Pseudoaneurysm of the profunda femoris artery is a rare and life-threatening complication following surgical fixation of intertrochanteric fractures. A high index of suspicion is essential for early diagnosis and management, especially in cases involving sharp medial fragments of the fracture, displaced lesser trochanter fragments, or when open reduction is performed using pointed bone levers.
Dr. Shrihari L Kulkarni, Department of Orthopaedics, SDM College of Medical Sciences and Hospital, Shri Dharmasthala Manjunatheshwara University, Dharwad, Karnataka, India. E-mail: shrihari1711@gmail.com
Introduction: Intertrochanteric fractures are one of the most common osteoporotic fractures in the elderly population. Most of them are managed with surgical fixation using proximal femoral nails. We report a patient with pseudoaneurysm of the profunda femoris artery following surgical fixation of an intertrochanteric fracture, which is a very rare complication.
Case Report: An 80-year-old male patient presented 3 weeks post-surgical fixation for an intertrochanteric fracture with pain and swelling of the thigh. Radiological evaluation revealed a pseudoaneurysm of the profunda femoris artery, which was managed by the cardiothoracic and vascular surgery team.
Conclusion: Pseudoaneurysm of the profunda femoris artery, though rare, is a serious complication following surgical fixation of the proximal femur fracture. Considering its potential for delay in onset, it can often be overlooked or diagnosed late, leading to significant risks.
Keywords: Pseudoaneurysm, intertrochanteric fracture, profunda femoris artery, proximal femoral nailing.
A pseudoaneurysm is a localized vascular abnormality that occurs when there is a partial disruption of an arterial wall, leading to blood leakage in the surrounding tissues. Over time, this blood collection becomes encapsulated by a fibrous wall and maintains communication with the parent artery through a channel known as the “neck.” Unlike true aneurysms, pseudoaneurysms do not involve all three layers of the arterial wall. They usually occur following a penetrating trauma or arterial puncture during diagnostic or therapeutic procedures or infections [1]. Vascular injury associated with peritrochanteric femoral fractures is rare but can occur, particularly in the context of modern surgical techniques. The reported incidence of such injuries has increased marginally from 0.2% to 0.49%, likely due to the more frequent use of advanced fixation devices and manipulation required for anatomical fracture reduction. Several intraoperative factors may contribute to iatrogenic vascular injuries, including the sharp bone fragments (e.g., a displaced lesser trochanter) or misdirected screws, overpenetration with drill bits, or improper placement of retractors and bone levers. In addition, limb positioning during surgery, large perineal post, excessive adduction, internal rotation, or traction, can reduce the distance between the femur and the surrounding vasculature, increasing the risk of vascular compromise, particularly to the profunda femoris artery and its branches [2]. Although numerous post-operative complications are well documented in the proximal femur fracture management, including infection, implant failure, and re-fractures in the ipsilateral or fresh fractures on the contralateral side, vascular injuries, especially pseudoaneurysms, remain an uncommon but potentially life-threatening complication. Given the diagnostic challenges and high risk of morbidity, clinicians must maintain a high index of suspicion for such vascular events in the post-operative period. In this report, we present a patient with a pseudoaneurysm of the profunda femoris artery following internal fixation of an intertrochanteric fracture, highlighting the importance of early recognition and multidisciplinary management of the rare complication.
An 80-year-old male presented to our emergency department with a history of a slip and fall at his residence. Following this, he had pain in the right groin and was not able to bear weight on his right lower limb. On examination, the limb was shortened and externally rotated. There was fullness over the right groin, right hip, and greater trochanter, which were tender with restricted hip movements. Radiographs showed Boyd and Griffin Type 2 intertrochanteric fracture with medially displaced lesser trochanter, flexed proximal fragment, adducted, and proximally migrated distal fragment (Fig. 1).

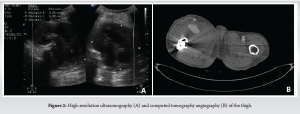
The patient underwent closed reduction and internal fixation with short proximal femoral nail anti-rotation (PFNA-2). Intraoperatively, the reduction was achieved by manipulation of the flexed and adducted proximal fragment with the help of a bone lever (Fig. 1). Intraoperative and post-operative periods were uneventful. The patient was discharged on post-operative day 6, the surgical wound healed, sutures were removed on post-operative day 15, and the patient was mobilized with partial weight bearing with walker support. The patient presented to us again on post-operative day 21 with complaints of pain and swelling over the right thigh. There was no history of fever or re-trauma, and the patient was able to walk full weight bearing with walker support. There was a pitting type of edema in his right lower limb extending up to the right proximal thigh. There was diffuse fullness over the anterior aspect of the thigh, which was more prominent on quadriceps contraction. All the peripheral pulses were well felt, there was no calf tenderness, and no neurological deficits. High-resolution ultrasonography showed a well-defined hetero-echoic collection in the proximal thigh in anterior and medial aspect with central anechoic area probably communicating to the femoral artery measuring 6.2 × 6.9 × 10.2 cm and showing Yin–Yan sign in color Doppler suggestive of pseudoaneurysm with peripheral thrombosis (Fig. 2). The computed tomography (CT) angiography of the right lower limb showed a well-defined contrast filled saccular outpouching with smooth surface seen arising from posterior wall of proximal portion of profunda femoris artery distal to common femoral artery bifurcation. There was no evidence of thrombus within the outpouching. Surrounding organized hematoma noted in the anterior and medial aspect of the thigh, approximately measuring 6.5 × 8.5 × 14 cm, suggestive of pseudoaneurysm of the right profunda femoris artery (Fig. 2).
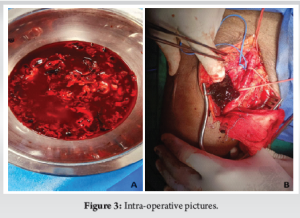
The patient was taken up for the surgery by the cardiothoracic and vascular surgery team, where the patient underwent hematoma evacuation and ligation of profunda femoris artery (Fig. 3). The patient had developed hypovolemic shock and was intubated. He succumbed the subsequent day due to cardiac arrest.
The profunda femoris artery originates from the posterolateral aspect of the femoral artery approximately 3 cm below the inguinal ligament. It travels medially and posteriorly along the thigh, giving rise to the medial and lateral circumflex femoral arteries, and continues through the adductor muscles to supply the posterior compartment of the thigh via its perforating branches [3]. Intertrochanteric fractures are common in the elderly population, particularly among osteoporotic patients, and their incidence is rising [4,5]. Intramedullary fixation devices, such as the PFNA, have become the preferred treatment due to less invasiveness and better biomechanical stability compared to dynamic hip screws [6]. Although multiple complications following surgical fixation of these fractures are well recognized, including infection, nerve injury, implant failure, and wound problems, vascular injuries remain rare, with an incidence of around 0.2% [7]. These injuries may result from the fracture pattern itself or iatrogenic causes during surgery. The close anatomical relationship of the profunda femoris artery and its branches to the medial and posterior aspects of the proximal femur renders these vessels vulnerable to damage, particularly in cases with displaced fracture fragments such as an avulsed lesser trochanter [8,9]. Iatrogenic vascular injury can occur during fracture fixation through several mechanisms: The use of bone levers or retractors placed too aggressively, over-penetration of drill bits during distal locking, or selection of screws that are too long and breach the medial cortex, impinging on adjacent vessels [10,11]. In addition, limb positioning on the fracture table, specifically adduction, internal rotation, and traction, may stretch and compress the vessels, further increasing their risk of injury [12,13]. A pseudoaneurysm develops when arterial wall integrity is compromised, causing blood to escape and form a fibrous capsule containing hematoma that remains in communication with the artery. Unlike true aneurysms, pseudoaneurysms lack all arterial wall layers, making them prone to expansion, rupture, and secondary complications such as infection, neurovascular compression, ischemia, and pain [1,2]. In the present case, the likely cause of the pseudoaneurysm was injury to the profunda femoris artery from the displaced lesser trochanter fragment, as suggested by the anatomical correlation. The manipulation of the proximal fragment with a bone lever during reduction could also have contributed. There was no evidence of screw over-penetration or improper drilling. The delayed presentation of 3 weeks postoperatively with swelling and pain is typical but often leads to diagnostic delays, as these symptoms may be mistakenly attributed to common post-operative changes. Persistent or progressive swelling, unexplained anemia, and bruising should prompt early vascular evaluation. Accurate diagnosis requires a high clinical suspicion supported by imaging modalities such as Doppler ultrasound and CT angiography. Timely recognition is critical to prevent catastrophic complications, including rupture and hemorrhagic shock. Preventative measures include careful surgical technique: Neutral limb positioning during distal locking, use of guarded drill bits, selecting appropriate screw length, and cautious placement of retractors and bone levers. Reducing traction before drilling and avoiding excessive limb adduction or internal rotation can help maintain safe distances between hardware and vessels. Hence, although rare, a profunda femoris artery pseudoaneurysm is a serious complication after proximal femur fracture fixation. Awareness and vigilance during and after surgery are essential for early diagnosis and effective multidisciplinary management to reduce morbidity and mortality.
Pseudoaneurysm of the profunda femoris artery is an uncommon but potentially life-threatening complication following surgical fixation of proximal femur fractures. Due to its rarity and often delayed presentation, it can be easily overlooked, leading to serious consequences such as hemorrhage, neurovascular compression, or compromised limb function. Clinicians should maintain a high index of suspicion in post-operative patients presenting with persistent thigh swelling, pain, or unexplained anemia. Early diagnosis using Doppler ultrasound and CT angiography, followed by prompt multidisciplinary management involving orthopedic surgeons and vascular specialists, is crucial to prevent severe complications and improve patient outcomes.
Patients present with post-operative swelling in the thigh, pain, or unexplained anemia following fixation of an intertrochanteric fracture, one must suspect the possibility of a pseudoaneurysm of the profunda femoris artery.
References
- 1. Singh S, Arora S, Thora A, Mohan R, Sural S, Dhal A. Pseudoaneurysm of profunda femoris artery following dynamic hip screw fixation for intertrochanteric femoral fracture. Chin J Traumatol 2013;16:233-6. [Google Scholar] [PubMed]
- 2. Samaan M, Idres FA, Hawa Y, Madania M. Late deep femoral artery injury after intertrochanteric hip fracture treatment: A case report. Int J Surg Case Rep 2023;105:107983. [Google Scholar] [PubMed]
- 3. Ginzburg E, Chong CK, Rich NM. Vascular anatomy of the extremities. In: Asensio JA, Trunkey DD, editors. Current Therapy of Trauma and Surgical Critical Care. St. Louis: Mosby; 2008. p. 467-72. [Google Scholar] [PubMed]
- 4. Kanis JA, Black D, Cooper C, Dargent P, Dawson-Hughes B, De Laet C, et al. A new approach to the development of assessment guidelines for osteoporosis. Osteoporos Int 2002;13:527-36. [Google Scholar] [PubMed]
- 5. Dauwe J, Verhulst K, Grechenig P. The 25 highest cited papers in trochanteric fractures. A systematic review. Biomed Surg 2017;1:40-6. [Google Scholar] [PubMed]
- 6. Sun Q, Fan G, Li X, Gong J, Ge W, Cai M. Relationship between femur and femoral arteries for identifying risk factors for vascular injury. Med Sci Monit 2017;23:1733-40. [Google Scholar] [PubMed]
- 7. Gong J, Liu P, Cai M. Imaging evaluation of the safe region for distal locking screw of proximal femoral nail anti-rotation in patients with proximal femoral fracture. Med Sci Monit 2017;23:719-24. [Google Scholar] [PubMed]
- 8. Rajasekaran K, Amin A, Arora S, Walton NP. Pseudoaneurysm of a branch of the profunda femoris artery following distal locking of an intramedullary hip nail: An unusual anatomical location. Hip Int 2008;18:231-5. [Google Scholar] [PubMed]
- 9. Potenza V, Saputo U, Catellani F, Farsetti P, Caterini R. Laceration of a branch of the profunda femoris artery caused by a spike of the displaced lesser trochanter in an inter-trochanteric femoral fracture. A case report. Int J Surg Case Rep 2016;24:195-8. [Google Scholar] [PubMed]
- 10. Lazarides MK, Arvanitis DP, Dayantas JN. Iatrogenic arterial trauma associated with hip joint surgery: An overview. Eur J Vasc Surg 1991;5:549-56. [Google Scholar] [PubMed]
- 11. Yang KH, Park HW, Park SJ. Pseudoaneurysm of the superficial femoral artery after closed hip nailing with a gamma nail: Report of a case. J Orthop Trauma 2002;16:124-7. [Google Scholar] [PubMed]
- 12. Grimaldi M, Courvoisier A, Tonetti J, Vouaillat H, Merloz P. Superficial femoral artery injury resulting from intertrochanteric hip fracture fixation by a locked intramedullary nail. Orthop Traumatol Surg Res 2009;95:380-2. [Google Scholar] [PubMed]
- 13. Vande Voorde K, Dauwe J, Van Oost J. Late presentation of an iatrogenic pseudoaneurysm of the profunda femoris artery following intramedullary nailing. Case Rep Orthop 2018;2018:8270256. [Google Scholar] [PubMed]









