Simultaneous ipsilateral hip, knee, and ankle fracture-dislocation is a rare high-energy injury requiring prompt recognition, imaging, early stabilization, and carefully planned surgical intervention through multidisciplinary management to optimize outcomes.
Dr. Bharat Kumar Soni, Department of Orthopaedics, All India Institute of Medical Sciences, Marudhar Industrial Area, 2nd Phase, M.I.A. 1st Phase, Basni, Jodhpur, Rajasthan, India. E-mail: bsoni9863@gmail.com
Introduction: Co-occurrence of ipsilateral hip, knee, and ankle fracture-dislocation is a rare condition demanding heightened urgency, constituting an emergency warranting immediate attention and utmost care. Delineating the management of such injury is required so that satisfactory functional outcomes can be achieved in this uncommon injury.
Case Report: A 41-year-old male was alleged to have sustained a road traffic accident, following which he presented to the emergency department of a tertiary care center with pain over the left hip, knee, and ankle joints, and deformity of the same limb. He was evaluated and diagnosed with ipsilateral hip fracture-dislocation, knee fracture-dislocation, and bimalleolar ankle fracture with ankle subluxation. He underwent open reduction internal fixation (ORIF) with raft plate (7H) for the proximal tibia fracture and two Herbert screws for the tibial spine fracture for fixing the knee fracture-dislocation. ORIF with 2 CC screw for medial malleolus and ORIF with 1 CC screw for lateral malleolus was done to fix ankle fracture subluxation. No surgical intervention was required for hip fracture-dislocation.
Conclusion: Simultaneous ipsilateral hip, knee, and ankle fracture-dislocation is a rare condition that should be approached as a limb-threatening orthopedic emergency. We report this case for its rarity and to document that good results can be achieved with early appropriate care.
Keywords: Hip fracture dislocation, Knee fracture dislocation, ankle fracture dislocation, Ipsilateral limb injuries, High energy trauma
The dislocation of the hip, knee, and/or ankle joint typically necessitates prompt surgical intervention, yet the co-occurrence of ipsilateral hip, knee, and ankle fracture-dislocation demands heightened urgency, constituting an emergency warranting immediate attention and expeditious care [1]. Such injuries are predominantly resulting from high-velocity motor vehicle collisions [2]. When associated with neurovascular compromise, these injuries are further complicated by the challenges of limb viability, and the prognosis is unfavorable if not properly managed. We document a case presented in the emergency department with ipsilateral hip fracture-dislocation, knee fracture-dislocation, and bimalleolar ankle fracture with ankle subluxation. In this discourse, we delineate the chronological events of management and elucidate the ultimate functional outcome of this infrequent injury.
A 41-year-old male motorcyclist sustained a road traffic accident (2 weeks vs. 4 weeks) presented to the 41-year-old male motorcyclist sustained a road traffic accident (2 weeks vs. 4 weeks) and presented to the emergency department of the tertiary care center, presenting his left hip in an attitude of flexion, adduction, and internal rotation, left knee swollen and posterior dislocated and left ankle swollen and valgus deformity, along with a lacerated wound of 3 cm over the right mid-leg (Fig. 1). The advanced trauma life support protocol was followed, and initial management was started. The range of movements at the hip, knee, and ankle joints was painful and restricted. After initial stabilization, radiographs were done and a diagnosis of the left-sided posterior hip dislocation with posterior wall rim fracture with knee fracture-dislocation with bimalleolar ankle fracture (Lauge-Hansen type Supination External Rotation) with ankle subluxation which was established on X-rays (Fig. 2).


Closed reduction of the left hip and left knee was done under mild sedation anesthesia in the emergency department, and calcaneal skeletal pin traction with an above-knee slab was applied to maintain the reduction. The knee dislocation was reduced by gentle traction applied to the leg. Further traction on the left hip with the hip in 90° flexion with an assistant stabilizing the pelvis, Allis 90/90 hip reduction maneuver, reduced the left hip dislocation which was stable post-reduction. During the procedure, anterior tibial artery, dorsalis pedis artery, and posterior tibial artery pulses were clinically checked regularly and were palpable. Post-reduction X-rays confirmed the reduction (Fig. 3). A computed tomography (CT) scan of the pelvis showed only a small posterior wall fracture fragment (Thompson-Ebstein type-1) with a congruently reduced hip joint, without any intra-articular loose body (Fig. 4). Magnetic resonance imaging (MRI) with CT scan was performed for the left knee was suggestive of tibial avulsion of the anterior cruciate ligament (ACL) (Mayer-Mckeever type 2) and lateral collateral ligament grade I tear at the femoral insertion along with proximal tibia fracture (Fig. 5 and 6).



The patient was transferred to the ward and after 4 days when the swelling subsided, shifted to operation theater, and given combined spinal epidural and positioned supine. He underwent open reduction internal fixation (ORIF) with raft plate (7H) for the proximal tibia fracture (Hohl and Moore type 2) and 2 Herbert screws for the tibial spine fracture (3.5 mm, 40 mm × 2) for the knee. ORIF with 2 CC screw for medial malleolus and ORIF with 1 CC screw for lateral malleolus was done to fix ankle fracture subluxation. No surgical intervention was required for hip fracture-dislocation (Fig. 7).

Below knee slab and knee range of motion (ROM) brace were applied postoperatively. The post-operative period was uneventful and no complication was noted; suture removal was done at 2 weeks. After 2 weeks, slab and brace were removed and, ROM exercises and non-weight-bearing mobilization were started. Rehabilitation protocol for multi-ligament injury of the knee was started. (Table 1). Functional outcome was measured using Harris Hip Score for hip joint, Lysholm Knee Score for knee joint, American Orthopedic Foot and Ankle Society–Ankle-Hindfoot Scale for foot joint (Table 2). At 6 weeks, partial weight-bearing and strength training was started.


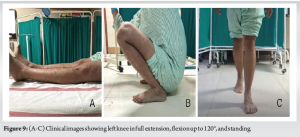
The patient was followed up in the outpatient department routinely, and subsequent radiographs were taken (Fig. 8). Six months post-surgery, the patient was able to achieve adequate hip, knee, and ankle ROM and walked unassisted with full weight bearing. He was also able to do squatting and sitting cross-legged comfortably at the end of 6 months postoperatively (Fig. 9).

Hip, knee, and ankle fracture-dislocation is a rare clinical occurrence and when present simultaneously, they should be approached as a limb-threatening emergency. A general physical examination with appropriate X-rays of the injured part should be performed on arrival at the emergency room. The neurovascular status of the injured lower limb should be well performed and documented, and it should be serially monitored. Hip dislocations in these injuries occur following axial forces acting on the flexed hip and are often associated with acetabular fractures, particularly posterior wall [3]. Posterior dislocation of the hip has been classified by Thompson and Epstein [4]. In our case, it was a Type 1 posterior dislocation of the hip, which is also the most common type. Treatment for this dislocation consists of closed reduction as soon as possible followed by immobilization in Buck’s traction, a cast, or a Thomas splint or skeletal traction for 2 weeks [5]. The extent of acetabular involvement and the stability of the hip post-reduction are pivotal factors influencing the course of the treatment. When the involvement surpasses 65% of the posterior wall, reconstruction of the acetabular wall becomes imperative to ensure hip stability [1]; however, irreducible or unstable hips post-reduction may necessitate resorting to open reduction. The complications of knee dislocation may be disastrous and must be anticipated. The incidence of vascular injuries in knee dislocations was around 18% in a study conducted by Medina et al. [6]. The popliteal artery is vulnerable to such trauma due to its unique fixation and anatomic relationships; intima disruption, dissection, thrombosis, pseudoaneurysm, and partial or complete transection. In our case, we used Doppler along with a pulse oximeter waveform for monitoring, and the Doppler signals were compared to the uninjured side. The peroneal nerve is injured most often, and the prognosis for return of function after injury is guarded. In a systematic review of Woodmass et al., [7] the majority of patients achieved complete recovery in incomplete palsy, and recovery was seen in <40% of patients with complete peroneal nerve palsy. Knee dislocations can be classified according to the Kennedy position or the Schenck anatomic classification system [8]. Knee dislocations can be reduced satisfactorily by closed methods. Immediate surgical intervention is indicated for an irreducible knee by closed reduction or an unstable knee, which requires a vascular repair and open knee dislocation. Circulation should be assessed periodically for 5–7 days. Once it is certain that the circulation is not impaired, treatment may be done for injured ligaments. MRI provides critical information regarding ligament injuries, meniscal injuries, chondral injuries, and fractures to guide treatment, particularly after an acute knee dislocation. Approximately 50% of knee dislocations are associated with tears of the ACL, whereas 75% are associated with tears of the posterior cruciate ligament [9]. Avulsion fractures of cruciate and collateral ligaments can be fixed with non-absorbable sutures or screws in isolation or while fixation of associated fractures around the knee. Whereas Jlidi et al. reported a case of a 35-year man in a road traffic accident with ipsilateral hip fracture-dislocation and a knee dislocated with patella fracture, the hip was closed reduced, and managed conservatively and the knee was reduced and stabilized with the external fixator [10]. Sharma et al. [11] mentioned 23-year-old male with ipsilateral hip fracture-dislocation and knee dislocation with a ligament injury. In the latter case, both joints were reduced in an emergency, and posterior wall acetabulum was fixed urgently and the delayed knee ligament was reconstructed. Falgons and Warner [12], in their study, reported 40-year-old male with ipsilateral posterior hip and anterior knee dislocation (Schenck type V) with ipsilateral femoral head fracture and incomplete femoral neck fracture. Three CC screws for the femoral neck and three cortical screws for the femur head was used to fix the fracture. Three months after injury, he underwent open treatment for osteochondral fracture medial condyle distal femur, ACL reconstruction with quadricep tendon autograft, and arthroscopic medial and lateral meniscus repair. Khan et al. reported a case of ipsilateral central hip and knee fracture-dislocation but even after fixing all the fractures, the patient later developed avascular necrosis and underwent total hip replacement [13]. Waterman and Banerjee [14], in their report, mentioned that in their case, a 25-year-old man presented with hip and knee dislocation which was closed reduced, an open tibia fracture was debrided, and intramedullary tibia nail was done and in the diastasis in the ankle was stabilized using syndesmotic screw. Salaria et al. [15] mentioned in their report a case of 37-year-old male farmer with the right knee lateral dislocation and ipsilateral ankle fracture-dislocation. Both were reduced initially in emergency and external fixator was applied to stabilize and later definitive fixation was done once swelling subsided. The ipsilateral hip, knee, and ankle fracture-dislocation is an uncommon phenomenon with various surgeon-related factors that could improve outcomes including emergent reduction of the knee joint, assessment of neurovascular injury, reduction of the hip joint as soon as possible, preferably in the emergency room with the knee stabilized, stabilization of the ankle joint and management of the multi-ligament knee injury on an elective basis.
Review of literature of reported cases of multiple joint fracture-dislocation in ipsilateral lower limb (Table 3).

Simultaneous ipsilateral hip, knee, and ankle fracture-dislocation is rare condition with limited reports reported in literature that should be approached as a limb-threatening injury and orthopedics emergency. We report this case for its rarity and to document that achieving good results is possible with early appropriate treatment.
Simultaneous ipsilateral hip, knee, and ankle fracture-dislocation is an extremely rare and severe high-energy injury. Early recognition, prompt radiographic assessment, staged surgical intervention, and a coordinated multidisciplinary approach are crucial in achieving optimal functional outcomes and limb salvage in such complex presentations.
References
- 1.Perumal R, Sundararajan SR, Vasudeva J, Rajasekaran S. Ipsilateral hip and knee dislocation with open tibial fracture: A case report of a limb threatening injury. J Orthop Case Rep 2016;6:47-50. [Google Scholar | PubMed]
- 2.Brautigan B, Johnson DL. The epidemiology of knee dislocations. Clin Sports Med 2000;19:387-97. [Google Scholar | PubMed]
- 3.Clegg TE, Roberts CS, Greene JW, Prather BA. Hip dislocations--epidemiology, treatment, and outcomes. Injury 2010;41:329-34. [Google Scholar | PubMed]
- 4.Yang EC, Cornwall R. Initial treatment of traumatic hip dislocations in the adult. Clin Orthop Relat Res 2000;377:24-31. [Google Scholar | PubMed]
- 5.Hegyes MS, Richardson MW, Miller MD. Knee dislocation. Complications of nonoperative and operative management. Clin Sports Med 2000;19:519-43. [Google Scholar | PubMed]
- 6.Medina O, Arom GA, Yeranosian MG, Petrigliano FA, McAllister DR. Vascular and nerve injury after knee dislocation: A systematic review. Clin Orthop Relat Res 2014;472:2621-9. [Google Scholar | PubMed]
- 7.Woodmass JM, Romatowski NP, Esposito JG, Mohtadi NG, Longino PD. A systematic review of peroneal nerve palsy and recovery following traumatic knee dislocation. Knee Surg Sports Traumatol Arthrosc 2015;23:2992-3002. [Google Scholar | PubMed]
- 8.Goebel CP, Domes C. Classifications in brief: The schenck classification of knee dislocations. Clin Orthop Relat Res 2020;478:1368-72. [Google Scholar | PubMed]
- 9.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med 1995;23:580-7. [Google Scholar | PubMed]
- 10.Jlidi M, Bouaicha W, Mallek K, Gharbi MH, Jaziri S, Daas S. A rare concomitant ipsilateral hip and knee dislocations: A case report and review of the literature. SAGE Open Med Case Rep 2024;12:2050313X241233199. [Google Scholar | PubMed]
- 11.Sharma G, Chahar D, Sreenivasan R, Verma N, Pankaj A. Ipsilateral hip and knee dislocation: Case report and review of literature. J Clin Orthop Trauma 2016;7:11521. [Google Scholar | PubMed]
- 12.Falgons CG, Warner SJ. Simultaneous ipsilateral hip and knee dislocation: Management and outcome - a case report. Trauma Case Rep 2024;53:101079. [Google Scholar | PubMed]
- 13.Khan AQ, Abbas MB, Agrawal P, Anwer A, Firoz A, Harun F. From trauma to triumph: Navigating the complexities of a central hip and ipsilateral knee dislocation with associated fractures. J Orthop Case Rep 2024;14:118-24. [Google Scholar | PubMed]
- 14.Waterman BR, Banerjee R. Management of simultaneous ipsilateral dislocation of hip, knee, and ankle. Am J Orthop (Belle Mead NJ) 2011;40:301-4. [Google Scholar | PubMed]
- 15.Salaria AK, Vatsyan KC, Kalia S, Gupta L, Rathore LP, Katoch P. Ipsilateral knee dislocation and ankle fracture dislocation. J Orthop Case Rep 2023;13:112-6. [Google Scholar | PubMed]
- 16.DuBois B, Montgomery WH Jr., Dunbar RP, Chapman J. Simultaneous ipsilateral posterior knee and hip dislocations: Case report, including a technique for closed reduction of the hip. J Orthop Trauma 2006;20:216-9. [Google Scholar | PubMed]
- 17.Sen RK, Tripathy SK, Krishnan V, Goyal T, Jagadeesh V. Ipsilateral fracture dislocations of the hip and knee joints with contralateral open fracture of the leg: A rare case and its management principles. Chin J Traumatol 2011;14:183-7. [Google Scholar | PubMed]
- 18.Kreibich DN, Moran CG, Pinder IM. Ipsilateral hip and knee dislocation. A case report. Acta Orthop Scand 1990;61:90-1. [Google Scholar | PubMed]
- 19.Schierz A, Hotz T, Käch K. Ipsilaterale Knie- und Hüftgelenkluxation [Ipsilateral Knee and Hip Joint Dislocation]. Vol. 105. German: Unfallchirurg; 2002. p. 660-3. [Google Scholar | PubMed]
- 20.Motsis EK, Pakos EE, Zaharis K, Korompilias AV, Xenakis TA. Concomitant ipsilateral traumatic dislocation of the hip and knee following high-energy trauma: A case report. J Orthop Surg (Hong Kong) 2006;14:322-4. [Google Scholar | PubMed]
- 21.LaRoque MC, Zeni F, Cole PA. Traumatic bifocal whereas and ipsilateral posterior knee dislocation: A case report. JBJS Case Connect 2023;13: (1). doi: 10.2106/JBJS.CC.22.00408. [Google Scholar | PubMed | CrossRef]
- 22.Malimson PD. Triple fracture-dislocation of the lower limb. Injury 1984;16:11-2. [Google Scholar | PubMed]
- 23.Millea TP, Romanelli RR, Segal LS, Lynch CJ. Ipsilateral fracture-dislocation of the hip, knee, and ankle: Case report. J Trauma 1991;31:416-9. [Google Scholar | PubMed]











