PHILOS plate fixation offers reliable anatomical reduction and stable fixation in proximal humerus fractures, even in elderly osteoporotic patients, enabling early mobilization and good functional outcomes with minimal complications when applied with proper surgical technique.
Dr. S Krishna Kumar, Department of Orthopaedics, Teerthanker Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India. E-mail: kkasik009@gmail.com
Introduction: Proximal humerus fractures (PHFs) are among the most frequently encountered fractures in clinical orthopedic practice, particularly in the elderly population. Although many cases can be managed conservatively, complex and displaced fractures often require surgical intervention. Proximal humerus internal locking system (PHILOS) plating has emerged as an effective treatment modality in these cases, especially in osteoporotic bone.
Materials and Methods: This retrospective cum prospective clinical study was conducted over 2 years and included 30 patients aged 18–65 years with PHFs treated surgically with PHILOS plating. Fractures were classified using Neer’s classification. Patients were followed for a minimum of 4 months. Functional outcomes were assessed using the Constant-Murley score.
Results: The mean age of patients was 39.56 ± 9.41 years, with a majority being in the age group of 30–50 years. The distribution of fractures included 2-part (33.3%), 3-part (56.6%), and 4-part fractures (10%). At the final follow-up, 46.7% of patients had excellent outcomes, 30% good, 13.3% fair, and 10% poor. The mean Constant-Murley score was 78. Patients with 2-part fractures had the highest mean score (81.2), followed by 3-part (78.8), and 4-part fractures (59.3).
Conclusion: PHILOS plate fixation for PHFs provides stable internal fixation, enables early mobilization, and leads to good-to-excellent functional outcomes, particularly in less complex fracture patterns. Early rehabilitation further enhances recovery.
Keywords: Proximal humerus fracture, proximal humerus internal locking system plate, Constant-Murley score, internal fixation, shoulder function.
Proximal humerus fractures (PHFs) rank among the top seven most frequent fractures in the adult population and represent a significant portion of injuries treated by orthopedic surgeons worldwide. These fractures account for 4–10% of all skeletal injuries and approximately 26% of all humeral fractures [1]. The incidence is notably higher in the elderly, primarily due to osteoporosis and age-related bone fragility, whereas in younger populations, they are usually caused by high-energy trauma such as road traffic accidents or falls from height [2,3]. These fractures vary widely in severity, ranging from non-displaced, stable fractures to complex multi-fragmentary patterns. While the majority (up to 80%) of PHFs can be managed nonoperatively with acceptable outcomes, approximately 20% necessitate surgical intervention due to displacement, instability, or intra-articular extension [4]. Neer’s classification system remains the standard for categorizing these injuries, based on the number of displaced fragments and their angulation and displacement thresholds (>1 cm or >45°) [5]. Achieving good functional outcomes in displaced PHFs can be challenging. Osteoporotic bone, the risk of avascular necrosis, and the proximity to vital neurovascular structures make internal fixation demanding. Historically, non-locking compression plates were used, but they often failed in elderly patients due to screw loosening, pull-out, and collapse of the fracture site [6,7].
The advent of locking compression plates, particularly the proximal humerus internal locking system (PHILOS) plate, has revolutionized the surgical management of these fractures. Designed with multi-angled locking screw options that offer both angular and axial stability, the PHILOS plate is especially beneficial in osteoporotic bone. The divergent and convergent screw orientation enhances purchase in the humeral head, reduces the risk of screw backout, and facilitates early mobilization [8-10]. Several studies have reported favorable outcomes with PHILOS plates, including high rates of union, improved functional scores, and a low incidence of hardware-related complications [11,12]. However, outcomes can vary significantly based on fracture complexity, quality of reduction, bone quality, and adherence to rehabilitation protocols. The present study aims to evaluate the short-term functional outcomes of patients with PHFs treated with PHILOS plating and to analyze the results across different types of fracture patterns as per Neer’s classification using the Constant-Murley score–a widely accepted measure of shoulder function incorporating pain, activities of daily living, range of motion (ROM), and strength [13].
Study design and setting
This retrospective cum prospective clinical study was conducted in the Department of Orthopaedics at Teerthanker Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, over 2 years after getting clearance from the ethical committee.
Inclusion and exclusion criteria
Inclusion criteria
- Age between 18 and 65 years
- Displaced PHFs classified under Neer’s criteria
- Closed fractures.
Exclusion criteria
- Pathological fractures
- Open fractures
- Polytrauma patients with associated severe injuries
- History of previous shoulder surgery or chronic shoulder disorders.
Sample size
A total of 90 patients who met the inclusion criteria were recruited for the study.
Preoperative assessment
Detailed demographic data, mechanism of injury, and clinical history were documented. All patients underwent standard radiographic evaluation with X-rays (anteroposterior and axillary views) and, where necessary, computed tomography scans with 3D reconstruction to better understand fracture morphology. Fractures were classified using Neer’s classification.
Surgical technique
All patients were treated with open reduction and internal fixation using a PHILOS plate. The choice of approach–deltopectoral or deltoid-splitting–was based on surgeon preference and fracture pattern. General anesthesia was administered in all cases.
After reduction of the fracture fragments, the PHILOS plate was positioned laterally on the proximal humerus, ensuring appropriate positioning to avoid impingement. Locking screws were placed into the humeral head in multiple directions for maximum stability. Rotator cuff sutures were passed through the plate when needed, especially in comminuted 3- and 4-part fractures, to augment tuberosity fixation.
Postoperative protocol
- Immobilization in an arm pouch for 1 week
- Pendulum exercises commenced in the 1st week
- Passive ROM started in the 2nd week
- Active-assisted and resisted exercises initiated between 3 and 5 weeks postoperatively.
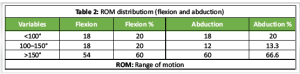
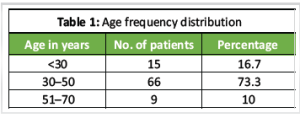
Follow-up and outcome assessment (Table 1-6). Patients were followed at 3 weeks, 6 weeks, and monthly thereafter for a minimum of 4 months. Clinical assessment included evaluation of pain, ROM, strength, and return to daily activities. Functional outcomes were assessed using the Constant-Murley score at 4 months postoperatively.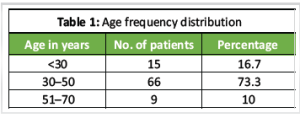
Demographics and fracture patterns (Table 1). The age of patients ranged from 22 to 64 years, with a mean age of 39.56 ± 9.41 years. A significant proportion (73.3%) were between 30 and 50 years. All patients sustained unilateral injuries. The dominant side was involved in 18 patients (60%).
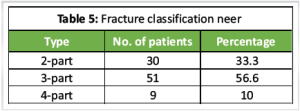
Fractures were classified as follows:
- 2-part fractures: 30 cases (33.3%)
- 3-part fractures: 51 cases (56.6%)
- 4-part fractures: 9 cases (10%).
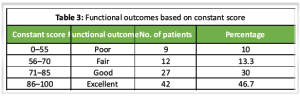
Functional outcome at 4 months (Table 3).
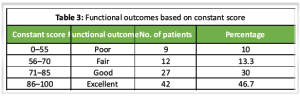
Using the constant-Murley score:
- Excellent (86–100): 42 patients (46.7%)
- Good (71–85): 27 patients (30%)
- Fair (56–70): 12 patients (13.3%)
- Poor (<56): 9 patients (10%).
The overall mean Constant-Murley score was 78, indicating a generally good functional result across the cohort.
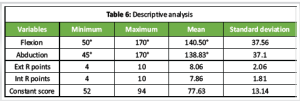
When analyzed by fracture pattern:
- 2-part fractures: Mean score = 81.2
- 3-part fractures: Mean score = 78.8
- 4-part fractures: Mean score = 59.3.
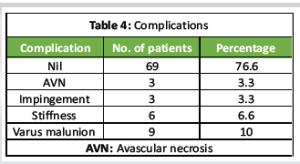
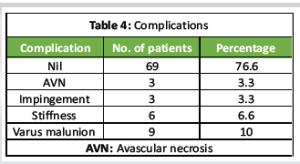
Patients with 2-part fractures had the best functional outcomes, likely due to simpler reduction and more stable fixation. Outcomes in 4-part fractures were less favorable due to the complexity of reduction and higher potential for avascular necrosis. Notably, 10 out of the 21 complications occurred in patients with 4-part fractures, underlining the technical difficulty and poorer prognosis associated with this subgroup. Complications (Table 4) 21 patients had complications. Out of which 10 patients had 4-part fractures. These were linked to avascular necrosis, impingement, varus malalignment and stiffness. No intraoperative complications, deep infections, or implant failures were reported during the study.
The management of PHFs has evolved significantly over the last few decades, with the development of anatomically contoured locking plates such as the PHILOS. This study aimed to evaluate the effectiveness of the PHILOS plate in treating displaced PHFs and to correlate outcomes with fracture complexity. Our findings showed a high rate of excellent and good outcomes (76.7%) with a low complication rate, reinforcing the value of PHILOS plating in managing these injuries. These results are consistent with studies by Patil et al. [8], who reported excellent outcomes in 30 cases treated with PHILOS, and Fazal and Haddad [11], who emphasized the plate’s advantage in achieving stable fixation even in osteoporotic bone. The improved performance in 2-part and 3-part fractures may be attributed to more straightforward anatomical reduction and preservation of the blood supply to the humeral head. Conversely, 4-part fractures pose a greater challenge due to increased risk of avascular necrosis, difficulty in tuberosity fixation, and greater risk of functional impairment, as reflected in their lower mean constant scores. A key strength of the PHILOS plate is its ability to facilitate early mobilization, which is critical in preventing postoperative stiffness–a common issue in shoulder injuries. The locking screw design ensures stable fixation even in compromised bone, reducing the likelihood of reduction loss, particularly in elderly osteoporotic patients [9,10]. Our study supports the use of the PHILOS plate in achieving satisfactory outcomes but also emphasizes the importance of early and aggressive rehabilitation, particularly in patients with complex fractures [14-17].
However, the functional outcomes in 4-part fractures were suboptimal, suggesting limited benefit of PHILOS plating in these cases and the need for careful patient selection. This study demonstrates that open reduction and internal fixation with PHILOS plates offers a reliable and effective treatment option for PHFs, providing good to excellent functional outcomes in most patients. The technique is especially beneficial in younger individuals and those with 2- or 3-part fractures. Early mobilization, meticulous surgical technique, and patient adherence to physiotherapy significantly influence outcomes. While PHILOS plates are not without limitations, especially in highly comminuted fractures, they represent a valuable tool in the modern orthopedic armamentarium for treating displaced PHFs.
Notably, 10 out of the 21 complications occurred in patients with 4-part fractures, underlining the technical difficulty and poorer prognosis associated with this subgroup. PHILOS plating provides optimal results primarily in 2-part and 3-part fractures; its use in 4-part fractures should be approached with caution due to increased complication risks. PHILOS plating is a reliable surgery option for treating displaced PHFs, offering excellent radiological union and functional recovery with minimal complications when performed with proper technique and patient selection.
References
- 1. Passaretti D, Candela V, Sessa P, Gumina S. Epidemiology of proximal humeral fractures: A detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg 2017;26:2117-24. [Google Scholar] [PubMed]
- 2. Thyagarajan DS, Haridas SJ, Jones D, Dent C, Evans R, Williams R. Functional outcome following proximal humeral interlocking system plating for displaced proximal humeral fractures. Int J Shoulder Surg 2009;3:57-62. [Google Scholar] [PubMed]
- 3. Flatow EL. Fractures of the proximal humerus. In: Bucholz RW, Heckman JD, editors. Rockwood and Green’s Fractures in Adults. 6thed. Philadelphia, PA: Lippincott Williams and Wilkins; 2001. p. 997-1035. [Google Scholar] [PubMed]
- 4. Young T, Wallace WA. Conservative treatment of fractures and fracture-dislocations of the upper end of the humerus. J Bone Joint Surg Br 1985;67:373-7. [Google Scholar] [PubMed]
- 5. Hall MC, Rosser M. The structure of the upper end of the humerus with reference to osteoporotic changes in senescence leading to fractures. Can Med Assoc J 1963;88:290-4. [Google Scholar] [PubMed]
- 6. Hawkins RJ, Bell RH, Gurr K. The three-part fracture of the proximal part of the humerus. Operative treatment. J Bone Joint Surg Am 1986;68:1410-4. [Google Scholar] [PubMed]
- 7. Kristiansen B, Christensen SW. Plate fixation of proximal humeral fractures. Acta Orthop Scand 1986;57:320-3. [Google Scholar] [PubMed]
- 8. Patil S, Srinivas P, Bhadbade V. A prospective study of 30 cases of PHILOS plating for displaced proximal humeral fractures. Int J Orthop Sci 2017;3:86-91. [Google Scholar] [PubMed]
- 9. Awal H, Sanaullah B, Israr A, Mohammad A. Outcome of PHILOS plating in proximal humerus fractures. J Pak Orthop Assoc 2016;28:84-7. [Google Scholar] [PubMed]
- 10. Geiger EV, Maier M, Kelm A, Wutzler S, Seebach C, Marzi I. Functional outcome and complications following PHILOS plate fixation in proximal humeral fractures. Acta Orthop Traumatol Turc 2010;44:1-6. [Google Scholar] [PubMed]
- 11. Fazal MA, Haddad FS. Philos plate fixation for displaced proximal humeral fractures. J Orthop Surg (Hong Kong) 2009;17:15-8. [Google Scholar] [PubMed]
- 12. Constant CR, Gerber C, Emery RJ, Sojbjerg JO, Gohlke F, Boileau P. A review of the constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg 2008;17:355-61. [Google Scholar] [PubMed]
- 13. Court-Brown CM, Cattermole H, McQueen MM. Impacted valgus fractures (B1.1) of the proximal humerus. The results of non-operative treatment. J Bone Joint Surg Br 2002;84:504. [Google Scholar] [PubMed]
- 14. Bigliani LU, Flatow EL, Pollock RG. Fractures of the proximal humerus. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD, editors. Fractures in Adults. 4thed. Philadelphia, PA: Lippincott-Raven; 1996. p. 1055-70. [Google Scholar] [PubMed]
- 15. Gerber C, Schneeberger AG, Vinh TS. The arterial vascularization of the humeral head. An anatomical study. J Bone Joint Surg Am 1990;72:1486-93. [Google Scholar] [PubMed]
- 16. Aggarwal S, Bali K, Dhillon MS, Kumar V, Mootha VK. Displaced proximal humeral fractures: An Indian experience with locking plates. J Orthop Surg Res 2010;5:60. [Google Scholar] [PubMed]
- 17. Moonot P, Ashwood N, Hamlet M. Early results for treatment of three- and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br 2007;89:1206-9. [Google Scholar] [PubMed]