Anterocentral portal offers safer access with better visibility and fewer tendon injuries than the medial midline portal in ankle arthroscopy.
Dr. Mayank Pratap Singh, Shiv vihar colony datia, Madhya Pradesh, India. E-mail: mayanksingh686@gmail.com
Introduction: The medial midline portal and anterocentral both are not standard portals for ankle arthroscopy, but they provide a wide field of vision.
Aims: The aim of this study was to compare anatomical safety between medial midline and anterocentral portal in arthroscopy in respect to the least injury to adjacent structures.
Materials and Methods: 20 cadaveric ankles were dissected and related anatomical structures were measured from anterocentral and medial midline portals.
Results: The dorsalis pedis artery (DPA) was at a mean distance of 10.08 mm, the deep peroneal nerve was at 16.20 mm, the tibialis anterior tendon was at 2.41 mm, and the extensor hallucis longus (EHL) tendon was at 2.62 mm from the medial midline portal. The EHL tendon was injured in two specimens during portal placement. The anterocentral portal was placed at a mean distance of 2.38 mm from the DPA, 7.09 mm from the superficial peroneal nerve, and 4.12 mm from the deep peroneal nerve.
Conclusion: Our study demonstrated that the anterocentral portal is safer than the medial midline portal for ankle arthroscopy. While there is a high risk of tendon injury in the medial midline portal.
Keywords: Anatomy of ankle, ankle arthroscopy, anterocentral portal, medial midline portal.
Arthroscopy simply means the inspection of the interior of a synovial joint [1]. Arthroscopy of the ankle joint has increased due to symptoms and complaints are very common, so arthroscopy is widely used for treatment and diagnosis of ankle pathologies [2,3,4,5].
For ankle arthroscopy, several arthroscopic portals have been utilized; Anteromedial and Anterolateral are most commonly used and allow access to all sides of the joint. The anterocentral portal and medial midline portal [7] might also be used. The anterocentral portal is a good choice to see both sides of the joint and provide a wide field of vision.
The overall reported complication rates for this procedure have ranged from 3.4% to 10.3% [6,7,8,9,10,11]. Neurovascular injuries are the most common, which ranged from 0.04% to 4.8% [12], almost half of the overall reported complications.
Anatomical variations of the structures are commonly seen in terms of distances and course around the ankle joint [13,14]. These anatomical structures (neurovascular and tendinous) may be injured during ankle arthroscopy through any portal.
We used 20 ankle specimens from cadavers. These specimens were dissected and studied for the anatomical placement of structures around portals.
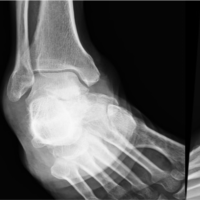
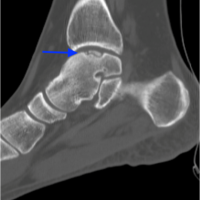
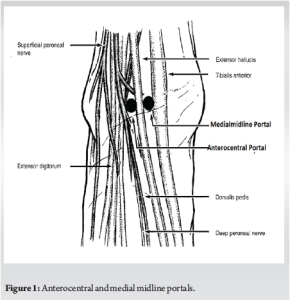
We identified surface landmarks (medial malleolus, lateral malleolus, extensor hallucis longus [EHL] and tibialis anterior muscle) and we marked each anatomical landmark (Fig. 1).
The tendons over the ankle were palpated to determine the site of entry and 20 mL of saline was injected into the joint to distend it by using a needle. On both sites, the portal was made using a 5 mm longitudinal skin incision and dissection was done deep to the joint without damaging the structures. Then 4 mm arthroscope was inserted and replaced with a short stick (Fig. 2).

Then the skin and subcutaneous fat were dissected from the underlying fascia for visualization of the muscle tendons, nerves, and vessels around the joint. We identified the anatomical structures adjacent to the portal. Moreover, we measured the distance of different structures from the portal. Where there were two branches of one structure, the distance from the portal to the nearest branch was measured.
Two portals were studied
- Medial midline portal (between tibialis anterior tendon and EHL tendon): The mean distance of dorsalis pedis artery (DPA), superficial peroneal nerve, tibialis anterior tendon, and EHL tendon was measured.
- Anterocentral (lateral to EHL): Measured mean distance of the DPA, Superficial peroneal nerve, and deep peroneal nerve.
Digital vernier caliper was used to measure the distance from the portal to the anatomical structures.
In this study, we obtained the data after dissection of 20 ankle specimens.
The mean distance from medial midline portal to DPA was 10.08 ± 3.16 mm (4.0–14.4), superficial peroneal nerve was 16.20 ± 4.92 mm (7.0–24.3), Tibialis anterior tendon was 2.41 ± 2.08 mm (0.6–8.4) and EHL tendon was 2.62 mm ± 1.93 (0–5.9). The EHL tendon laceration was encountered in two specimens Table 1.
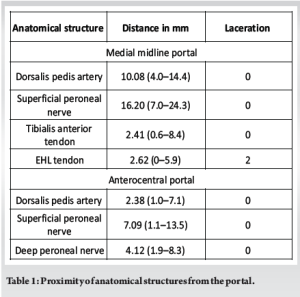
The anterocentral portal was at a mean distance of 2.38 ± 1.75 mm (1.0–7.1) from the DPA, 7.09 ± 3.84 mm (1.1–13.5) from the superficial peroneal nerve, and 4.12 ± 1.63 mm (1.9–8.3) from the deep peroneal nerve.
The present study was aimed at studying the extra-articular anatomy of the ankle region with respect to the medial midline and anterocentral portals. The distance was measured between each of the respective portals to the adjacent neurovascular and tendinous structures.
Medial midline portal
In this study, a mean distance between the medial midline portal and the DPA was 10.08 mm (range 4.0–14.4 mm), between superficial nerve 16.20 mm (range 7.0–24.3 mm), between tibialis anterior tendon was 2.41 mm (range 0.6–8.4 mm) and between EHL tendon was 2.62 (range 00–5.9 mm). Buckingham et al. [15] found a mean distance of 11 mm (range 5–15 mm) from the DPA.
Golano et al. [16] stated that this portal gives an intra-articular view similar to that by anterocentral portal but with lower chances of lesion to vital structures. Bharambe et al. [17] found the mean distance for DPA and deep peroneal nerve was 1.7 (range being 1–2 mm).
Anterocentral portal
In this study, the mean distance between the portal and the DPA was 2.38 mm (range 1.0–7.1 mm), between the superficial peroneal nerve was 7.09 mm (range 1.1–13.5 mm), and between the deep peroneal nerve was 4.12 mm (range 1.9–8.3 mm). Buckingham et al. [15] reported the mean distance to be 0.7 (range 0–5) from the DPA and 1.1 (range 0–5) in case of the deep peroneal nerve. In their study, the superficial peroneal nerve was lacerated in three cases and in one case, it lacerated the deep peroneal nerve.
Golano et al. [16] discouraged due to the high associated risk of injury to the superficial peroneal nerve superficially and the deep peroneal nerve and the DPA on the deeper plane. They stated that any associated variations of the artery may also lead to vascular lesions.
Bharambe et al. [17] found the average distance from the portal to the DPA and deep peroneal nerve was 1.4 mm. Feiwell and Frey [18] found the average distance of this portal from the neurovascular bundle to be 3.3 mm (range, 0–10 mm). In one case, the arthroscope penetrated and in 4 cases was related to the neurovascular bundle.
Stotter et al. [19] concluded that the anterocentral portal in ankle arthroscopy is safe with a low number of neurovascular injuries and can be recommended as a standard portal.
Strengths and limitations
The principal strength of this study lies in its direct anatomical evaluation using cadaveric specimens, which provides accurate and objective measurements of the proximity of critical neurovascular and tendinous structures to the medial midline and anterocentral portals. By conducting a comparative assessment between these two less commonly used arthroscopic portals, the study contributes valuable data that may aid in minimizing complications during ankle arthroscopy. Moreover, the use of consistent methodology across specimens enhances the reliability of the findings. However, certain limitations must be acknowledged. The cadaveric nature of the specimens does not account for the dynamic anatomical shifts or physiological responses observed in live patients, such as tissue elasticity or vascular pulsatility. The relatively small sample size (n = 20) may also limit the generalizability of the results. In addition, demographic details, such as age, sex, or comorbidities of the cadavers were not considered, which might influence anatomical variability. Finally, variations in portal placement technique by different surgeons were not simulated, which may affect external applicability.
To conclude between medial midline and anterocentral portals, the Anterocentral safer than the medial midline portal. The EHL tendon injury was encountered in two specimens during portal placement.
The anterocentral portal provides better joint visibility and avoids frequent portal changes during the procedure.
Surgeon should be aware of anatomy and anatomical variations of structures related to the ankle, to minimize complications of ankle arthroscopy.
Surgeons must be aware of the anatomical proximity of neurovascular and tendinous structures while choosing arthroscopic portals. The anterocentral portal, although traditionally underused, may offer better safety and visibility than the medial midline portal with minimal tendon risk.
References
- 1.Jackson RW. From the scalpel to the scope: The history of arthroscopy. Proc (Bayl Univ Med Cent) 1996;9:77-9. [Google Scholar | PubMed]
- 2.Andrews JR, Previte WJ, Carson WG. Arthroscopy of the ankle: Technique and normal anatomy. Foot Ankle 1985;6:29-33. [Google Scholar | PubMed]
- 3.Barber FA, Britt BT, Ratliff HW, Sutker AN. Arthroscopic surgery of the ankle. Orthop Rev 1988;17:446-51. [Google Scholar | PubMed]
- 4.Dias S, Lewis TL, Alkhalfan Y, Ahluwalia R, Ray R. Current concepts in the surgical management of chronic ankle lateral ligament instability. J Orthop 2022;33:87-94. [Google Scholar | PubMed]
- 5.Shimozono Y, Seow D, Kennedy JG, Stone JW. Ankle arthroscopic surgery. Sports Med Arthrosc Rev 2018;26:190-5. [Google Scholar | PubMed]
- 6.Yammine K, Assi C. Neurovascular and tendon injuries due to ankle arthroscopy portals: A meta-analysis of interventional cadaveric studies. Surg Radiol Anat 2018;40:489-97. [Google Scholar | PubMed]
- 7.Barber FA, Click J, Britt BT. Complications of ankle arthroscopy. Foot Ankle 1990 Apr;10(5):263-6. [Google Scholar | PubMed]
- 8.Arshad Z, Aslam A, Al Shdefat S, Khan R, Jamil O, Bhatia M. Complications following ankle arthroscopy. Bone Joint J 2023;105-B:239-46. [Google Scholar | PubMed]
- 9.Zekry M, Shahban SA, El Gamal T, Platt S. A literature review of the complications following anterior and posterior ankle arthroscopy. Foot Ankle Surg 2019;25:553-8. [Google Scholar | PubMed]
- 10.Lamy C, Steinstra JJ. Complications in ankle arthroscopy. Clin Podiatr Med Surg 1994;11:523-39.. [Google Scholar | PubMed]
- 11.Gramajo F, Toledo I, Vázquez L, Masquijo I, Masquijo J. Ankle arthroscopy in children and adolescents: Analysis of indications and complications. Rev Mex Ortop Ped 2021;23:1-3. [Google Scholar | PubMed]
- 12.Dos Santos TF, Matos E Dinato MC. Vascular complication after anterior ankle arthroscopy: Case report. Sci J Foot Ankle 2019;13:87-90. [Google Scholar | PubMed]
- 13.Parikh S, Dawe E, Lee C, Whitehead-Clarke T, Smith C, Bendall S. A cadaveric study showing the anatomical variations in the branches of the dorsalis pedis artery at the level of the ankle joint and its clinical implication in ankle arthroscopy. Ann R Coll Surg Engl 2017;99:286-8. [Google Scholar | PubMed]
- 14.Jeon A, Seo CM, Lee JH, Han SH. The distribution pattern of the neurovascular structures for anterior ankle arthroscopy to minimize structural injury: Anatomical study. Bio Med Res Int 2018;2018:3421985. [Google Scholar | PubMed]
- 15.Buckingham RA, Winson IG, Kelly AJ. An anatomical study of a new portal for ankle arthroscopy. J Bone Joint Surg Br 1997;79:650-2. [Google Scholar | PubMed]
- 16.Golano P, Vega J, Pérez-Carro L, Gotzens V. Ankle anatomy for the arthroscopist. Part I: The portals. Foot Ankle Clin 2006;11:253-73,v. [Google Scholar | PubMed]
- 17.Vaishaly BK, Amol SA, Dinesh PK, Sumedha C. Anatomical study of the ankle joint in relation to the anterior, the posterior and the (new) medial arthroscopic portals: A cadaveric study. Int J Cur Res Rev 2017;9:21-9. [Google Scholar | PubMed]
- 18.Feiwell LA, Frey C. Anatomic study of arthroscopic portal sites of the ankle. Foot Ankle 1993;14:142-7. [Google Scholar | PubMed]
- 19.Stotter C, Klestil T, Chemelli A, Naderi V, Nehrer S, Reuter P. Anterocentral portal in ankle arthroscopy. Foot Ankle Int 2020;41:1133-42 [Google Scholar | PubMed]