For irreducible shoulder dislocations with coronally-split greater tuberosity fractures in the elderly, a “joystick” reduction, informed by a pre-operative 3D-CT diagnosis of complex dual entrapment, exemplifies a successful bone-preserving strategy.
Dr. Tao He, Department of Orthopedics, Chengdu Orthopedic Hospital, Chengdu, Sichuan, China. E-mail: hehuanhuan670@gmail.com
Introduction: Low-energy traumatic irreducible anterior shoulder dislocations with concomitant greater tuberosity fractures in elderly females are rarely reported. The difficulty in reduction is attributed to the interplay between osseous impaction and soft tissue interposition. Three-dimensional computed tomography (CT) was utilized to delineate this combined obstruction mechanism. An open surgical approach incorporating joystick reduction techniques and preservation of the long head of the biceps tendon was implemented. To our knowledge, no systematic therapeutic protocols have been established for such complex injuries in geriatric patients.
Case Report: An 83-year-old Chinese female presented with left shoulder pain and restricted mobility after a ground-level fall. Physical examination revealed a squared shoulder deformity, deltoid muscle strength of 2/5, and sensory abnormalities in the axillary nerve territory. Radiographs confirmed anteroinferior humeral dislocation with comminuted greater tuberosity fracture. Closed reduction attempts failed twice. Three-dimensional CT demonstrated: ① Hill-Sachs defect engaging the anterior glenoid rim; ② coronally split greater tuberosity fragment interposed in joint space; ③ 25 mm medial displacement of proximal humerus. The deltopectoral approach exposed the long head of biceps tendon traversing humeral head, forming complex interposition. Kirschner wire (K-wire) joystick technique was employed to disimpact osseous blocks. Tension band suturing combined with locking plate fixation was performed. Biceps tendon integrity was completely preserved. The post-operative course was uneventful, with satisfactory functional and radiographic outcomes and no recurrent dislocation during follow-up.
Conclusion: This case demonstrates that three-dimensional CT precisely identifies osseous impaction mechanisms in irreducible anterior shoulder dislocations among elderly patients. Intraoperative K-wire joystick techniques combined with long head of biceps tendon preservation achieve anatomical reduction and stability restoration. This protocol establishes a standardized imaging-surgical framework for geriatric osteoporotic patients with failed closed reduction.
Keywords: Shoulder dislocation, humeral fracture, biceps brachii, tomography.
The glenohumeral joint’s high mobility, resulting from a shallow glenoid fossa and lax capsule, leads to the highest dislocation incidence of any major joint, at 23.9/100,000 population. This incidence shows a bimodal age distribution: A peak in young males (15–20 years) due to sports injuries, and a higher rate in females over 63, linked to postmenopausal osteoporosis and capsular degeneration [1]. Anterior dislocation is the most common type, typically caused by axial loading in abduction and external rotation, which can lead to Bankart lesions. Although closed reduction is the standard treatment with favorable outcomes, long-term monitoring for potential recurrence and arthritis is crucial. Consequently, open reduction is rarely required in clinical practice [2]. In the elderly, the risk of an irreducible dislocation is significantly higher, often complicated by osteoporosis, humeral head impaction, massive rotator cuff tears, or soft-tissue interposition like the long head of the biceps tendon (LHBT). Consequently, no consensus exists for managing these complex injuries, with ongoing debates about optimal timing, imaging, and surgical approach. This uncertainty is reflected in the literature; for instance, a recent systematic review by Liechti et al. [3] on the topic did not include any cases with a coronally split greater tuberosity fracture, highlighting a critical gap in evidence. This literature gap is more pronounced for specific fracture patterns. Critically, no quantitative correlation between fragment morphology and reduction difficulty has been established, and there are no documented cases of a coronal split greater tuberosity fracture causing an irreducible dislocation in an elderly female after low-energy trauma – a scenario likely linked to unique osteoporotic fragility patterns. This article reports a rare case of an irreducible anterior shoulder dislocation with a concomitant coronal split greater tuberosity fracture in an octogenarian female with severe osteoporosis following a low-energy fall. We aim to describe the complex “osseous-soft tissue dual entrapment” mechanism as delineated by three-dimensional computed tomography (3D-CT) and present a management framework that prioritizes bone preservation and soft tissue integrity. This framework provides an innovative strategy for addressing such complex geriatric glenohumeral dislocations.
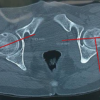
An 83-year-old right-handed female presented to the emergency department with left shoulder pain and deformity. The injury mechanism was confirmed as a ground-level fall. No prior history of shoulder trauma or familial skeletal disorders was documented. Dual-energy X-ray absorptiometry revealed a lumbar spine T-score of −3.1. This value meets the World Health Organization diagnostic criteria for severe osteoporosis. Physical examination revealed pathognomonic squaring deformity of the left shoulder. Complete loss of active motion was observed. Dugas’ sign was confirmed positive. Axillary nerve hypoesthesia was detected in the deltoid dermatome. Deltoid muscle strength was graded 2/5 on the Medical Research Council scale. Intact distal vascular perfusion and radial artery pulsation were documented in the affected upper extremity. Emergency radiographs demonstrated anteroinferior humeral head dislocation. A comminuted greater tuberosity fracture was confirmed. Proximal humeral medial displacement exceeded 25 mm from the coracoid process vertical reference line (Fig. 1a). Closed reduction failed after two attempts. 3D-CT evaluation was subsequently performed.
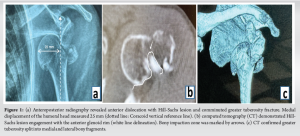
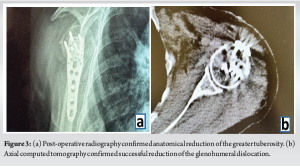
3D CT confirmed two critical findings: ① Posterolateral Hill-Sachs defects were found interlocked with the anterior glenoid rim (Fig. 1b). ② Coronal plane split fracture of the greater tuberosity was observed, separating into medial and lateral fragments. The medial fragment apex was lodged within the anteroinferior labrum (Fig. 1c). These imaging findings collectively indicated irreducible combined osseous and soft tissue interlocking. Closed reduction was reattempted under general anesthesia. Following an unsuccessful outcome, open surgical intervention was ultimately required. A deltopectoral approach was utilized to expose the surgical field. Direct visualization confirmed two pathological findings: Osseous interlocking between the humeral head and anteroinferior glenoid rim; impacted split fracture fragments of the greater tuberosity. Intraoperative exploration revealed pathognomonic elongation of the LHBT. The distended tendon traversed the humeral head surface, generating dynamic impingement (Fig. 2a). A 2.5-mm Kirschner wire (K-wire) was inserted anterolaterally into the humeral head at 30° angulation. This joystick technique enabled successful disimpaction through counterclockwise rotation combined with gentle inferolateral traction (Fig. 2b). Three high-strength FiberWire® sutures were passed through rotator cuff tendon-bone interfaces. Tension band suture configuration achieved anatomical reduction of comminuted fracture fragments (Fig. 2c). Suture limbs were then secured to pre-designed perforations on Pilos® locking plates. This innovative tendon-bone-plate triple-load fixation construct enabled anatomical restoration while maximally preserving rotator cuff insertion integrity (Fig. 2d). Intraoperative and post-operative radiographs demonstrated complete anatomical reduction of both dislocation and fracture (Fig. 3a and b).

Pendulum exercises were initiated on post-operative day 1 according to an accelerated rehabilitation protocol. Complete axillary nerve functional recovery was confirmed at post-operative day 6. Deltoid muscle contraction against gravity was achieved without compensatory movements. Active motion was regained at 3 weeks post-operatively. Guided passive mobilization was maintained during this transitional phase.
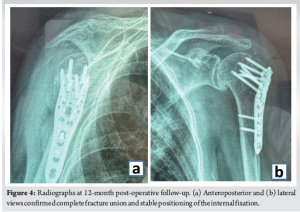
At the 12-month post-operative follow-up, the patient demonstrated excellent clinical outcomes. She reported no pain (15 points) and unrestricted performance in activities of daily living (20 points), including the ability to position her hand above her head. Range of motion assessment revealed active pain-free forward flexion of 110° (6 points)and abduction of 87°(4 points). Functional external rotation allowed her to comb her hair (7 points), and functional internal rotation reached the T7 spinous process level (10 points). Strength assessment indicated the ability to lift over 2 kg (21 points). The total Constant-Murley score was 83 points. Radiographic evaluation at 12 months (Anteroposterior and lateral views) (Fig. 4) confirmed complete fracture union and anatomical positioning of the internal fixation devices without migration. Furthermore, there were no signs of avascular necrosis of the humeral head or recurrent dislocation.
The management of irreducible anterior shoulder dislocations presents unique challenges. These challenges are particularly pronounced in the elderly osteoporotic population. A rare fracture pattern, the coronal split of the greater tuberosity, was observed in this case. This specific pathology was not represented in a recent systematic review on the topic [3]. This report, therefore, contributes to the literature by documenting this injury and proposing a tailored management framework. In such complex scenarios, paramount importance is placed on accurate pre-operative diagnosis. Two-dimensional radiographs are often insufficient for delineating the multifactorial barriers to reduction. A precise identification of the composite entrapment mechanism is enabled by early 3D-CT evaluation. An improved understanding of fracture morphology is furnished by these advanced imaging modalities. This principle is corroborated by recent studies, where systematic 3D-CT mapping was deemed crucial for enhanced surgical decision-making [4]. Soft tissue interposition, particularly of the LHBT, is also a well-documented cause of irreducibility that can be visualized [5,6]. Such detailed analysis is indispensable for planning a safe surgical approach. A “bone-preserving” philosophy was the foundation of our management framework. This principle is critical for achieving stable fixation in osteoporotic bone. The Kirschner-wire joystick technique was innovatively adapted for dislocation reduction. This approach aligns with modern principles for minimally invasive fracture stabilization [7]. A 2.5-mm K-wire was inserted into the head fragment, serving as a joystick. Controlled rotational force was then applied to disengage the osseous interlocking. This maneuver was performed with minimal traction, mitigating the risk of iatrogenic fractures in the fragile bone. Precise adjustment of varus/valgus alignment and anatomical reconstruction were thereby achieved [7].
Persistent debate surrounds the management of the LHBT. The decision to preserve the LHBT was based on dual biomechanical and vascular considerations. This choice is consistent with the present trend highlighted in recent literature. A shift away from simple tenotomy toward preserving the LHBT for its role in stability and reconstruction is now recognized [8]. Furthermore, LHBT preservation helps protect the accompanying arcuate artery [9]. The integrity of this vessel is vital for preventing post-operative osteonecrosis. An open approach with plate fixation was selected for this case. While arthroscopic techniques offer minimally invasive advantages for certain shoulder pathologies [10,11], their utility in managing such complex fracture-dislocations with significant fragment comminution and displacement is limited. The selection of an open approach was guided by the fracture’s complexity. This decision is strongly supported by recent comparative research. For greater tuberosity fractures with large displacement (>5 mm), open reduction with plate fixation is identified as the preferred method [12]. This evidence-based choice facilitated anatomical reduction under direct vision and provided the stability required for early rehabilitation. Finally, the transient axillary nerve neuropraxia resolved completely within 6 days post-surgery. This rapid recovery suggests a benefit from early, stable reduction and decompression. This observation aligns with the present understanding of managing such nerve injuries [13]. The limitation of this work is its nature as a single case report. However, by presenting a systematic framework supported by recent evidence, this report offers a valuable reference for managing this challenging clinical entity.
This case illustrates that low-energy mechanisms can result in irreducible anterior shoulder dislocations in elderly osteoporotic patients. The pathomechanical analysis revealed three critical factors: ① Osseous interlocking at the humeral head-glenoid interface, ② Incarceration of comminuted greater tuberosity fragments, ③ Dynamic entrapment of LHBT. Following failed closed reduction, early 3D-CT evaluation is recommended to delineate entrapment components. This approach assists in minimizing iatrogenic fracture risks associated with repeated manipulation attempts. The joystick technique was prioritized to achieve low-traction reduction. Preservation of LHBT integrity was emphasized to maintain humeral head vascular perfusion and anteroinferior stability. A biomechanically optimized suture-plate composite fixation was employed. This construct achieved comminuted fragment stability while preserving rotator cuff integrity. Complete functional restoration was achieved at 1-year follow-up (Constant-Murley score: 83). This outcome validated the feasibility of simultaneous anatomical and functional restoration. Future multicenter studies are warranted to establish evidence-based protocols for geriatric irreducible dislocations.
When closed reduction of an anterior shoulder dislocation fails in an elderly osteoporotic patient, clinicians must suspect a complex dual entrapment from a split greater tuberosity and interposed biceps tendon. Proceeding to early 3D-CT is critical to guide a bone-preserving open reduction, thereby avoiding iatrogenic fractures from further forceful manipulation and preserving vital stabilizing structures.
References
- 1. Patrick CM, Snowden J, Eckhoff MD, Green CK, Scanaliato JP, Dunn JC, et al. Epidemiology of shoulder dislocations presenting to United States emergency departments: An updated ten-year study. World J Orthop 2023;14:690-7. [Google Scholar]
- 2. Guler O, Ekinci S, Akyildiz F, Tirmik U, Cakmak S, Ugras A, et al. Comparison of four different reduction methods for anterior dislocation of the shoulder. J Orthop Surg Res 2015;10:80. [Google Scholar]
- 3. Liechti DJ, Shepet KH, Glener JE, Neumann EJ, Sraj S. A systematic review of acute irreducible shoulder dislocations in the 21st century. Orthop J Sports Med 2022;10(9):23259671221121633. [Google Scholar]
- 4. Mys K, Visscher L, Van Knegsel KP, Gehweiler D, Pastor T, Bashardoust A, et al. Statistical morphology and fragment mapping of complex proximal humeral fractures. Medicina (Kaunas) 2023;59:370. [Google Scholar]
- 5. Seo JB, Yoon SH, Yang JH, Yoo JS. Irreducible posterior fracture and dislocation of shoulder with massive rotator cuff tear due to incarceration of biceps tendon: A case report.J Orthop 2020;21:6-9.Published 2020 Feb 4. doi:10.1016/j.jor.2020.02.007 [Google Scholar]
- 6. Pantazis K, Panagopoulos A, Tatani I, Daskalopoulos B, Iliopoulos I, Tyllianakis M. Irreducible anterior shoulder dislocation with interposition of the long head of the biceps and greater tuberosity fracture: A case report and review of the literature. Open Orthop J 2017;11:327-34. [Google Scholar]
- 7. Beeres FJ, Quaile OM, Link BC, Babst R. Repositionstechniken bei minimal-invasiver stabilisierung proximaler humerusfrakturen [Reduction techniques for minimally invasive stabilization of proximal humeral fractures]. Oper Orthop Traumatol 2019;31:63-80. [Google Scholar]
- 8. Neculau DC, Avram GM, Kwapisz A, Scarlat MM, Obada B, Popescu IA. Long head of the biceps tendon versatility in reconstructive shoulder surgery: A narrative review of arthroscopic techniques and their biomechanical principles with video presentation. Int Orthop 2024;48:1249-56. [Google Scholar]
- 9. Determe D, Rongières M, Kany J, Glasson JM, Bellumore Y, Mansat M, et al. Anatomic study of the tendinous rotator cuff of the shoulder. Surg Radiol Anat 1996;18:195-200. [Google Scholar]
- 10. Gupta AP, Kumar P, Bhadani JS, Mukhopadhaya J, Matish M, Rajnish RK. Comprehensive evaluation and arthroscopic management of circumferential labral tears following traumatic first time shoulder dislocation: A case report and review. J Orthop Case Rep 2024;14:125-9. [Google Scholar]
- 11. Oeding JF, Schulz WR, Wang AS, Krych AJ, Taylor DC, Samuelsson K, et al. Comparing recurrence rates and the cost-effectiveness of arthroscopic labral repair and nonoperative management for primary anterior shoulder dislocations in young patients: A decision-analytic markov model-based analysis. Am J Sports Med 2024;52:3339-48. [Google Scholar]
- 12. Kim YJ, Ji JH, Park SE, Parikh D, Lee WJ. Comparison between arthroscopic suture anchor fixation and open plate fixation in the greater tuberosity fracture of the proximal humerus. Eur J Orthop Surg Traumatol 2024;34:621-31. [Google Scholar]
- 13. Hill JR, Lanier ST, Brogan DM, Dy CJ. Management of adult brachial plexus injuries. J Hand Surg Am 2021;46:778-88. [Google Scholar]