Baastrup’s disease has an uncommon presentation presenting with cauda equina syndrome. Early diagnosis and prompt surgical decompression are critical to improving neurological outcomes and preventing long-term complications
Dr. Nitin Pothare, Assistant Professor,Department of Orthopedic Surgery, N.K.P. Salve Institute of Medical Sciences and Research Centre and Lata Mangeshkar Hospital, Nagpur, Maharashtra, India. E-mail: nitinpothare@gmail.com
Introduction: Baastrup’s disease, more commonly known as kissing spines, has been implicated as a cause for low back pain and extension of the synovial cavity to the intraspinal space, resulting in extradural compression. However, this is the first report in the literature of a cyst responsible for cauda equina syndrome.
Case Report: We present a case of a 60-year-old male having an epidural synovial cyst as an extension of Baastrup’s disease, causing cauda equina syndrome, and to review the relevant literature. Radiographs were normal, and magnetic resonance imaging showed the presence of a cyst in the posterior epidural space at the L4-L5 level causing dural compression. Moreover, the cysts were excised, and spinal decompression was performed. The patient had good relief of symptoms.
Conclusion: This case highlights the importance of considering Baastrup’s disease as a potential, though uncommon, cause of neurological deficits in patients presenting with cauda equina syndrome. Early diagnosis and prompt surgical decompression are critical to improving neurological outcomes and preventing long-term complications.
Keywords: Baastrup’s disease, cauda equina, epidural cyst.
Baastrup’s disease, also known as lumbar interspinous bursitis or “kissing spine syndrome,” is a degenerative spinal condition primarily affecting the lumbar region, most commonly at the L4-L5 level. First formally described by Christian Ingerslev Baastrup in 1933 [1-3]. Baastrup’s disease is a well-recognized cause of low back pain, particularly in the elderly. Studies suggest that it may affect up to 81% of individuals over the age of 80 [4]. Although its prevalence in the general population remains unclear. Despite its relative frequency, Baastrup’s disease is often underdiagnosed, either due to a lack of awareness or limitations in imaging techniques. This condition occurs when adjacent spinous processes come into close contact due to excessive lumbar lordosis, leading to the degeneration of interspinous ligaments and subsequent inflammation. Magnetic resonance (MR) findings include edema-hypointense streak on T1 and a hyperintense streak on T2 between the spinous processes, sclerosis-hypointense streak on T2 between the spinous processes, flattening, bursitis, and midline epidural fibrosis [5,6]. This case report presents an atypical manifestation of Baastrup’s disease, where the patient developed cauda equina compression, highlighting the need for careful diagnosis and tailored management strategies.
A 60-year-old male patient with no comorbidity came to our outpatient department complaining of acute onset of back pain radiating to both lower limbs for 8 months. He was managed with painkillers and symptomatic management. There was a history of progressive neurogenic claudication for 6 months, 3 weeks of worsening low back radiating pain to both lower extremities (L5 distribution), and 1 week of voiding difficulty. The patient had pain on movements. The patient had difficulty performing his daily activities and had difficulty earning his livelihood due to the complaints.
Clinical findings
On examination, tenderness was present at L4-5 level, Paraspinal muscle spasm was present, Power in bilateral extensor hallucis longus (EHL) and flexor hallucis longus (FHL) was grade 1, bilateral ankle reflex was absent, sensation were normal, planters were flexors, he also developed acute bladder dysfunction with perigenital numbness. Acute urine retention was present with pre-void bladder ultrasound (800 mL), rectal sphincter tone was intact. These findings were consistent with the clinical diagnosis of a cauda equina syndrome.
Diagnostic assessment and interpretation
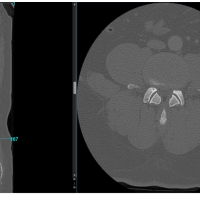
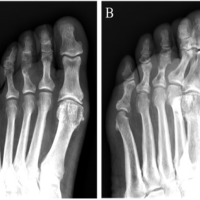
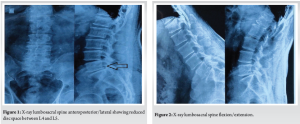
For diagnosis of the condition X-ray lumbosacral spine (LS) revealed degenerative changes involving the LS, along with articulation of spinous processes at L4-5 (Fig. 1 and 2), which was confirmed on computed tomography (CT) LS (Fig. 3). MR imaging LS shows at L4-5 level, posterior midline extradural cyst with a broad-based disc bulge resulting in thecal sac and equine nerve root compression (Fig. 4).

Intervention
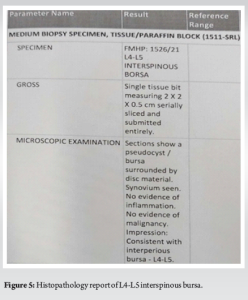
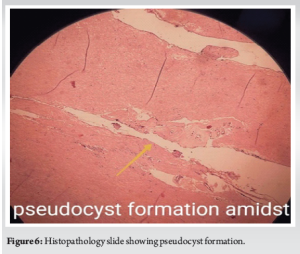
Patient underwent an L4 laminectomy, L4-L5 discectomy using METRX TUBULAR system with working sheath 22×5. The cavity was lined with a thick fibrous wall and contained an hourglass-shaped communication through the midline cleft of the ligamentum flavum. The intraspinal cyst had a thin wall and was filled with fluid, which was compressing the dural sac. The bursa was excised and sent for histopathological examination (Fig. 5,6). Over-the-top decompression was performed, resulting in thecal sac decompression and bilateral release of the nerve roots.
Post-operative protocol
The patient was mobilized from the next day. Analgesics and antibiotics were given as per protocol. The patient was given a lumbo-sacral belt and was advised against forward bending and lifting heavy weights. The patient was discharged on post-operative day 4.
Outcome
Following decompression, the patient showed substantial neurological improvement. She was discharged 4 days post-intervention, experiencing no back or lower limb pain, with enhanced saddle sensation and bladder function, increased motor strength in her right leg, and satisfactory mobility. At her 1-year follow-up, the patient remains well and neurologically intact.
The cause of pain associated with “kissing spines” remains a topic of debate. It is typically mechanical in nature and often increases with spinal extension. Early reports suggested that relief from pain could be achieved through injections of local anesthetic agents [7]. The localized episodic back pain has been attributed to significant osteoarthritic bone erosion in the adjacent spinous processes, which are equipped with sensory nerve endings. Macnab proposed that “kissing spines” usually occur alongside an unstable disc segment, suggesting that it is the associated disc degeneration, rather than the bony contact of the spinous processes, that leads to the patient’s symptoms [8]. In addition, diffuse fatty replacement of the paraspinal muscles has been described in these patients and may play a role in the etiology of pain in Baastrup’s disease [9]. Bywaters and Evans conducted autopsy studies on 152 lumbar spines to investigate the prevalence of Baastrup’s disease [10]. They observed pseudojoints, chondroid metaplasia, enchondral ossification, and significant osteoarthritic bone erosion with eburnation in their findings. They introduced a “bursal index” to identify spines at risk for developing this condition, with prevalence ranging from 6.2% to 22.1%. Spines with a lower bursal index were found to be more predisposed to the development of Baastrup’s disease [11]. Hamlin reported increased radiotracer uptake on single-photon emission CT scans in lesions associated with this condition. The diversity of theories regarding symptom sources has led to various treatment perspectives. In one early study, 10 patients experienced improvement after undergoing surgical excision of the spinous processes [12]. However, a later study involving 64 patients who had partial or total surgical excision of the lumbar spinous processes revealed that surgery does not always alleviate pain [13]. This study concluded that other pathological changes, such as disc degeneration, congenital malformations like spina bifida occulta, and spinal stenosis, could be responsible for the patients’ complaints. To date, there have been no reports of lumbar Baastrup’s disease causing symptomatic spinal canal stenosis. However, this is the first case report documenting Baastrup’s disease resulting in cyst formation, leading to epidural extension and compression of neural elements, culminating in cauda equina syndrome.
Baastrup’s disease is usually linked to chronic back pain, but it can also, though rarely, present as cauda equina syndrome, a serious condition that requires urgent intervention. This case underlines the importance of considering Baastrup’s disease as a potential, albeit uncommon, cause of neurological deficits in patients with cauda equina syndrome. Early diagnosis and prompt surgical decompression are crucial for improving neurological outcomes and preventing long-term complications. By being aware of this rare presentation, clinicians can make timely and accurate diagnoses, ultimately enhancing patient care and outcomes.
Baastrup’s disease, typically associated with chronic mechanical back pain, can present with rare but severe neurological complications such as cauda equina syndrome. This case underscores the importance of recognizing atypical manifestations of Baastrup’s disease, as timely diagnosis and urgent surgical decompression are crucial for preventing permanent neurological deficits. Clinicians should consider Baastrup’s disease as a potential cause of spinal canal stenosis and neural compression, particularly in patients with progressive neurological symptoms.
References
- 1.Jang EC, Song KS, Lee HJ, Kim JY, Yang JJ. Posterior epidural fibrotic mass associated with Baastrup’s disease. Eur Spine J 2010;19 Suppl 2:S165-8. [Google Scholar | PubMed]
- 2.Rajasekaran S, Pithwa YK. Baastrup’s disease as a cause of neurogenic claudication: A case report. Spine (Phila Pa 1976) 2003;28:E273-5. [Google Scholar | PubMed]
- 3.Baastrup CL. On the spinous processes of the lumbar vertebrae and the soft tissue between them and on pathological changes in the region. Acta Radiol 1933;14:52-4. [Google Scholar | PubMed]
- 4.Mitra R, Ghazi U, Kirpalani D, Cheng I. Interspinous ligament steroid injections for the management of Baastrup’s disease: A case report. Arch Phys Med Rehabil 2007;88:1353-6. [Google Scholar | PubMed]
- 5.Haig AJ, Harris A, Quint DJ. Baastrup’s disease correlating with diffuse lumbar paraspinal atrophy: A case report. Arch Phys Med Rehabil 2001;82:250-2. [Google Scholar | PubMed]
- 6.Sartoris DJ, Resnick D, Tyson R, Haghighi P. Age-related alterations in the vertebral spinous processes and intervening soft tissues: Radiologic-pathologic correlation. Am J Roentgenol 1985;145:1025-30. [Google Scholar | PubMed]
- 7.Filippiadis DK, Mazioti A, Argentos S, Anselmetti G, Papakonstantinou O, Kelekis N, et al. Baastrup’s disease (kissing spines syndrome): A pictorial review. Insights Imaging 2015;6:123-8. [Google Scholar | PubMed]
- 8.Hatgis J, Granville M, Jacobson RE. Baastrup’s disease, interspinal bursitis, and dorsal epidural cysts: Radiologic evaluation and impact on treatment options. Cureus 2017;9:e1449. [Google Scholar | PubMed]
- 9.Schwartz RH, Urits I, Viswanath O. Extensive degeneration of vertebral body leading to Baastrup’s disease: A radiographic review of an image. Pain Ther 2019;8:285-7. [Google Scholar | PubMed]
- 10.Bywaters EG, Evans S. The lumbar interspinous bursae and Baastrup’s syndrome. An autopsy study. Rheumatol Int 1982;2:87-96. [Google Scholar | PubMed]
- 11.Hamlin LM, Delaplain CB. Bone SPECT in Baastrup’s disease. Clin Nucl Med 1994;19:640-1. [Google Scholar | PubMed]
- 12.Macnab I. Backache. Baltimore: Williams and Wilkins; 1977. [Google Scholar | PubMed]
- 13.Franck S. Surgical treatment of intraspinal osteoarthrosis (kissing spine). Acta Orthop Scand 1944;14:127-52. [Google Scholar | PubMed]