Severe knee joint dislocations often require immediate closed reduction and duplex sonography, with subsequent prioritizing vascular and neurological repair before orthopedic treatment
Dr. Gero Knapp, Department of Trauma, Hand, and Reconstructive Surgery, University Hospital Giessen GmbH, Rudolf-Buchheim-Strasse 7, 35392 Giessen, Germany. E-mail: Gero.Knapp@chiru.med.uni-giessen.de
Introduction: Dislocations of the knee joint due to low-energy trauma following knee arthroplasty are very rare cases. However, when vascular involvement is present, it must be taken very seriously. This study aims to examine the clinical course, diagnostic approach, and surgical management of knee joint dislocation with vascular injury following low-energy trauma in a patient with a pre-existing knee arthroplasty.
Case Report: This case report details the instance of a 67-year-old female patient experiencing an anterior dislocation of the knee joint subsequent to a low-energy fall, occurring years after the surgical implantation of a knee joint prosthesis. Clinically and radiologically, an anterior dislocation of the knee joint accompanied by a rupture of the popliteal artery (PI/III segment) was confirmed. The involvement of the popliteal artery was evident in duplex sonography and computed tomography angiography conducted after closed reduction. The surgical intervention involved performing an end-to-end anastomosis of the popliteal artery, followed by the installation of a cemented rotating hinge knee endoprosthesis.
Conclusion: Severe knee joint dislocations often require immediate closed reduction and duplex sonography, potentially leading to emergency surgical intervention. Prioritizing vascular and neurological repair before orthopedic treatment is essential, with follow-up assessments for joint stability recommended.
Keywords: Total knee arthroplasty, dislocations, vascular rupture.
Total knee endoprostheses (total knee arthroplasty [TKA]) are among the most common orthopedic procedures in clinical practice [1]. Patient satisfaction is high, and more than 82% of the prostheses achieve a lifespan of 25 years [2]. Severe complications after TKA are rare with an incidence of <2.5% [3]. Prosthesis dislocation is one of the rarest complications following TKA. In primary care, tibiofemoral dislocation occurs in about 0.15–0.5% of all TKA while persisting pain demonstrates one of the most common complications in 12% of the cases [4, 5]. Anterior dislocations with vascular involvement following TKA are particularly rare. Only a few cases are described in the literature [4, 6, 7]. A review of Almoguera-Martinez et al. identified only 15 cases of anterior prosthetic dislocations of which only three included a vascular injury [4]. Especially, anterior knee joint dislocations caused by low-energy trauma are rare. A standardized treatment regimen, especially standardized guidelines, for anterior knee joint dislocations has therefore not yet been established. More common, posterior knee joint dislocations are observed following high-energy trauma. Various risk factors had been detected for knee joint dislocations after TKA including tibial component malalignment, polyethylene wear, extensor mechanism dysfunction, and flexion-extension gap mismatch [8, 9, 10]. There is some evidence that early diagnosis and prompt surgical treatment are crucial for an improved outcome [11]. Our case presents a 67-year-old female patient with an acute popliteal artery injury after a tibiofemoral dislocation in a primary TKA and aims to examine the clinical course, diagnostic approach, and surgical management of knee joint dislocation with vascular injury.
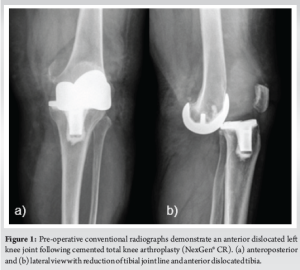
A 67-year-old female patient with an obese body mass index (BMI) (38.1 kg/m2) and a known history of hypertension presented to the interdisciplinary emergency department by ambulance. Upon initial examination in primary care, the patient presented with significant swelling and loss of mobility in the left knee joint. This followed an incident where the patient sustained a fall and twisted her knee while getting off a bicycle. The initial clinical assessment showed an absence of palpable pulses in the left popliteal, posterior tibial, and dorsalis pedis arteries. In addition, the left lower leg was noted to have a cold sensation upon palpation. Further body check examinations, including a neurological examination, presented neither anomaly. The initial X-ray of the left knee joint showed an anterior dislocation of the embedded knee TKA (NexGen® CR), which was implanted in 2013 (Fig. 1).
Performing short anesthetics, the patient was brought to the operating room for emergency closed repositioning. Intraoperative color-coded Doppler sonography revealed no signal of the left popliteal artery.
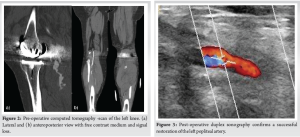
Following the closed reduction, angio-computed tomography (CT) confirmed the presence of a severe tear in the left popliteal artery, accompanied by active bleeding into the soft tissue located behind the knee joint (Fig. 2).
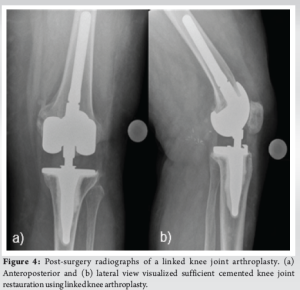
In addition, there was a lack of perfusion of the posterior tibial artery and fibular artery in the proximal half of the lower leg, resulting in a 1-vessel supply of the left lower leg through the anterior tibial artery. Upon evaluation of the imaging and clinical findings, vascular surgery was conducted the same day with the knee joint appearing stable in all planes upon clinical examination. The damaged sections of the popliteal artery were excised and the vessel was reconstructed using an end-to-end anastomosis technique, without the need for a graft insert (Fig. 3). Post-operatively, the patient was immobilized with a hard-frame-range of motion (ROM) orthosis (DonJoy®, Enovis Corporation, Delaware, United States of America) with a ROM of 0/0/90° for 3 weeks. A repeat CT scan of the left knee joint showed peri-prosthetic detachment of two cortical fragments on the medial femoral condyle (4 × 6 mm and 20 × 22 mm) and an intact lateral condyle. At the 1-month follow-up, she had only attended physical therapy twice, was unable to bear weight on the leg, and had a ROM of 0/0/90°. Until the 2-month follow-up appointment partial mobilization was performed with a maximum of 20 kg of weight-bearing and the hard-frame-ROM orthosis. The patient continued physiotherapy and was able to increase her ROM to 0/0/100°. However, there was subjective and objective mediolateral 3rd° instability of the knee joint in extension and she felt unstable without orthosis, so at the patient’s request, an indication for revision surgery to a higher degree of coupling was made. An uncomplicated revision of the bicompartmental surface replacement prosthesis to a cemented, coupled rotating-hinge prosthesis (NexGen® Complete Knee Solution, Zimmer Biomet, Indiana, United States of America) was conducted 5 months after the fall and the vascular surgery. Post-operative radiographic examination showed satisfactory prosthesis placement and proper repositioning results (Fig. 4). Initially, follow-up appointments were conducted every 6–8 weeks, and then adjusted to an as-needed basis. In the 1st weeks the patient experienced paresthesia in the distribution area of the peroneal nerve, without any motor deficits. A magnetic resonance imaging revealed spinal canal stenosis from L1 to L5. The neurological symptoms are well managed conservatively with Gabapentin. Besides that the patient is overall very satisfied, experiencing no instability, with a ROM of 0/0/110° (Flex./Ext.) and intact peripheral blood flow, motor, and sensory function. Present treatment includes physical therapy, manual lymphatic drainage, and custom insoles. At present, the patient attends quarterly appointments with a primary focus on managing osteoarthritis in the right knee.
Cases of anterior tibiofemoral dislocations in the presence of a TKA with vascular involvement are very rare. There are a few such cases described in the literature [4, 6, 7]. The first cases of dislocated knee prostheses were described by Insall et al. in 1979 [12]. However, all dislocated knees following TKA were posterior dislocations. In 1997, anterior dislocations were first described by Wang and Wang [13]. Certain factors, such as obesity and a high BMI, are known to elevate the risk of such events. Clinical evidence suggests that in cases of TKA, a higher BMI is associated with an elevated risk of joint instability and prosthetic failure due to the increased biomechanical load [14]. Furthermore, there was a vascular involvement with the rupture of the left popliteal artery in the present case. The risk of vascular injury in knee dislocations without prosthesis is 30–60% [15]. Following a knee joint arthroplasty, the overall incidence is only about 5% [16]. In terms of obesity, the risk of a vascular injury requiring an intervention with a tibiofemoral dislocation is about 1.9% higher in obese patients and 5.7% higher in morbidly obese patients compared to the general population [17]. Also in this patient, classified as obese with a BMI of 38.1 kg/m², obesity likely contributed significantly to the biomechanical load to the knee joint and the vascular involvement. Popliteal artery injuries after knee dislocations are documented as being potentially limb-threatening in the literature, emphasizing the importance of rapid diagnosis and intervention within 6–8 h to prevent ischemic complications [18-20]. In this case, the absence of palpable pulses and the cold sensation in the lower leg were critical indicators, prompting urgent surgical exploration. The primary management of this case involved a surgical repair of the injured popliteal artery using an end-to-end anastomosis, a technique particularly suited for short-segment arterial injuries as it directly reconnects the vessel ends without the need for grafting. Post-operatively, the knee joint was initially immobilized with a hard-frame-ROM orthosis to protect the vascular repair and support joint stability. The ROM was restricted to 0°/0°/90° to safeguard the surgical outcome and prevent vascular compromise. Despite the successful vascular and orthopedic management, the patient exhibited mediolateral instability, ultimately necessitating revision surgery. This highlights the challenge of achieving long-term joint stability following TKA dislocation in patients with complex vascular injuries. Revision to a higher degree of coupling, like in our case with rotating-hinge prosthesis, has shown to be effective, providing greater stability than traditional TKA components [21, 22]. The case emphasizes the importance of a multidisciplinary approach in managing complex knee dislocations with vascular injuries, involving orthopedic, vascular, and physical therapy teams to optimize outcomes. Regular follow-up and rehabilitation are crucial, especially for patients with additional risk factors such as obesity and hypertension [14]. This comprehensive approach can improve long-term function and quality of life for patients with similar injuries. However, due to the rarity of these cases, there is currently no evidence-based treatment protocol. The treatment of these cases is based on individual considerations and experiences, as outlined in case reports.
In cases of anterior tibiofemoral dislocation in the presence of a TKA, prompt closed reduction with immediate CT angiography and vascular surgery consultation is essential. Throughout the patient’s care, good interdisciplinary collaboration between orthopedic and vascular surgery teams is of great importance. In instances of instability, as observed in this case, the recommendation is to proceed with prosthesis replacement utilizing a prosthesis with a higher degree of coupling.
This article presents the authors’ clinical experience and the decision-making process that led to the successful treatment of a traumatic knee joint dislocation with popliteal artery rupture followed by knee joint arthroplasty.
References
- 1.Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 2018;100:1455-60. [Google Scholar]
- 2.Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019;393:655-63. Erratum in: Lancet 2019;393:876. [Google Scholar]
- 3.Ma LL, Yu XR, Weng XS, Lin J, Jin J, Qian WW, et al. Possible risk factors for severe complications occurring after primary total knee arthroplasty. Chin Med Sci J 2022;37:303-8. [Google Scholar]
- 4.Almoguera-Martinez A, Godinho-Soares C, Calcedo Bernal V, Pareja Esteban JA, Garcia-Lopez M, Plasencia Arriba MÁ. Anterior tibiofemoral dislocation after total knee arthroplasty: A case report and literature review. Chin J Traumatol 2022;25:237-41. [Google Scholar]
- 5.Tian M, Li Z, Chen X, Wu Q, Shi H, Zhu Y, et al. Prevalence and predictors of chronic pain with two-year follow-up after knee arthroplasty. J Pain Res 2022;15:1091-5. [Google Scholar]
- 6.Conti A, Camarda L, Mannino S, Milici L, D’Arienzo M. Anterior dislocation in a total knee arthroplasty: A case report and literature review. J Orthop 2014;12:S130-2. [Google Scholar]
- 7.Constantinescu D, Pavlis W, Berge DV, Barnhill S, Geller J, Vilella FE. Anterior prosthetic knee dislocation with acute vascular injury: A case report. Ann Med Surg (Lond) 2022;75:103425. [Google Scholar]
- 8.Galinat BJ, Vernace JV, Booth RE Jr., Rothman RH. Dislocation of the posterior stabilized total knee arthroplasty. A report of two cases. J Arthroplasty 1988;3:363-7. [Google Scholar]
- 9.Gebhard JS, Kilgus DJ. Dislocation of a posterior stabilized total knee prosthesis. A report of two cases. Clin Orthop Relat Res 1990;254:225-9. [Google Scholar]
- 10.Bargren JH. Total knee dislocation due to rotatory malalignment of tibial component: A case report. Clin Orthop Relat Res 1980;147:271-4. [Google Scholar]
- 11.Giustra F, Bosco F, Masoni V, Capella M, Cacciola G, Risitano S, et al. Irreducible knee dislocation: Improved clinical outcomes of open and arthroscopic surgical treatment. A systematic review of the literature. Eur J Orthop Surg Traumatol 2024;34:735-45. [Google Scholar]
- 12.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am 1979;61:173-80. [Google Scholar]
- 13.Wang CJ, Wang HE. Dislocation of total knee arthroplasty. A report of 6 cases with 2 patterns of instability. Acta Orthop Scand 1997;68:282-5. [Google Scholar]
- 14.Foran JR, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg Am 2004;86:1609-15. [Google Scholar]
- 15.Addevico F, Nucci AM, Rosati M, Poggetti A, Scaglione M. Traumatic anterior dislocation of a prosthetic knee, from trauma to delayed onset of vascular injury. Arthroplast Today 2018;4:407-10. [Google Scholar]
- 16.Rouquette L, Erivan R, Pereira B, Boisgard S, Descamps S, Villatte G. Tibiofemoral dislocation after primary total knee arthroplasty: A systematic review. Int Orthop 2019;43:1599-609. [Google Scholar]
- 17.Johnson JP, Kleiner J, Klinge SA, McClure PK, Hayda RA, Born CT. Increased incidence of vascular injury in obese patients with knee dislocations. J Orthop Trauma 2018;32:82-7. [Google Scholar]
- 18.Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am 1977;59:236-9. [Google Scholar]
- 19.Azar FM, Brandt JC, Miller RH 3rd, Phillips BB. Ultra-low-velocity knee dislocations. Am J Sports Med 2011;39:2170-4. [Google Scholar]
- 20.Frassica FJ, Sim FH, Staeheli JW, Pairolero PC. Dislocation of the knee. Clin Orthop Relat Res 1991;263:200-5. [Google Scholar]
- 21.Springer BD, Hanssen AD, Sim FH, Lewallen DG. The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res 2001;392:283-91. [Google Scholar]
- 22.Röhner E, Benad K, Zippelius T, Kloss N, Jacob B, Kirschberg J, et al. Good clinical and radiological results of total knee arthroplasty using varus valgus constrained or rotating hinge implants in ligamentous laxity. Knee Surg Sports Traumatol Arthrosc 2019;27:1665-70. [Google Scholar]