Metacarpophalangeal joint arthrodesis with temporary interphalangeal joint pinning is a viable treatment option to preserve function in a young, high-demand patient with severe thumb boutonniere deformity with interphalangeal joint dislocation.
Dr. Jeffrey G. Stepan, MD, Department of Orthopaedic Surgery and Rehabilitation Medicine, 5841 S. Maryland Ave, MC3079, Chicago, Illinois, United States. 60637 Email: jstepan@bsd.uchicago.ed
Introduction: Thumb boutonniere deformity, commonly associated with autoimmune arthropathies, presents as metacarpophalangeal (MCP) joint flexion and interphalangeal (IP) joint hyperextension. Literature guiding management remains incomplete and out-of-date, and it largely addresses low-demand populations. IP joint dislocation is a particularly severe presentation that notably has only been reported once before.
Case Report: We report a rare case of severe Type 1 thumb boutonniere deformity with IP joint dislocation in a 42-year-old, high-demand female patient with a history of autoimmune diseases. We describe the successful treatment of this severe thumb deformity using MCP arthrodesis and temporary IP joint pinning, which resulted in preserved function and stability. At 1-year follow-up, the patient reported good function of the thumb with no instances of IP joint dislocation.
Conclusion: In prior literature, MCP arthroplasty with IP arthrodesis has been recommended in severe thumb boutonniere deformities, but this may be inappropriate for younger, higher-demand patients. Surgeons should obtain a comprehensive understanding of each patient’s anatomy and functional goals to best develop treatment strategies. The success of MCP arthrodesis and temporary IP joint pinning in this population is evidenced by the maintained IP joint range of motion and lack of dislocation with pinch and grip activities at 1 year follow-up.
Keywords: Boutonniere deformity, dislocation, interphalangeal joint, arthrodesis, pinning, thumb, young.
Chronic autoimmune disorders, such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), are commonly characterized by widespread inflammation resulting in both systemic complications and joint deformities [1, 2]. One hallmark of these disorders, particularly RA, is involvement of the hand, where deformities can significantly impact a patient’s quality of life [1-3]. Advances in the management of autoimmune disease, such as the introduction of disease-modifying antirheumatic drugs and biologics, have contributed to a decline in the prevalence of severe hand deformities in recent years [4, 5]. However, there remain instances where patients may present with unique and challenging deformities. Among the spectrum of hand deformities, boutonniere deformity is a notable malformation resulting from an imbalance between the extensor and flexor mechanisms [5, 6]. While boutonniere deformity is well-documented in the fingers, its occurrence in the thumb demands special attention due to the digit’s unique anatomical and functional aspects. Thumb boutonniere deformity is thought to develop secondary to metacarpophalangeal (MCP) joint synovitis and attenuation of the surrounding soft structures. The proximal phalanx subluxates volar on the metacarpal head and the extensor mechanism attenuates, at which point the extensor pollicis longus (EPL) can subluxate volar and ulnar leading to secondary interphalangeal (IP) joint deformities [3, 5, 6]. We report a case of severe thumb boutonniere deformity with dislocation of the IP joint in a young female patient. The treatment of advanced type 1 deformity is not well described with few published cases, often with recurrence of IP joint deformity and unsatisfactory results [7]. The presence of complete dislocation at the IP joint is rare with few reports in the literature, and there is thus a lack of guidance regarding management of such advanced deformities, especially in younger populations. We present a case of a young patient with an advanced Type 1 boutonniere deformity with IP joint dislocation. The patient was informed that data concerning the case would be submitted for publication, and she provided consent. This case report adheres to CARE reporting guidelines.
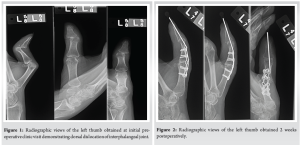
Our patient is a 42-year-old right-hand dominant female with a longstanding history of RA, SLE, Sjogren’s syndrome, and Raynaud’s syndrome who presented to hand clinic 3 days after developing the atraumatic inability to extend her left thumb at the MCP joint. She reported that the deformity was painless, had never occurred previously, and was associated with a clicking and popping sensation. She has suffered from joint pain since her mid-twenties, and her autoimmune conditions were being treated with methotrexate, hydroxychloroquine, and methylprednisolone, as well as a variety of biologics. On physical exam, the thumb was held in the boutonniere deformity, which was further provoked by the extension of the digit. A notable “clunk” was felt secondary to dorsal dislocation of the distal phalanx, which was passively but not actively reducible. With the MCP joint held reduced, her IP joint did not dislocate with active extension. She maintained full passive range of motion of the thumb MCP and IP joints, and there was no obvious subluxation of the EPL noted on inspection. Sensation to light touch was preserved throughout the median, ulnar, and radial nerve distributions, and the patient reported no pain. Radiographic views of the left thumb were obtained, demonstrating dorsal dislocation of the IP joint of the thumb and flexion at the MCP joint (Fig. 1). Clinical and radiological findings were consistent with severe boutonniere deformity of the thumb. The patient was provisionally provided a thumb spica brace to support the thumb in a corrected position, though she noticed recurrent dislocation as well as the emergence of pain over the next weeks.
Operation
Definitive surgical treatment was planned with fusion of the MCP joint and pinning of the IP joint. During the surgery, the EPL tendon did not exhibit volar subluxation, and the extensor pollicis brevis was attenuated. We then proceeded with preparation of the joint for fusion using a sagittal saw, and a ladder plate was utilized to fuse the MCP joint at 20 degrees of flexion with slight palmar abduction and slight pronation. A 0.045” pin was placed across the IP joint in a retrograde fashion with the thumb reduced in flexion.
Post-operative course
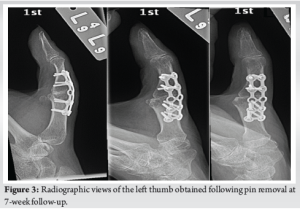
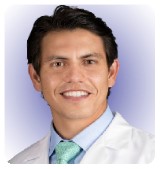
At 2 weeks follow-up, there was no evidence of hardware migration, the thumb was well-reduced, and the patient was placed in a thumb spica cast (Fig. 2). The pin and cast were removed at 7 weeks (Fig. 3), at which time the patient exhibited signs of good clinical healing and was provided a thumb spica brace.
At 10 weeks, she was gradually returning to activities, and her thumb was well-reduced with intact flexion and extension at the IP joint. The thumb remained well-reduced at 9-month follow-up, and she denied any issues with use of her thumb at that time.
At 1-year follow-up, the patient reported good function of the thumb with no instances of IP joint dislocation. Passive hyperextension of the IP joint was noted on physical exam, but she could not be dislocated passively. In addition, the IP joint remained reduced with flexion and extension (Fig. 4), and she could pinch without IP joint subluxation or dislocation (Fig. 5). The patient was pain-free in her thumb. Final radiographic imaging at this time demonstrated stable fixation of the thumb without evidence of hardware migration or failure (Fig. 6).

Thumb boutonniere deformity, characterized by an imbalance of flexion and extension forces, is a well-recognized consequence of RA and autoimmune disorders. The severity of this case was likely compounded by the presence of SLE, which may have contributed to increased joint laxity – SLE-related joint deformities are predominantly characterized by soft-tissue laxity and commonly lack the bony erosions observed in RA. Although boutonniere deformity commonly results in instability at the MCP and IP joints, complete dislocation at the IP joint has only been noted in one previous study grouped together with “advanced” Type 1 deformity, [7] and is particularly consequential in younger, high-demand patients. A nuanced understanding of thumb boutonniere deformity is crucial in guiding appropriate treatment strategies in such cases, as treatment options are varied. Various classification systems have been used to grade joint involvement and deformity severity, and cases may generally be conceptualized as early, moderate, or advanced [3, 5, 8, 9]. In early cases, characterized by a passively correctable MCP joint deformity, near-normal IP joint posture, and minimal functional loss, conservative management is typically employed. This includes the use of splints to maintain correct alignment and occupational therapy to enhance range of motion and strength [3, 4, 6, 8]. Moderate deformities, which typically feature a fixed MCP joint deformity, passively correctable IP joint, and noticeable functional impairment, may also necessitate a combination of splinting and therapeutic exercises, though certain surgical options may also be considered at this stage, such as synovectomy and extensor mechanism repair (e.g., EPL rerouting techniques) [5, 6, 8, 9]. Advanced deformities are debilitating conditions with fixed MCP and IP joint deformity, dislocation, and/or joint destruction, and such cases often require surgical intervention [3, 5, 8, 9]. Common surgical interventions include centralization procedures, terminal tendon tenotomy, and soft-tissue procedures, though more advanced deformities with intact cartilage may be treated with central slip reconstruction [3-6,8,10]. In the case of articular destruction and/or severe contracture, arthrodesis is a reliable option for increased stability, deformity correction, and pain control, especially in isolated MCP involvement; arthroplasty may also be considered in low-demand patients [3, 6, 7, 9, 10]. Overall, treatments aim to prevent deformity progression, bolster stability, and maintain functionality [1, 3, 5, 6]. Various surgical options were considered in the pre-operative planning of our case. MCP arthroplasty with IP arthrodesis would typically be considered in such a severe thumb deformity, but this approach would restrict long-term functionality and be inappropriate in a young, high-demand patient [7, 9]. Soft-tissue rearrangement and centralization procedures for reconstruction of the EPL line of pull were also ruled out given the dislocation at the IP joint and the absence of EPL subluxation. Our ultimate surgical approach involved MCP joint fusion and IP joint pinning, driven by the need for stability and definitive deformity correction while preserving lasting IP joint function in a young patient. MCP fusion is posited to be the most reliable treatment method of the rheumatoid thumb, providing rapid and predictable results – arthrodesis has been reported to result in greater pinch strength and lower rates of IP joint progression postoperatively relative to other techniques [3, 6]. Arthrodesis of the MCP joint in a functional position also allowed for correction of the IP joint dislocation, with temporary IP pinning conferring further stability to the joint. This improvement in stability persisted after the removal of pins with preserved flexion and extension, and the overall success of the approach is evidenced by the maintained IP joint range of motion and lack of dislocation with pinch and grip activities at 1-year follow-up.
A comprehensive understanding of each patient’s anatomy and functional goals is pivotal in tailoring treatment strategies, and literature guiding the management of thumb boutonniere deformity remains incomplete. We reported on a case of severe thumb boutonniere deformity with dorsal dislocation at the IP joint in a young patient. This deformity is both rare and debilitating, and emerging treatment techniques must address the need to preserve function in such high-demand patients. We describe successful treatment with preservation of function utilizing MCP arthrodesis and temporary IP joint pinning in such a patient.
Severe thumb boutonniere deformity with dorsal dislocation at the IP joint in a young patient is both rare and debilitating. Literature guiding management remains incomplete, outdated, and largely addresses low-demand populations, which may be inappropriate for younger patients. MCP arthrodesis with temporary IP joint pinning is a viable, emerging treatment option to preserve function in a young, high-demand patient with such a thumb boutonniere deformity with IP joint dislocation.
References
- 1.Dwivedi S, Testa EJ, Modest JM, Ibrahim Z, Gil JA. Surgical management of rheumatoid arthritis of the hand. R I Med J (2013) 2020;103:32-6. [Google Scholar]
- 2.Chen SL, Zheng HJ, Zhang LY, Xu Q, Lin CS. Case report: Joint deformity associated with systemic lupus erythematosus. Immun Inflamm Dis 2022;10:e717. [Google Scholar]
- 3.Boyer MI, Gelberman RH. Operative correction of swan-neck and boutonniere deformities in the rheumatoid hand. J Am Acad Orthop Surg 1999;7:92-100. [Google Scholar]
- 4.Rehim SA, Chung KC. Applying evidence in the care of patients with rheumatoid hand and wrist deformities. Plast Reconstr Surg 2013;132:885-97. [Google Scholar]
- 5.Oda R, Toyama S, Fujiwara H. A new approach for the correction of type I thumb deformity owing to rheumatoid arthritis. J Hand Surg Glob Online 2020;2:55-60. [Google Scholar]
- 6.Terrono AL. The rheumatoid thumb. J Am Soc Surg Hand 2001;1:81-92. [Google Scholar]
- 7.7. Terrono A, Millender L, Nalebuff E. Boutonniere rheumatoid thumb deformity. J Hand Surg Am 1990;15:999-1003. [Google Scholar]
- 8.Nalebuff EA, Millender LH. Surgical treatment of the boutonniere deformity in rheumatoid arthritis. Orthop Clin North Am 1975;6:753-63. [Google Scholar]
- 9.Terrono A, Millender L. Surgical treatment of the boutonniere rheumatoid thumb deformity. Hand Clin 1989;5:239-48. [Google Scholar]
- 10.Lee JK, Lee S, Kim M, Jo S, Cho JW, Han SH. Anatomic repair of the central slip with anchor suture augmentation for treatment of established boutonniere deformity. Clin Orthop Surg 2021;13:243-51. [Google Scholar]