Brachial plexus palsy must be anticipated in cervicothoracic scoliosis, especially while performing correction maneuvers despite adequate preventive measures
Dr. Shreya Shenoy, SKS Hospital and Postgraduate Medical Institute, Salem, Tamil Nadu, India. Email address: shreyasemail2@gmail.com
Introduction: Correction of spinal deformity in the pediatric age group is associated with a neurological complication at a rate of 0.71–0.94%. Of these, primary brachial plexus traction palsies have been rarely reported.
Case Report: We present two cases of complex painless spinal deformity in growing children, managed initially with halo gravity traction with post-operative transient brachial plexus palsy diagnosed on post-operative day 1. Post-operative magnetic resonance imaging showed edema around the brachial plexus which resolved at 4 weeks in both cases.
Conclusion: Transient brachial plexus palsy may present postoperatively in patients with excessive correction of neck tilt angle and T1 slope angle. They generally have a good prognosis with medical management and the surgeon need not rush with a decision on re-exploration.
Keywords: Brachial plexus, lower brachial plexus palsy, post-operative complication, scoliosis.
Correction of spinal deformity in the pediatric age group is associated with a neurological complication at a rate of 0.71–0.94% [1, 2]. Neurological complications are points of concern for the child and the parents, as the resulting clinical effects are devastating for the growing child [3]. It adds on to the morbidity surrounding the surgery. Since 1975, the scoliosis research society has been instrumental in recording the complications associated with spinal deformity corrections. Their morbidity and mortality database reports an increase in the prevalence of neurological complications as the operation rate of scoliosis increases [4]. The neurological complications have been further attributed and divided according to risk associated into surgeon-dependant and surgeon-independent factors [1]. Surgeon-dependant factors include the distraction, overcorrection, osteotomies, and correction of kyphosis [5, 6]. Surgeon-independent factors include type of curve, preexisting neurological deficit, approach, and type of instrumentation [1, 7]. The incidence of neurological injury is higher in syndromic, neuromuscular, and congenital scoliosis as opposed to the idiopathic scoliosis [1]. Of all neurological complications, the traction palsy of brachial plexus has been rarely reported. Isolated cases of brachial plexus injury have been reported with positioning and central line insertion but there have been no reports of brachial plexus palsy, primarily due to deformity correction [8-10]. Here, we present a case report of two cases who had post-operative brachial plexus palsy following deformity correction.
Case 1
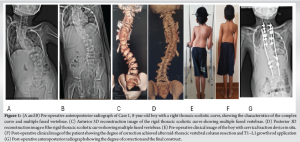
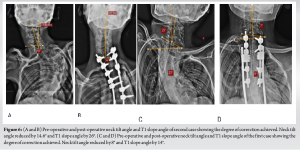
An 8-year-old otherwise healthy boy presented to us with a history of progressive painless deformity of spine since birth. On examination, the child had a right-sided shoulder imbalance, a right thoracic scoliotic curve with normal neurology, no limb length discrepancy, and no neurocutaneous markers. The child had a normal gait. On radiography and magnetic resonance imaging (MRI), there were multiple fused vertebrae. Cobb’s angle at presentation was 64° with a curve from T1 to L1, and the neck tilt angle at presentation was 15° with a T1 slope angle of 23°. With a plan of surgical correction later, the patient was initially managed with halo gravity traction for 4 weeks. Following this, he underwent mid-thoracic vertebral column resection and T1 to L1 growth rod application (Fig. 1). Post-operative Cobb’s angle was measured to be 37°, neck tilt angle reduced to 7° and T1 slope angle came down to 9°.
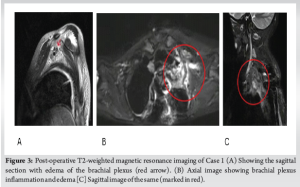
On post-operative day 1, the patient developed left-sided upper limb weakness (Fig. 2). Post-operative imaging showed no anomalies surrounding the fixation. Considering the presentation, we diagnosed him of Klumpke’s brachial plexus palsy and Horner’s syndrome. MRI of the brachial plexus showed edema around the brachial plexus and sympathetic chain on the left side (Fig. 3), and he was started on intravenous high-dose methylprednisolone therapy as per NASCIS guidelines [11]. The patient recovered completely in 4 weeks.

Case 2
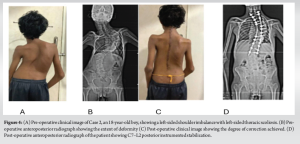
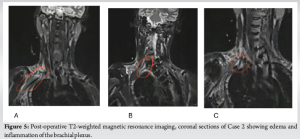
An 18-year-old male patient presented to us with painless progressive deformity of the back from the age of 6 years. On examination, head central with a neck tilt toward the right. He had a left-sided shoulder imbalance with left-sided thoracic scoliosis. He had no neurocutaneous markers no limb length discrepancy, normal gait, and neurology was normal. On imaging, he was diagnosed of severe rigid cervicothoracic scoliosis. Pre-operative operative Cobb’s angle was 90° with a curve from T1 to T12 and the patient had a neck tilt angle of 17.2° and the T1 slope was 55°. With a plan for surgery, he was managed initially with halo gravity traction for 4 weeks. Following this, the patient underwent corrective osteotomy at the apex, deformity correction, and C7–L2 posterior instrumented stabilization and fusion under neuromonitoring (Fig. 3). We achieved a 61°correction as per the Cobb’s angle measure. Post-operative neck tilt angle was reduced to 2.57 ° and T1 slope 29 °. On Post-operative day 1, the patient developed left upper limb weakness. MRI of brachial plexus showed edema around the right C4-5 and C5-6 nerve roots (Fig. 4). Patient started on intravenous steroids and on post-operative day 3, he started showing signs of recovery of right upper limb weakness. He had a complete neurological recovery in 3 weeks.
The pediatric spinal deformities are complex entities that require extensive planning before intervention. Especially in the case of syndromic, congenital or neuromuscular curves and those associated with a kyphosis are more likely to have post-operative neurological events [2, 12, 13]. The neurological injuries range from transient peripheral nerve palsy to complete spinal cord paralysis [14]. Incidence of perioperative peripheral nerve injury is approximated to 0.03–0.1% in surgical procedures [15]. The brachial plexus lies superficial in its course in the axilla and near bony prominences, therefore, is prone to injuries [8]. Being freely mobile and its close proximity to bony structures like the clavicle anteriorly, the first rib inferiorly, and the head of the humerus posterolaterally, it is more vulnerable to stretch and compression injuries [8]. Multiple isolated case reports in the literature report mechanisms for injury of brachial plexus, primarily due to positioning, stretching, compression, or direct piercing during surgery [10, 16-19]. Perioperative injury to brachial plexus has been attributed to different mechanisms. First reason seems to be the ischemia of the plexus of nerves. Ischemia leads to slowing of the conduction system of the peripheral nerves, further leading to demyelination and axonal damage. This is augmented by the phenomenon of reperfusion injury associated with increased blood flow following the ischemic insult [20]. Second mechanism is the stretch of the nerve that leads to disruption of the axonal flow. This happens when the nerve is stretched more than 5–15% of their resting lengths [21]. Other described mechanisms include peripheral nerve compression and direct insult to the nerve. Kamel and Barnette discuss the implications of positioning and its effect with respect to peripheral nerve injuries [20]. They propose that most causes of brachial plexus palsies are avoidable. In both our cases, patients underwent a complete posterior approach for correction of deformity. Adequate precautions were taken to avoid palsy due to positioning in both patients. Despite this, the patients had brachial plexus palsy. Therefore, we believe that the palsy is due to surgical correction maneuvers performed intraoperatively on the complex curves. There have been sparse instances reported wherein mechanical factors cause neurological injury. Smith et al. in their paper propose that over correction and over maneuvering of the spinal column in rigid scoliosis leads to neurological complications [22]. Moreover, the change of slope of the first rib after correction of the structural curve may have been instrumental in the compression of the brachial plexus intraoperatively resulting in the compression palsy of the brachial plexus as indicated by a significant reduction in T1 slope angle and neck tilt angle in both of our cases (Fig. 5) [23]. Second, on retrospective review of the cases and analysis of the surgical technique, considering the correction maneuvers applied, we observed that in both the patients, had a proximal rigid curve where the brachial plexus was relatively low lying. In addition, in the fused spine, the number of vertebrae proximal to the level of correction was lesser than a normal spine leading to a traction force on the brachial plexus during the correction. Although it requires further literature evidence, we believe this could be a probable cause of the traction palsy. We extended our fixation to T1 level in both cases. We believe that any form of deformity correction is attempted in the form of rod rotation or cantilever mechanism or compression distraction technique in these cases causes subsequent stretching of the nerve root of the brachial plexus resulting in inflammation and edema, which could have contributed to the transient deficits in our cases. (Fig. 6).
We also considered the theory that brachial plexus palsy could have occurred due the pre-operative use of halo gravity traction, as cases have been reported in literature. Although the incidence is known, most of these cases present with the palsy preoperatively, and it seems unlikely to have delayed presentations immediate postoperatively [24, 25]. In our cases, we have ruled out brachial plexus palsy following halo gravity traction by doing a clinical neurological examination preoperatively which was found to be normal in both cases. There have also been instances in literature wherein the brachial plexus palsy was attributed to cannulation of the internal jugular vein [10, 18]. In both our cases, we have ruled out the same using precautions such as USG-guided central insertion and careful monitoring. In the 2nd case, the central line was inserted on the right side, but the patient developed brachial plexus palsy on the left side. Although neuromonitoring was used in our cases, the patients developed post-operative neurological deficit. Hence, we are of the opinion that neuromonitoring, though believed to be a safe and effective method to prevent neurological deficits, is not always 100% sensitive [5, 26]. However, we also believe that specific lead placement overall cervical root dermatomes could have helped us detect the palsy intraoperatively. Both our patients made a complete recovery from the palsy and returned to normal functional status. Neurological complications associated with scoliosis have a good prognosis. About 87% of the patients make a complete recovery from any peripheral nerve injuries within 3–6 months of surgery [2, 4].
Brachial plexus traction palsy is a rare complication of deformity correction. Adequate pre-operative planning, proper identification of curves, precise selection of upper and lower instrumented vertebra, the use of adequate deformity reduction maneuvers are vital. We must also take precautions, to avoid excessive correction of neck tilt angle, while factoring in the complexity of the scoliotic curve. Patients with brachial plexus traction injury following deformity correction surgery generally have a good prognosis with medical management and the surgeon need not rush with a decision on re-exploration.
Brachial plexus traction palsy following correction of a complex spinal deformity could be due to mechanical causes such as over-distraction of proximal curve. Identification of proximal curve, measurement of neck tilt, and placement of neuromonitoring leads in appropriate level helps in the prevention of brachial plexus palsy following deformity correction.
References
- 1.Lykissas MG, Crawford AH, Jain VV. Complications of surgical treatment of pediatric spinal deformities. Orthop Clin North Am 2013;44:357-70. [Google Scholar]
- 2.Bivona LJ, France J, Daly-Seiler CS, Burton DC, Dolan LA, Seale JJ, et al. Spinal deformity surgery is accompanied by serious complications: Report from the morbidity and mortality database of the scoliosis research society from 2013 to 2020. Spine Deform 2022;10:1307-13. [Google Scholar]
- 3.Spinal Deformity Study Group, Diab M, Smith AR, Kuklo TR. Neural complications in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2007;32:2759-63. [Google Scholar]
- 4.Burton DC, Carlson BB, Place HM, Fuller JE, Blanke K, Cho R, et al. Results of the scoliosis research society morbidity and mortality database 2009-2012: A report from the morbidity and mortality committee. Spine Deform 2016;4:338-43. [Google Scholar]
- 5.Wilber RG, Thompson GH, Shaffer JW, Brown RH, Nash CL Jr. Postoperative neurological deficits in segmental spinal instrumentation. A study using spinal cord monitoring. J Bone Joint Surg Am 1984;66:1178-87. [Google Scholar]
- 6.MacEwen GD, Bunnell WP, Sriram K. Acute neurological complications in the treatment of scoliosis. A report of the scoliosis research society. J Bone Joint Surg Am 1975;57:404-8. [Google Scholar]
- 7.Asher M, Lai SM, Burton D, Manna B, Cooper A. Safety and efficacy of Isola instrumentation and arthrodesis for adolescent idiopathic scoliosis: Two- to 12-year follow-up. Spine (Phila Pa 1976) 2004;29:2013-23. [Google Scholar]
- 8.Uribe JS, Kolla J, Omar H, Dakwar E, Abel N, Mangar D, et al. Brachial plexus injury following spinal surgery: A review. J Neurosurg Spine 2010;13:552-8. [Google Scholar]
- 9.Ferrero-Manzanal F, Lax-Pérez R, López-Bernabé R, Betancourt-Bastidas JR, De Onzoño-Pérez AI. Traction injury of the brachial plexus confused with nerve injury due to interscalene brachial block: A case report. Int J Surg Case Rep 2016;27:78-82. [Google Scholar]
- 10.Nowak ŁR, Duda K, Mizianty M, Wilczek M, Bieda T. Horner syndrome after unsuccessful venous port implantation by cannulation of the right internal jugular vein. Anaesthesiol Intensive Ther 2015;47:336-8. [Google Scholar]
- 11.Thomas AX, Riviello JJ Jr., Davila-Williams D, Thomas SP, Erklauer JC, Bauer DF, et al. Pharmacologic and acute management of spinal cord injury in adults and children. Curr Treat Options Neurol 2022;24:285-304. [Google Scholar]
- 12.Leong JJ, Curtis M, Carter E, Cowan J, Lehovsky J. Risk of neurological injuries in spinal deformity surgery. Spine (Phila Pa 1976) 2016;41:1022-7. [Google Scholar]
- 13.Vitale MG, Moore DW, Matsumoto H, Emerson RG, Booker WA, Gomez JA, et al. Risk factors for spinal cord injury during surgery for spinal deformity. J Bone Joint Surg Am 2010;92:64-71. [Google Scholar]
- 14.Li J, Hu Z, Qian Z, Tang Z, Qiu Y, Zhu Z, et al. The prognosis and recovery of major postoperative neurological deficits after corrective surgery for scoliosis : An analysis of 65 cases at a single institution. Bone Joint J 2022;104-B:103-11. [Google Scholar]
- 15.Welch MB, Brummett CM, Welch TD, Tremper KK, Shanks AM, Guglani P, et al. Perioperative peripheral nerve injuries: A retrospective study of 380,680 cases during a 10-year period at a single institution. Anesthesiology 2009;111:490-7. [Google Scholar]
- 16.Schwartz DM, Drummond DS, Hahn M, Ecker ML, Dormans JP. Prevention of positional brachial plexopathy during surgical correction of scoliosis. J Spinal Disord 2000;13:178-82. [Google Scholar]
- 17.Goettler CE, Pryor JP, Reilly PM. Brachial plexopathy after prone positioning. Crit Care 2002;6:540-2. [Google Scholar]
- 18.Briscoe CE, Bushman JA, McDonald WI. Extensive neurological damage after cannulation of internal jugular vein. Br Med J 1974;1:314. [Google Scholar]
- 19.Raffan AW. Post-operative paralysis of the brachial plexus. Br Med J 1950;2:149. [Google Scholar]
- 20.Kamel I, Barnette R. Positioning patients for spine surgery: Avoiding uncommon position-related complications. World J Orthop 2014;5:425-43. [Google Scholar]
- 21.Wall EJ, Massie JB, Kwan MK, Rydevik BL, Myers RR, Garfin SR. Experimental stretch neuropathy. Changes in nerve conduction under tension. J Bone Joint Surg Br 1992;74:126-9. [Google Scholar]
- 22.Smith JS, Wang VY, Ames CP. Vertebral column resection for rigid spinal deformity. Neurosurgery 2008;63 3 Suppl:177-82. [Google Scholar]
- 23.Dahlin LB, Backman C, Düppe H, Saito H, Chemnitz A, Abul-Kasim K, et al. Compression of the lower trunk of the brachial plexus by a cervical rib in two adolescent girls: Case reports and surgical treatment. J Brachial Plex Peripher Nerve Inj 2009;4:14. [Google Scholar]
- 24.Seller K, Haas S, Raab P, Krauspe R, Wild A. Die präoperative halo-extension bei hochgradiger lähmungsskoliose [Preoperative halo-traction in severe paralytic scoliosis]. Z Orthop Ihre Grenzgeb 2005;143:539-43. [Google Scholar]
- 25.Qian BP, Qiu Y, Wang B. Brachial plexus palsy associated with halo traction before posterior correction in severe scoliosis. Stud Health Technol Inform 2006;123:538-42. [Google Scholar]
- 26.Labrom RD, Hoskins M, Reilly CW, Tredwell SJ, Wong PK. Clinical usefulness of somatosensory evoked potentials for detection of brachial plexopathy secondary to malpositioning in scoliosis surgery. Spine (Phila Pa 1976) 2005;30:2089-93. [Google Scholar]