Significantly displaced extraarticular fractures of the glenoid neck and lateral column require surgical fixation which gives excellent clinical and functional results.
Dr. Dhruva Angachekar, Department of Orthopedics, Vedantaa Institute of Medical Sciences, Dahanu, Maharashtra, India. E-mail: drdhruva55@gmail.com
Introduction: Since traumatic injuries to the scapula and scapulothoracic articulation are rare, they have not been extensively covered in the literature. According to reports, arthrosis, rotator cuff dysfunction, scapulothoracic dyskinesis, and impingement pain all contributed to decreased shoulder function after nonsurgical therapy. In addition, it was noted that surgical intervention for scapular fractures produced better results and a higher functional recovery.
Case Report: A 51-year-old female presented to our emergency department with a history of a fall of a heavy object over her right shoulder. A 3D computed tomography scan of the right shoulder was performed, and it revealed an extraarticular fracture of the lateral column with significant displacement and a glenopolar angle of >40° along with a scapular spine fracture. We decided to fix the fracture using 3.5 mm contoured reconstruction plates through the modified Judet approach. The patient had good clinical function and radiological union at 8 months post-surgery.
Conclusion: The modified Judet approach in the open reduction and fixation offers a great exposure of the glenoid neck and lateral column fractures for fixation while causing minimal morbidity and good functional results.
Keywords: Scapula fracture, modified Iudet approach, scapula lateral column fracture.
Since traumatic injuries to the scapula and scapulothoracic articulation are rare, they have not been extensively covered in the literature. Scapular fractures account for 1% of all fractures and 3–5% of all fractures involving the shoulder girdle, making them comparatively uncommon injuries [1]. These fractures are typically caused by high-energy trauma. Since patients with scapular fractures commonly have multiple concurrent injuries involving the pulmonary system, cervical spine, or cranial region, the reported mortality rate for these individuals ranges from 10% to 15% [2]. The majority of scapular fractures can be satisfactorily treated without surgery. Because the scapula is surrounded by several muscles that give the bone a good vascular supply, scapular fractures usually heal successfully without surgery [3].
According to reports, arthrosis, rotator cuff dysfunction, scapulothoracic dyskinesis, and impingement pain all contributed to decreased shoulder function after nonsurgical therapy. In addition, it was noted that surgical intervention for scapular fractures produced better results and a higher functional recovery [4,5]. When there is 2 cm medialization of the lateral column or when the scapular body is angulated more than 40°, open reduction and internal fixation (ORIF) is frequently carried out [6]. We present a case report of an isolated extraarticular scapular fracture with significant displacement of the lateral column managed with ORIF using reconstruction plates.
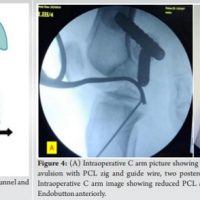
A 51-year-old female presented to our emergency department with a history of fall of heavy object over her right shoulder. She presented with pain over her right scapular region and shoulder, and inability to move her shoulder. She had no other injuries and was vitally stable. Radiographs were taken, which showed a fracture of the lateral column and body of the scapula. To better understand the anatomy of the fracture, 3D computed tomography (CT) scan was performed (Fig. 1). It revealed an extraarticular fracture of the lateral column with significant displacement and a glenopolar angle of >40° along with a scapular spine fracture. We decided to go ahead with surgical fixation of the fracture once the patient was cleared for surgery.
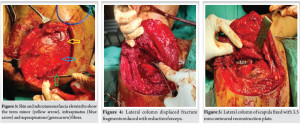
The patient was placed in lateral decubitus position (Fig. 2) and a boomerang incision was taken starting from the inferior angle of the scapula along the medial border of the scapula and then turning over the superomedial angle toward the subcutaneous spine of the scapula. A large skin flap and subcutaneous fat are elevated off the scapular fascia to reveal the supraspinatous, posterior fibers of the deltoid, infraspinatus, teres minor and superior fibers of teres major (Fig. 3). The posterior fibers of the deltoid were released from the spine of scapula and elevated to expose the lateral extent of the infraspinatus and teres minor muscle bellies. A modified Judet approach was taken between the interval between infraspinatus and teres minor to reach the lateral border of the scapula for fracture fixation. The ascending branch of the circumflex scapular artery was encountered and ligated. Care was taken to prevent injury to the suprascapular nerve and vessels as they are in close proximity and are known to be injured during this approach. The lateral column fragments were reduced anatomically and held in place with a reduction forceps (Fig. 4). The scapular body fragment was lateralized due to the pull of the infraspinatus and teres minor. The fragment was medialized toward the glenoid neck fragment and fixed with a 3.5 mm seven-hole precontoured reconstruction plate (Fig. 5). The scapular spine fracture line was exposed by elevating fibres of the supraspinatous from the spine of the scapula and was reduced anatomically with a reduction forceps. The fracture was fixed with a 3.5 mm eight-hole precontoured reconstruction plate (Fig. 6). Copious fluid irrigation was done, and the reflected fibres of the posterior deltoid were reattached to the scapular spine. The interval between infraspinatus and teres minor was not sutured. A drain tube was inserted, which was removed after 24 h. Finally, the Bomerang skin flap was closed in layers, and a sterile dressing was done.

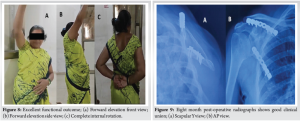
Post-operative radiographs showed excellent fracture reduction (Fig. 7). Post-operative pendulum exercises were started 24 h after surgery, followed by passive range of motion and scapular stabilization exercises at 2 weeks. Active range of motion exercises were started at 6 weeks post-surgery. Once 90% of the normal range of motion was achieved in all plane’s scapular, rotator cuff, and deltoid strengthening exercises were initiated at 4 months post-surgery. The patient shows a good functional outcome (Fig. 8) and radiological union (Fig. 9) at 8 months post-surgery.
Scapular fractures are relatively rare injuries, constituting up 1% of all fractures and 3–5% of all fractures involving the shoulder girdle [1]. High-energy trauma is usually the cause of these fractures. The reported death rate for patients with scapular fractures ranges from 10% to 15% since these patients frequently have numerous concurrent injuries involving the cervical spine, pulmonary system, or cranial region [2]. The majority of scapular fractures can be satisfactorily treated without surgery. Because the scapula is surrounded by several muscles that give the bone a good vascular supply, scapular fractures usually heal successfully without surgery [3]. These fractures are linked to clavicle fractures, which cause the “floating shoulder” phenomenon. The decision to undertake osteosynthesis of the clavicle, which would indirectly reduce the scapula’s column and achieve shoulder stability, is heavily influenced by the extent of ligament lesions and the degree of dislocation [7].
When there is 2 cm medialization of the lateral column or when the scapular body is angulated more than 40°, ORIF is frequently carried out [6]. The current standards of care recommend at least one of the following for surgical intervention: (a) Intra-articular glenoid surface stepoff in CT of more than 4 mm; (b) Line of fracture spanning the spine, scapular body, and neck; (c) More than 40° angular deformities on the scapular-Y view; (d) Shortening or displacement of more than 20 mm on Anteroposterior radiography or CT scan; (e) CT scans with a glenopolar angle <10; (f) Acromioclavicular dislocation or floating shoulder (concomitant clavicle, acromion, or coronoid process fracture with displacement >10 mm) [8]. Debate remains regarding the best treatment of intra-articular and significantly displaced scapula fractures. Although a few researchers have found positive results following nonoperative treatment, other authors have reported less than universally acceptable outcomes [9]. Pain, instability, and the avoidance of degenerative joint disease should be the main objectives of surgical treatment for these injuries [10].
The posterior (Judet) approach is one of the most popular and useful surgical techniques for the scapula. It entails separating the infraspinatus muscle from the infraspinatus fossa to reduce and fix scapular fractures [11]. The Judet technique has long been the accepted method for treating scapular fractures surgically. We used the modified Judet approach in which the infraspinatus muscle is not separated from the scapular fossa, which is the only change made to this method. We dissect in the interval between infraspinatus and teres minor, with the capacity to visualize all fracture patterns and lines and treat intra-articular and glenoid fractures without the morbidity of significant dissection. This updated approach offers all the benefits of the original method. Due to its closeness to the axillary nerve inferiorly and the suprascapular nerve and vessel superiorly, the modified Judet technique requires careful dissection. These important structures can be harmed by excessive dissection and traction. It is necessary to firmly reattach the deltoid that was separated from its origin from the scapular spine and acromion, ideally by creating osseous tunnels. If not, chronic shoulder pain and a loss of deltoid strength will result [10]. Porcellini et al. observed in an observational study that an infraspinatus-sparing surgical approach for scapular fracture prevents external-rotation weakness and infraspinatus hypotrophy. They also recommended that the classic Judet approach be limited to difficult fractures that are not reducible with a narrow exposure [12].
Scapular fractures present special difficulties in terms of access and fixing technique, making internal fixation a difficult treatment. It will be difficult to get a good intra-operative radiography imaging and an appropriate reduction, especially when the fracture is comminuted. In addition, there is a chance that the neurovascular structures surrounding the scapula will sustain damage. According to clinical observations, comminuted extra-articular fractures of the glenoid neck or scapular body account for the majority of unstable scapular fractures. These intricate fractures can be fixed with a range of implants. Locking compression plates, reconstruction plates, distal radius plates, distal humerus Y-type locking plates, T-plates, calcaneous deformed plates, and microplates are a few of the implants used to fix scapula fractures that have been documented in the literature [8].
Zlowodzki et al. conducted a systematic review that included 22 case series totaling 520 cases. According to their findings, 12% of patients with conservatively treated extra-articular scapula fractures experienced chronic discomfort, 25% had radiographic scapula deformity, and 20% had poor functional results [3]. Operative fixation is necessary for displaced and comminuted fractures, according to another systematic study conducted by Kannan et al. They discovered that the functional outcome after operational care was better for displaced scapular neck fractures (>10 mm) [13].
In their retrospective study, Jaikish and Sambandam examined 12 patients who received treatment between 2015 and 2018 for neck fractures with displaced scapular bodies. By using a modified Judet technique, scapular fractures were exposed and repaired using either a recon locking plate and screws or a 3.5 mm T buttress. The average age of the study participants was 42 years old. The follow-up period was 33 months on average. The average Murley score and constant were 80. Four patients showed excellent outcomes, seven showed decent results, and one showed a fair result. At the time of the last follow-up, the shoulder’s mean post-operative range of motion was 34° of external rotation, 136° of abduction, and 140° of forward flexion. He came to the conclusion that internal fixation using T buttress locking plates and reconstruction plates produces good functional results for displaced extra-articular scapular fractures [14].
Isolated scapular fractures are rare fractures, with most of them being treated conservatively. However, fixation is indicated in certain situations, as poor functional results have been reported with conservative treatment in many cases. The modified Judet approach in the open reduction and fixation offers a great exposure of the glenoid neck and lateral column fractures for fixation while causing minimal morbidity and good functional results.
Significantly displaced extraarticular glenoid neck and lateral column fractures need ORIF with anatomically countered plates, and the modified Judet approach provides an excellent exposure of such fracture patterns with minimal morbidity.
References
- 1.Goss TP. Scapular fractures and dislocations: Diagnosis and treatment. J Am Acad Orthop Surg 1995;3:22-33. [Google Scholar | PubMed]
- 2.Armstrong CP, Van der Spuy J. The fractured scapula: Importance and management based on a series of 62 patients. Injury 1984;15:324-9. [Google Scholar | PubMed]
- 3.Zlowodzki M, Bhandari M, Zelle BA, Kregor PJ, Cole PA. Treatment of scapula fractures: Systematic review of 520 fractures in 22 case series. J Orthop Trauma 2006;20:230-3. [Google Scholar | PubMed]
- 4.Nordqvist A, Petersson C. Fracture of the body, neck, or spine of the scapula. A long-term follow-up study. Clin Orthop Relat Res 1992;283:139-44. [Google Scholar | PubMed]
- 5.Cole PA, Talbot M, Schroder LK, Anavian J. Extra-articular malunions of the scapula: A comparison of functional outcome before and after reconstruction. J Orthop Trauma 2011;25:649-56. [Google Scholar | PubMed]
- 6.Schwartzbach CC, Seoudi H, Ross AE, Hendershot K, Robinson L, Malekzadeh A. Fracture of the scapula with intrathoracic penetration in a skeletally mature patient. A case report. J Bone Joint Surg Am 2006;88:2735-8. [Google Scholar | PubMed]
- 7.DeFranco MJ, Patterson BM. The floating shoulder. J Am Acad Orthop Surg 2006;14:499-509. [Google Scholar | PubMed]
- 8.Noguchi T, Mautner JF, Duncan SF. Dorsal plate fixation of scapular fracture. J Hand Surg Am 2017;42:843.e1-5. [Google Scholar | PubMed]
- 9.Scavenius M, Sloth C. Fractures of the scapula. Acta Orthop Belg 1996;62:129-32. [Google Scholar | PubMed]
- 10.Obremskey WT, Lyman JR. A modified judet approach to the scapula. J Orthop Trauma 2004;18:696-9. [Google Scholar | PubMed]
- 11.Bauer G, Fleischmann W, Dussler E. Displaced scapular fractures: Indication and long-term results of open reduction and internal fixation. Arch Orthop Trauma Surg 1995;114:215-9. [Google Scholar | PubMed]
- 12.Porcellini G, Palladini P, Congia S, Palmas A, Merolla G, Capone A. Functional outcomes and clinical strength assessment after infraspinatus-sparing surgical approach to scapular fracture: Does it really make a difference? J Orthop Traumatol 2018;19:15. [Google Scholar | PubMed]
- 13.Kannan S, Singh HP, Pandey R. A systematic review of management of scapular fractures. Acta Orthop Belg 2018;84:497-508. [Google Scholar | PubMed]
- 14.Jaikish S, Sambandam B. Functional outcome of open reduction and internal fixation of displaced extra-articular scapula fractures. Indian J Orthop 2021;55:708-13. [Google Scholar | PubMed]