Anterior thoracic meningoceles and enterogenous cysts of the spine may be indistinguishable on radiologic evaluation; when one of these is considered likely in a patient, the possibility of the other must be considered in the differential diagnosis.
Dr. Apurve Parameswaran, Department of Orthopaedics, Medicover Hospitals, Hyderabad, Telangana, India. E-mail: doctorapurve@gmail.com
Introduction: Enterogenous cysts (also known as neurenteric cysts) are rare congenital lesions presumed to arise from an abnormal persistent communication between embryonic ectodermal and endodermal tissues. They may be symptomatic or asymptomatic, and generally have an insidious and prolonged clinical course. They are typically intradural and extramedullary in location. Very few cases of extramedullary enterogenous cysts have been reported in the literature, most of which were cranial. We present a rare case of an anteriorly situated extradural enterogenous cyst at the level of the thoracic spine, mimicking an isolated anterior thoracic meningocele on radiologic evaluation.
Case Report: A 4-year-old boy was referred to our spine surgery unit for the evaluation and management of an incidentally detected T1 vertebral anomaly. Magnetic resonance imaging revealed the presence of a focal defect over the right half of the T1 vertebral body, through which herniation of a fluid-filled sac into the pre- and right paravertebral regions was noted. A diagnosis of anterior thoracic meningocele was made, and surgery was advised. Following surgical exposure of the entire extent of the sac, needle aspiration to decompress the lesion was performed, which yielded a milky-colored viscous fluid, unlike cerebrospinal fluid. The likelihood of an enterogenous cyst was suspected. The lesion was excised at the level of the base of its peduncle, and the vertebral defect was closed using a small contoured plate. Histopathologic evaluation confirmed the presence of an enterogenous cyst.
Conclusion: Anterior thoracic meningoceles and enterogenous cysts of the spine may be indistinguishable on radiologic evaluation, and a definitive diagnosis may be reached only through histopathologic evaluation. The possibility of an enterogenous cyst must be considered in the differential diagnosis of meningoceles, and vice versa.
Keywords: Neurenteric cyst, enterogenous cyst, occult spinal dysraphism, meningocele, extradural cyst.
Enterogenous cysts, also known as neurenteric cysts, are rare congenital lesions lined by endoderm-derived gastrointestinal or respiratory epithelium, presumably arising from an abnormal persistent communication between embryonic ectodermal and endodermal tissues [1,2]. They represent 0.3–0.5% of all spinal masses [1,2]. Their clinical course is usually insidious and prolonged over months to years, though they may remain undetected until autopsy in patients who remain asymptomatic throughout life, or manifest in the neonatal period itself if associated with severe cardiopulmonary abnormalities [3,4]. More commonly, however, they present in the first four decades of life, with a male preponderance [3,5]. Enterogenous cysts can be found at any level of the central nervous system from the supratentorial compartment to the coccyx, though the majority have been reported to occur at the level of the cervical or thoracic spine [3,4]. They are typically intradural, extramedullary lesions [3]. We present a rare case of an anteriorly situated extradural enterogenous cyst at the level of the thoracic spine, mimicking an isolated anterior thoracic meningocele, in a 4-year-old child. The patient and his parents were informed that data concerning the case would be submitted for publication; they provided voluntary assent and informed consent, respectively, for the same.
A 4-year-old boy, born to non-consanguineous parents, was evaluated and treated by a pediatrician for three episodes of dizziness lasting a few seconds, during the preceding 7 months. He gave no history of headache, nausea, vomiting, blurred vision, fever, or loss of weight. During his diagnostic work-up, however, a wedge-shaped T1 vertebra was detected (Fig. 1). He was referred to our spine surgery unit for further evaluation and management of the same. On general physical examination, no dysmorphism or cutaneous stigmata of spinal dysraphism were noted. Examination of the cardiorespiratory system and the abdomen revealed no obvious abnormalities. Neurologic examination was also unremarkable with no signs of myelopathy or radiculopathy. His blood cell counts, serum inflammatory markers, serum electrolytes, electrocardiogram, and magnetic resonance imaging (MRI) of the brain were normal.
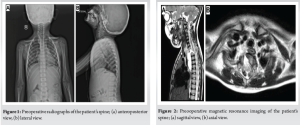
An MRI of his spine showed hypoplasia and a focal defect of the right half of the T1 vertebral body with an absent pedicle (Fig. 2), through which herniation of a fluid-filled sac (presumed to be dural) measuring 2.3 × 2.4 × 5.2 cm into the pre- and right paravertebral regions from the level of the T1 to T6 vertebral bodies was reported. Partial fusion of T1 and T2 vertebral bodies was noted. No evidence of spinal cord herniation into the sac was noted. Based on these findings, a diagnosis of an isolated anterior thoracic meningocele with intrathoracic herniation was made, and surgery was advised. Under general anesthesia, with the patient supine, a right-sided anterior cervico-thoracic approach was taken. With the assistance of a cardiothoracic surgeon, the manubrium sterni was split along the distal part of the approach. Surgical exposure was carried down to the level of the T5 vertebra. The full extent of the herniated sac was identified and dissected to the base (Fig. 3a).
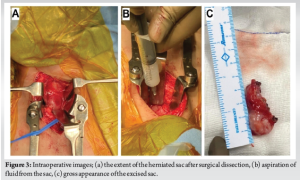
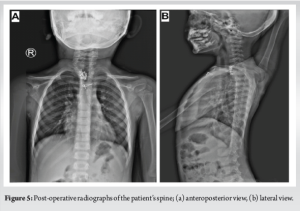
Needle aspiration of the sac was performed next to reduce its volume and facilitate excision. This procedure, however, yielded a milky-colored viscous fluid that did not appear like cerebrospinal fluid (Fig. 3b). At this point, it was evident that the lesion was not a meningocele, but more likely to be an enterogenous cyst. It was ligated at the level of its peduncle and was excised (Fig. 3c). The T1 vertebral defect was closed by fixing a small contoured maxillofacial Z-plate directly over its anterior opening. The rest of the surgery proceeded routinely. On histopathologic evaluation, the wall of the sac was found to be about 1.1 mm in thickness and was filled with mucus. The lining of the cyst comprised ciliated columnar epithelium or stratified cuboidal epithelium in different regions, overlying multi-layered smooth muscle (Fig. 4). Aggregates of mucus glands, ducts, variably sized blood vessels, benign mature adipocytes, lymphoid aggregates, and nerve bundles were found admixed with the muscular layer. No evidence of a granuloma or malignancy was noted. This confirmed the diagnosis of an enterogenous cyst. The child was advised to avoid strenuous activity in the immediate post-operative period. He recovered well and was asymptomatic with no signs of recurrence at 6 months following surgery (Fig. 5).

Intraspinal epithelium-lined cysts of presumed endodermal origin were described as “teratomatous cysts” by Kubie and Fulton in 1928, and “instestinomas” by Puusepp in 1934 [5-7]. They were subsequently called “neurenteric cysts” by Holcomb and Matson in 1954, and “enterogenous cysts” by Harriman in 1958 [8,9]. Several hypotheses have been proposed to explain the pathogenesis of these complex malformations, including failure of closure of the embryonic neurenteric canal connecting the endoderm and the developing neurectoderm, formation of accessory neurenteric canals, splitting of the proximally migrating notochord by remnants of the retreating primitive knot and subsequent herniation of endoderm through the orifice, formation and persistence of midline endo-ectodermal adhesions or malformations cephalad to the primitive knot, aberrations of notochordal intercalation and excalation, aberrant intercalation of the endoderm into the dorsal neurectoderm, and teratomatous origin from primordial germ cells [3,4,10,11]. The precise etiopathogenesis of these lesions, however, is still unclear. Although several authors describe enterogenous cysts as “tumors” [3,4,12,13], they are benign non-neoplastic lesions similar to hamartomas, and are considered to be a form of “occult spinal dysraphism” [2,14]. Despite frequently being associated with various congenital vertebral anomalies [2,4], they have no characteristic history or clinical findings; they may remain asymptomatic or may present with symptoms secondary to a mass effect or from an inflammatory reaction due to leakage of cyst contents [1,3]. Notwithstanding the considerable improvement in the detection of these lesions through MRI, definitive diagnosis of enterogenous cysts is seldom possible preoperatively, with histopathologic examination and the demonstration of columnar or cuboidal epithelial lining cells akin to gastrointestinal or respiratory linings – with or without cilia, mucus glands, and/or goblet cells – being the only reliable means to establish the same [3]. Indeed, the diagnosis of enterogenous cyst might only be made retrospectively following histopathologic examination in several instances [15]. Enterogenous cysts are rare lesions to begin with. Furthermore, approximately 90% of them are intradural and extramedullary in location, with the remaining 10% comprising extradural as well as intramedullary lesions [16]. An extensive literature search on the PubMed database revealed very few reports of extradural enterogenous cysts, most of which were cranial [17-20]. In addition, a purely extradural, dorsally placed, infected intraspinal thoracic-level neurenteric cyst with extension into the paraspinal space was reported by Savardekar et al. [21]. Our case report is unique on two counts. Firstly, it presents the findings and management of an anteriorly situated extradural enterogenous cyst of the spine in a 4-year-old child. Second, it presents the diagnostic challenge associated with preoperative recognition of the lesion consequent to the resemblance of its radiological appearance to that of a meningocele and the absence of a comparable literary precedent. Our patient initially presented with dizziness but no signs of compressive myelopathy, radiculopathy, or cutaneous stigmata of spinal dysraphism. His incidental MRI findings were consistent with an anterior upper thoracic meningocele, given the apparent communication of the cystic lesion with the spinal cord and the seeming isointensity of the contents of the cyst with cerebrospinal fluid. Accordingly, surgery was advised promptly, as is the current standard of care for symptomatic as well as asymptomatic meningoceles [22]. The intraoperative and histopathological findings, however, negated this supposition. We believe that the gradual progression of the patient’s enterogenous cyst resulted in its close posterior proximity with the pachymeninges, as well as anterior herniation through the pre-existing vertebral defect into the thoracic cavity, resulting in the radiologic appearance of the described phenomenon of thoracic herniation of an isolated anterior thoracic meningocele [23]. To the best of our knowledge, similar findings have not been reported in the past. Despite the slow progression of enterogenous cysts, they have the potential to eventually result in hypotonia, muscle wasting, and paraplegia or quadriplegia [4]. In some instances, enterogenous cysts have been reported to be associated with malignant transformation [24,25], calcification [16,26], and holospinal dissemination [27], thereby adding to the complexity of curative endeavours and rendering surgical management extremely challenging. In view of these considerations, we believe that early surgical intervention was undoubtedly appropriate for our patient. However, given the high probability of recurrence following subtotal resection of enterogenous cysts [12], the presence of vulnerable neurovascular structures in the vicinity of the lesion in our case, the redundancy of intraoperative exploration posterior to the peduncle of the lesion in light of the intraoperative findings, and the impracticability of obtaining clear histopathological “margins” as in true neoplasias, the patient was advised regular follow-up visits and serial MRI evaluation.
The detection of a spinal lesion was incidental in our patient. Radiologic evaluation was suggestive of an isolated anterior thoracic meningocele given the possibility of identical appearance of enterogenous cysts and meningoceles, and the lack of a comparable literary precedent. Intraoperative aspiration of the contents of the sac led to the initial suspicion of an enterogenous cyst, while histopathologic evaluation eventually confirmed this impression. Given that surgical intervention is the standard of care for both these conditions, surgical exploration and histopathologic evaluation are appropriate whenever either of these pathologies is suspected. However, the possibility of an enterogenous cyst must be considered in the differential diagnosis of meningoceles, and vice versa.
Meningoceles as well as enterogenous cysts can remain asymptomatic and may be detected incidentally during the evaluation of unrelated complaints. Both conditions require surgical intervention. However, a definitive diagnosis may be reached only through histopathologic evaluation, as they can appear similar on radiologic evaluation. When one of these conditions is suspected in a patient, the likelihood of the other should be considered in the differential diagnosis.
References
- 1.Menendez RH, D’Osvaldo DH, Vilarino A, Amante MF, Dillon HS. Neurenteric cyst of the ventral craniocervical junction: Case report and review of the literature. World Neurosurg 2019;125:257-60. [Google Scholar | PubMed]
- 2.Rauzzino MJ, Tubbs RS, Alexander E 3rd, Grabb PA, Oakes WJ. Spinal neurenteric cysts and their relation to more common aspects of occult spinal dysraphism. Neurosurg Focus 2001;10:1-10. [Google Scholar | PubMed]
- 3.Ergün R, Akdemir G, Gezici AR, Kara C, Ergüngör F. Craniocervical neurenteric cyst without associated abnormalities. Pediatr Neurosurg 2000;32:95-9. [Google Scholar | PubMed]
- 4.Cai C, Shen C, Yang W, Zhang Q, Hu X. Intraspinal neurenteric cysts in children. Can J Neurol Sci 2008;35:609-15. [Google Scholar | PubMed]
- 5.Liu CX, Meng B, Li YB, Bai H, Wu ZX. A rare case of thoracic spinal intradural extramedullary enterogenous cyst with acute onset: Case report and literature review. Ann R Coll Surg Engl 2019;101:e142-6. [Google Scholar | PubMed]
- 6.Kubie LS, Fulton JF. A clinical and pathological study of two teratomatous cysts of the spinal cord, containing mucus and ciliated cells. Surg Gynec Obstet 1928;47:297-311. [Google Scholar | PubMed]
- 7.Puusepp M. Variété rare de tératome, sousdural de la region cervicale (intestinome): Quadriplégie, extirpation, guérison complète. Rev Neurol 1934;2:879-86. [Google Scholar | PubMed]
- 8.Holcomb GW Jr., Matson DD. Thoracic neurenteric cyst. Surgery 1954;35:115-21. [Google Scholar | PubMed]
- 9.Harriman DG. An intraspinal enterogenous cyst. J Pathol Bacteriol 1958;75:413-9. [Google Scholar | PubMed]
- 10.Macdonald RL, Schwartz ML, Lewis AJ. Neurenteric cyst located dorsal to the cervical spine: Case report. Neurosurgery 1991;28:583-7. [Google Scholar | PubMed]
- 11.Bentley JF, Smith JR. Developmental posterior enteric remnants and spinal malformations: The split notochord syndrome. Arch Dis Child 1960;35:76-86. [Google Scholar | PubMed]
- 12.Vachhani JA, Fassett DR. Intramedullary neurenteric cyst associated with a tethered spinal cord: Case report and literature review. Surg Neurol Int 2012;3:80. [Google Scholar | PubMed]
- 13.Balasubramaniam S, Tyagi DK, Sawant HV. Intramedullary enterogenous cyst of the conus medullaris presenting as lower limb pain. J Craniovertebr Junction Spine 2011;2:46-8. [Google Scholar | PubMed]
- 14.Baek WK, Lachkar S, Iwanaga J, Oskouian RJ, Loukas M, Oakes WJ, et al. Comprehensive review of spinal neurenteric cysts with a focus on histopathological findings. Cureus 2018;10:e3379. [Google Scholar | PubMed]
- 15.El Ahmadieh TY, Sillero R, Kafka B, Aoun SG, Price AV. Isolated dorsal thoracic neuroenteric cyst with spinal cord compression: Case reports in pediatrics. World Neurosurg 2018;118:296-300. [Google Scholar | PubMed]
- 16.Joshi KC, Singh D, Suggala S, Mewada T. A rare case of solid calcified intramedullary neurenteric cyst: Case report and technical note. Asian J Neurosurg 2017;12:290-2. [Google Scholar | PubMed]
- 17.Fan T, Benaim E, Lee Diaz J, MacDonald C. Neurenteric cyst of the temporal bone: A case report. SAGE Open Med Case Rep 2021;9:2050313X211067913. [Google Scholar | PubMed]
- 18.Reddy RS, Vijayasaradhi M, Uppin MS, Challa S. A rare case of extradural neurenteric cyst with supratentorial and infratentorial extension. Acta Neurochir (Wien) 2010;152:1957-9 [Google Scholar | PubMed]
- 19.Basheer N, Kasliwal MK, Suri A, Sharma MC, Arora A, Sharma BS. Lateral extradural, supratentorial neurenteric cyst. J Clin Neurosci 2010;17:639-41. [Google Scholar | PubMed]
- 20.Inoue T, Kawahara N, Shibahara J, Masumoto T, Usami K, Kirino T. Extradural neurenteric cyst of the cerebellopontine angle. Case report. J Neurosurg 2004;100:1091-3. [Google Scholar | PubMed]
- 21.Savardekar A, Salunke P, Rane S, Chhabra R. Dorsally placed extradural infected neurenteric cyst in a two-year old with paraspinal extension. Neurol India 2012;60:129-31. [Google Scholar | PubMed]
- 22.Yun-Hai S, Nan B, Ping-Ping G, Bo Y, Cheng C. Is repair of the protruded meninges sufficient for treatment of meningocele? Childs Nerv Syst 2015;31:2135-40. [Google Scholar | PubMed]
- 23.Oner AY, Uzun M, Tokgoz N, Tali ET. Isolated true anterior thoracic meningocele. Am J Neuroradiol 2004;25:1828-30. [Google Scholar | PubMed]
- 24.Dunham CP, Curry B, Hamilton M. Malignant transformation of an intraaxial-supratentorial neurenteric cyst - case report and review of the literature. Clin Neuropathol 2009;28:460-6. [Google Scholar | PubMed]
- 25.Chu M, Wang L, Yu H, Li J, Lu D, Piao Y, et al. Meningeal carcinomatosis secondary to neurenteric cysts with malignant transformation: A case report. BMC Neurol 2022;22:433. [Google Scholar | PubMed]
- 26.Ziu M, Vibhute P, Vecil GG, Henry J. Isolated spinal neurenteric cyst presenting as intramedullary calcified cystic mass on imaging studies: Case report and review of literature. Neuroradiology 2010;52:119-23. [Google Scholar | PubMed]
- 27.Yasuda M, Nakagawa H, Ozawa H, Inukai C, Watabe T, Mizuno J, et al. Disseminated neurenteric cyst. J Neurosurg Spine 2008;9:382-6. [Google Scholar | PubMed]