Delayed anterior tibial artery pseudoaneurysm is a rare but important complication of tibial nailing, and early diagnosis with imaging, followed by minimally invasive endovascular treatment, can lead to excellent outcomes.
Dr. Murat Acar, Department of Radiology, Wake Forest University School of Medicine, Winston-Salem, North Carolina, United States. E-mail: macar@wakehealth.edu
Introduction: Intramedullary nailing is a widely accepted and effective treatment for tibial shaft fractures. Anterior tibial artery (ATA) pseudoaneurysms caused by interlocking screws are exceedingly uncommon, with only a few cases reported in the literature.
Case Report: We present the case of a 56-year-old male who developed worsening swelling and pain in his left lower extremity 8 months after undergoing intramedullary nailing for a tibial shaft fracture. Doppler ultrasound revealed an ATA pseudoaneurysm with characteristic imaging findings, which was confirmed by computed tomography angiography (CTA). The patient was treated with coil embolization of the ATA pseudoaneurysm, followed by surgical evacuation of the thrombus. The post-operative course was uncomplicated, and the patient recovered well. ATA pseudoaneurysm related to tibial nailing can be easily overlooked due to expected post-operative edema and swelling. Early detection through Doppler ultrasound and CTA is essential. Treatment options range from non-invasive methods to open surgery and endovascular interventions. In this case, a combination of coil embolization and surgical hematoma evacuation proved to be a minimally invasive and effective approach.
Conclusion: This case highlights the importance of considering rare vascular complications after tibial nailing. Timely diagnosis and endovascular treatment approaches can lead to successful outcomes.
Keywords: Tibial fracture, tibia nailing, interlocking screw, pseudoaneurysm, coil embolization.
Intramedullary nailing is a well-established and effective treatment for tibial shaft fractures, with a very low incidence of vascular complications. To date, only a few cases of anterior tibial artery (ATA) pseudoaneurysms linked to interlocking screws of intramedullary nails have been reported [1,2,3,4,5,6,7]. Here, we present a case of delayed diagnosis of an ATA pseudoaneurysm caused by a proximal interlocking screw, identified through comprehensive diagnostic imaging, including computed tomography angiography (CTA) and Doppler ultrasound. The condition was successfully managed with a combination of coil embolization and surgical evacuation of a large hematoma.
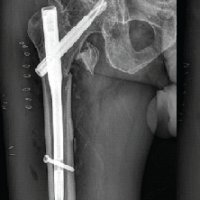
A 56-year-old male presented to the emergency department of our institution with worsening swelling and pain in his left lower extremity. Eight months prior, he had sustained fractures of the left mid-tibial shaft, proximal fibular shaft, and posterior malleolus after dropping a piece of plywood on his leg (Fig. 1a). Initial management involved closed reduction of the tibial shaft fracture with the application of a uniplanar external fixator, alongside open reduction and internal fixation of the posterior malleolus fracture. Subsequently, the tibial fracture was stabilized with intramedullary nailing, and the external fixator was removed. Additional blocking screws were placed proximally and distally to maintain alignment and prevent varus collapse. Two proximal interlocking screws were inserted in a medial-to-lateral direction using an outrigger jig (Fig. 1b). No significant bleeding or acute swelling was noted intraoperatively or in the immediate post-operative period. Routine follow-up examinations revealed swelling and stiffness, which were initially considered expected findings given the high-energy nature of the injury and extensive soft tissue involvement. A peripheral venous Doppler study was performed following external fixation and showed no evidence of thrombosis. However, the assessment was limited due to the presence of a large cutaneous wound and bandaging.
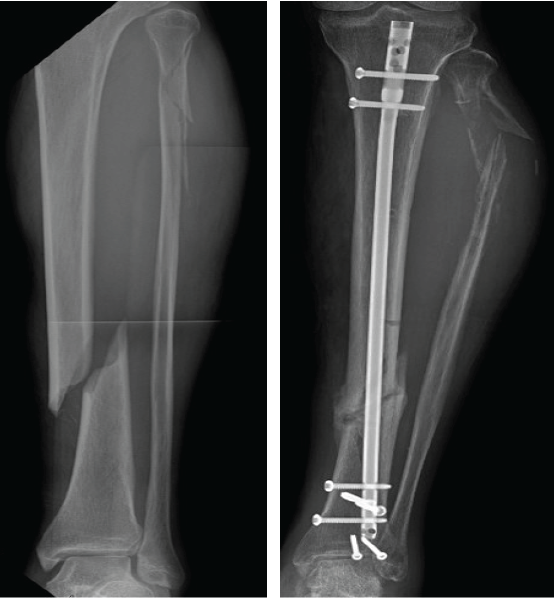
Figure 1: (a) Pre-operative radiograph reveals acute, mildly comminuted fractures of the mid/distal tibia and proximal fibular shaft. (b) Post-operative radiograph reveals intramedullary nailing of tibial shaft fracture in improved alignment and proximal fibular shaft fracture with increased displacement and apex posterior angulation. Upon the present presentation with the increased lateral calf pain and swelling, Doppler ultrasound revealed a large pseudoaneurysm of the ATA with the characteristic yin-yang sign (Fig. 2). CTA confirmed a pseudoaneurysm arising from the proximal ATA, surrounded by a large hematoma in the leg (Fig. 3). The largest aneurysmal sac measured approximately 8.7 × 10.4 × 16.1 cm, with an actively filling, non-thrombosed component measuring about 3.4 × 3.8 × 6.5 cm. Given the significant compressive symptoms caused by the hematoma, coil embolization of the ATA was performed to exclude blood flow into the pseudoaneurysm cavity. Selective catheterization of the left ATA was achieved through ultrasound-guided puncture of the right common femoral artery. Multiple Penumbra Ruby coils were deployed into the proximal and distal segments of the ATA, effectively sealing the pseudoaneurysm defect. A pre- and post-procedural angiogram demonstrated successful cessation of blood flow into the pseudoaneurysm cavity (Fig. 4a and b).
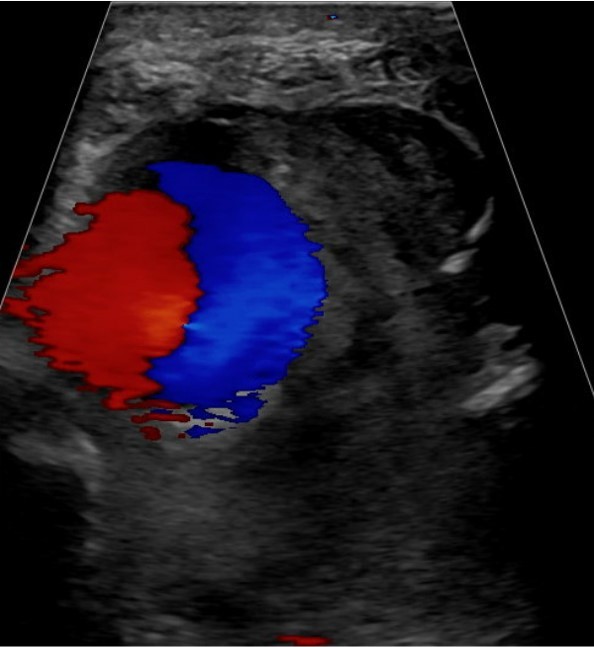
Figure 2: Color Doppler ultrasound shows a large, rounded structure with a classical yin-yang sign arising from the region of the anterior tibial artery.

Figure 3: Computed tomography angiography confirms the large pseudoaneurysm arising from the proximal anterior tibial artery, with a surrounding hematoma.
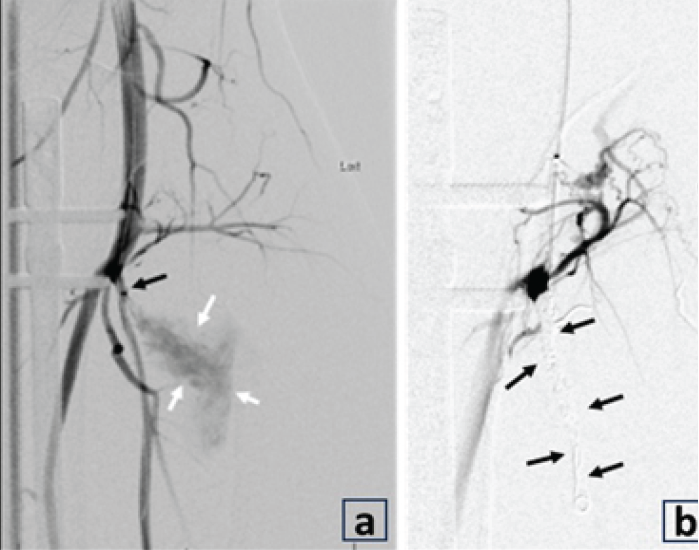
Figure 4: (a and b) Angiogram after selective catheterization of the left anterior tibial artery (ATA) demonstrates contrast filling of pseudoaneurysm (white arrows) and the origin at the proximal ATA (black arrow) near the screw. After coil embolization (b), the angiogram shows no contrast filling into the pseudoaneurysm cavity (black arrows), consistent with the successful cessation of blood flow into the pseudoaneurysm cavity. Following embolization, a left leg incision was made over the most prominent area of fluctuance, and the large hematoma cavity was entered. Suction and manual evacuation were used to remove approximately 250 cc of old thrombus along with the pseudoaneurysm capsule. A closed suction drain was placed in the evacuated cavity, and the incision was closed with interrupted nylon sutures. Sterile dressings were applied. The post-operative course was uncomplicated, and the patient recovered well. At the 3-month follow-up, CTA demonstrated post-procedural changes consistent with embolization of the ATA pseudoaneurysm. The distal ATA remained patent, with no evidence of recurrence. The aneurysm neck was successfully sealed, and there was a reduction in the size of the aneurysm sac (Fig. 5).

Figure 5: Coronal computed tomography angiography shows embolization of the anterior tibial artery pseudoaneurysm (black arrow) and patent distal anterior tibial artery (white arrow) without extravasation to suggest recurrence of the pseudoaneurysm.
Intramedullary nailing with interlocking screws is a reliable method for managing tibial fractures, with a low incidence of complications. Vascular complications, specifically pseudoaneurysm of the ATA following lateral-to-medial distal locking of an intramedullary nail for tibial shaft fractures, were first reported by Han et al., in 2004, with a few additional cases documented since then [1,2,4,5,6]. A pseudoaneurysm can develop in any artery but is most commonly seen in the femoral artery, particularly following cardiac catheterization. It occurs due to an injury to the adventitial layer of the artery, leading to the gradual leakage of blood into the surrounding tissue. Unlike a true aneurysm, which involves all three layers of the arterial wall, a pseudoaneurysm is characterized by a fibrous pseudocapsule that encases the leaking blood [1,8]. Although the exact timing of pseudoaneurysm formation is uncertain, we hypothesize that it likely occurred during drilling or the early phase of proximal interlocking screw fixation, with gradual enlargement over time. The growth rate of a pseudoaneurysm can vary widely depending on factors such as its etiology, anatomical location, and surrounding tissue. In smaller pseudoaneurysms, typically those measuring <3 cm, spontaneous thrombosis may occur, potentially leading to resolution without the need for intervention [7]. Symptoms of a pseudoaneurysm primarily arise from swelling and the mass effect exerted on surrounding nerves and vessels, causing pain, numbness, and muscle weakness [4]. Typically, most superficial pseudoaneurysms present as a painful, pulsatile mass and are relatively easy to diagnose. In contrast, deep pseudoaneurysms, as in this case following tibial nailing, are rare and often overlooked. They can be concealed by expected post-operative edema and soft tissue swelling. In this patient, the swelling and stiffness were initially attributed to normal healing after extensive cutaneous and soft tissue injury, delaying diagnosis and treatment. Doppler ultrasound is the preferred initial screening tool for assessing potential vascular and soft tissue complications. In this case, it revealed an ATA pseudoaneurysm with the characteristic “yin-yang” sign, indicating bidirectional blood flow within the pseudoaneurysm sac. These findings were subsequently confirmed by CTA. Various treatment options are available for pseudoaneurysms, including open surgery with arterial repair, reconstruction, or ligation, as well as minimally invasive methods such as ultrasound-guided compression, thrombin injection, and endovascular interventions such as stenting, coiling, or embolization. While surgical repair and endovascular stenting are typically reserved for pseudoaneurysms arising from large arteries, coiling is preferred for pseudoaneurysms of smaller arteries [8,9,10,11]. A review of the literature shows that management approaches for ATA pseudoaneurysms associated with tibial nailing have varied. Reported cases include non-invasive treatment with ultrasound-guided thrombin injection [6], coil embolization [3], and ATA embolization with coils following surgical hematoma evacuation [4]. Several other cases were managed surgically [1,2,5]. In the present case, the neck of the pseudoaneurysm was successfully closed using coiling as a minimally invasive and effective method. Because of the mass effect and neurovascular compression from the large thrombus, suction and manual evacuation were performed through a small leg incision.
This case highlights the importance of considering vascular complications in patients presenting with swelling and pain after tibial nailing. Prompt diagnosis and a tailored treatment approach can lead to successful outcomes.
ATA pseudoaneurysm is a rare but important vascular complication following tibial nailing that can mimic routine post-operative swelling. Clinicians should maintain a high index of suspicion in patients with persistent or worsening symptoms. Early imaging with Doppler ultrasound and CTA is essential for diagnosis. Minimally invasive treatment, such as coil embolization combined with surgical evacuation when necessary, can lead to effective resolution and favorable outcomes.
References
- 1. Han KJ, Won YY, Khang SY. Pseudoaneurysm after tibial nailing. Clin Orthop Relat Res 2004;418:209-12. [Google Scholar] [PubMed]
- 2. Greve F, Cronlein M, Beirer M, Kirchhoff C, Biberthaler P, Braun KF. Pseudoaneurysm of the anterior tibial artery after interlocking tibial nailing: An unexpected complication. Eur J Med Res 2016;21:36. [Google Scholar] [PubMed]
- 3. Park JJ, Perry LD, Tamburrini D, Kumar S. Successful coil embolization of a large anterior tibial artery pseudoaneurysm after open reduction internal fixation of a bi-condylar tibial plateau fracture. Am Surg 2023;89:3886-8. [Google Scholar] [PubMed]
- 4. Gahlot N, Kanojia RK. Anterior tibial artery pseudoaneurysm due to interlocking bolt of tibial nail: A case report and review. Acta Orthop Traumatol Turc 2017;51:77-83. [Google Scholar] [PubMed]
- 5. Inamdar D, Alagappan M, Shyam L, Devadoss S, Devadoss A. Pseudoaneurysm of anterior tibial artery following tibial nailing: A case report. J Orthop Surg (Hong Kong) 2005;13:186-9. [Google Scholar] [PubMed]
- 6. Hanson CG, Hanson LF. Non-invasive repair of an iatrogenic tibial artery branch pseudoaneurysm after intramedullary nailing. J Clin Orthop Trauma 2017;8 Suppl 2:S49-51. [Google Scholar] [PubMed]
- 7. Matsubara N, Fukuo Y, Yoshimura K, Kashiwagi H, Futamura G, Park Y, et al. A case of puncture-site giant pseudoaneurysm following recanalization therapy for acute ischemic stroke: Marked growth and rupture of a femoral artery pseudoaneurysm. J Neuroendovasc Ther 2021;15:366-72. [Google Scholar] [PubMed]
- 8. Pathinathan K, Sivakumaran D, Dimantha WH, Nishanthan AA, Chanaka KA, Munidasa D. Late-onset pseudoaneurysms of lower limb arteries following late complications of orthopaedic constructs – two cases and review of literature. Int J Surg Case Rep 2021;87:106457. [Google Scholar] [PubMed]
- 9. Luther A, Kumar A, Negi KN. Peripheral arterial pseudoaneurysms-a 10-year clinical study. Indian J Surg 2015;77 Suppl 2:603-7. [Google Scholar] [PubMed]
- 10. Kinoshita H, Hashimoto M, Hirayama J, Fujita K, Takeuchi Y, Iwasaki J, et al. Huge pseudoaneurysm of the femoral artery after internal fixation of femoral trochanteric fracture. Case Rep Orthop 2018;2018:3182643. [Google Scholar] [PubMed]
- 11. Raherinantenaina F, Rakotorahalahy RA, Andrianandraina MC, Rakoto Ratsimba HN, Rajaonanahary TM. [Management of traumatic and iatrogenic arterial pseudoaneurysms in a tropical environment]. J Med Vasc 2017;42:338-48. [Google Scholar] [PubMed]