, Fligger L. Convergent type proximal radioulnar translocation complicating posterior elbow dislocation: Watch out for dual dislocations in children’s elbows. J Pediatr Orthop B 2011;20:138-41. [Google Scholar | PubMed]
- 17.Yoon HK, Seo GW. Proximal radioulnar translocation associated with elbow dislocation and radial neck fracture in child: A case report and review of literature. Arch Orthop Trauma Surg 2013;133:1425-9. [Google Scholar | PubMed]
- 18.Parikh SN, Lykissas MG, Mehlman CT, Sands S, Herrera-Soto J, Panchal A. Convergent and divergent dislocation of the pediatric elbow: Two case reports and comprehensive review of literature. J Pediatr Orthop B 2014;23:158-67. [Google Scholar | PubMed]
- 19.Najid H, Abdul Rashid AH, Ibrahim S. Missed proximal radioulnar joint translocation with ulnar nerve entrapment: An unusual injury in a child. J Pediatr Orthop B 2019;28:79-84. [Google Scholar | PubMed]
- 20.Gómez Robledo J, Díez Lizuaín ML. An unusual case of posterior elbow dislocation with proximal radioulnar translocation. Rev Esp Cir Ortop Traumatol (Engl Ed) 2019;63:69-74. [Google Scholar | PubMed]
- 21.Keny S, Modi N, Haidermota M, Modi N, Haidermota M, Gokhale N, et al. ‘PRUT’ - a cadaveric study to understand the mechanism of this rare paediatric elbow injury with a comprehensive review of literature. Trauma Case Rep 2024;52:101067. [Google Scholar | PubMed]
- 22.Nawijn F, Emmink BL, Keizer J, Bosman WM. Paediatric forearm fracture with a twist: A proximal radioulnar translocation combined with radial head fracture. BMJ Case Rep 2018;2018:bcr2017-223228. [Google Scholar | PubMed]
- 23.Samara E, Dayer R, Davat M, Ruffieux E, Steiger CN, Ceroni D. Proximal radioulnar translocation associated with posterior fracture-dislocation of elbow in an adolescent girl: A case report. JBJS Case Connect 2020;10:e0445. [Google Scholar | PubMed]
- 24.Al-Hadithy N, Mulligan A, Babu S, Van Rensburg L. Proximal radioulnar translocations in adults: A tertiary centre study. Eur J Orthop Surg Traumatol 2020;30:851-8. [Google Scholar | PubMed]
- 25.Lippe CN, Williams DP. Combined posterior and convergent elbow dislocations in an adult. A case report and review of the literature. J Bone Joint Surg Am 2005;87:1597-600. [Google Scholar | PubMed]









