Vitamin D status is a significant and modifiable determinant of fracture healing time in lower-limb fractures. Early detection and correction of deficiency may enhance union rates and reduce recovery duration.
Dr. Sujit Kumar Singh, Assistant Professor, Department of Orthopedics, ASJSATDS Medical College, Fatehpur, Uttar Pradesh, India Email drsujitkrsingh@gmail.com
Aim and Background: Vitamin D plays a central role in calcium–phosphate metabolism and bone healing. Deficiency is common among fracture patients and may contribute to delayed union, particularly in weight-bearing lower-limb fractures. The purpose of this study was to assess the relationship between lower limb fracture healing time and baseline serum Vitamin D levels.
Materials and Methods: A prospective, observational, multi-center study was conducted from January 2022 to December 2024. Adult patients with acute lower-limb fractures were enrolled. Within a week following the injury, baseline serum 25-hydroxyvitamin D levels were assessed. The levels of Vitamin D were categorized as adequate (>30 ng/mL), inadequate (20–30 ng/mL), or deficient (<20 ng/mL). Healing time was recorded clinically (pain-free weight bearing) and radiologically (radiographic union scale for tibial fractures score ≥12). Statistical analysis included correlation and regression models.
Results: A total of 120 patients (mean age 44.8 ± 13.2 years, M:F = 1.6:1) were included. The mean Vitamin D level was 21.6 ± 8.4 ng/mL; deficiency was present in 45.0%, insufficiency in 31.7%, and sufficiency in 23.3%. The mean healing time was 16.4 ± 3.8 weeks, with faster healing in sufficient patients (14.8 ± 2.9 weeks) compared to insufficient (16.7 ± 3.2 weeks) and deficient (17.9 ± 3.9 weeks) groups (P < 0.001). Vitamin D levels continued to be an independent predictor on regression analysis (β = −0.41, P < 0.001) and had a negative correlation with healing time (r = −0.62, P < 0.001).
Conclusion: Higher incidences of delayed union and longer healing durations were linked to lower baseline Vitamin D levels. Patients with lower limb fractures may have better results with routine screening and deficit repair.
Keywords: Vitamin D, fracture healing, lower-limb fractures, tibia fracture, bone metabolism.
Fracture healing is a coordinated biological process involving inflammation, repair, and remodeling phases, each of which depends on both local mechanical stability and optimal systemic conditions. By controlling osteoblastic activity and calcium-phosphate metabolism, Vitamin D plays a critical role in maintaining skeletal homeostasis, which in turn affects callus development and mineralization [1,2,3].
Patients with orthopedic injuries frequently have Vitamin D deficiency, and those with lower limb fractures are especially likely to have it [4,5,6]. According to reports, 50–80% of individuals who have fractures of the foot, ankle, tibia, or femur exhibit inadequate or deficient levels of serum 25-hydroxyvitamin D (25[OH]D) [4,7,8]. This deficiency has been associated with delayed callus maturation, impaired mineralization, and an increased risk of delayed union or non-union [3,6,9].
Clinical studies have explored this relationship with varying results. Brinker et al. identified Vitamin D deficiency as the most common metabolic abnormality in patients with fracture non-union [6]. Warner et al. found that lower perioperative Vitamin D levels correlated with poorer functional recovery after ankle fracture fixation [1]. However, Ettehad et al. found that Vitamin D levels decreased as fractures healed, indicating higher metabolic needs [8]. Furthermore, Smith et al. documented a high prevalence of deficiency in patients with foot and ankle trauma, emphasizing the need for early detection [4].
Recent randomized controlled trials have examined whether supplementation accelerates fracture union. Slobogean et al. reported that although high-dose Vitamin D did not significantly hasten radiographic union in acute tibial and femoral fractures, patients with severe deficiency tended to heal more slowly [2]. Systematic reviews echo these mixed findings, highlighting heterogeneity in study designs, fracture sites, baseline Vitamin D status, and dosing regimens [3,9].
Despite accumulating evidence, there remains limited data specifically correlating baseline Vitamin D levels with time to healing in lower-limb fractures. These fractures are subject to high mechanical loads during recovery, making timely union essential to restoring function and preventing complications, such as malunion, stiffness, and chronic pain. To provide information to support early screening and intervention efforts, this study was undertaken to assess the relationship between serum Vitamin D levels and fracture healing time in lower limb fractures.
This 2-year, multi-center, prospective, observational study was carried out between January 2022 and December 2024.
Study population
Individuals who were 18 years of age or older who had acute lower limb fractures that needed either non-operative or surgical treatment were eligible to be included. Only closed fractures of the femur, tibia, fibula, and ankle were included. Patients with pathological fractures, People with chronic kidney illness, liver disease, metabolic bone problems (apart from Vitamin D deficiency), or those on long-term corticosteroid therapy were not included.
Data collection
Age, sex, body mass index, occupation, and comorbidities were among the baseline demographics that were documented. Details of the fracture, such as anatomical site, side, mechanism of injury, and classification according to the AO/OTA system, were documented.
Evaluation of Vitamin D
Using a chemiluminescent immunoassay, serum 25-hydroxyvitamin D (25[OH]D) levels were assessed within a week of the injury. The state of Vitamin D was classified as:
- Deficient: <20 ng/mL
- Insufficient: 20–30 ng/mL
- Sufficient: >30 ng/mL.
Fracture healing assessment
Both clinical and radiographic methods were used to assess fracture healing. Clinical healing was characterized by the absence of discomfort at the fracture site and pain-free full weight bearing. The radiographic union scale for tibial fractures (RUST) score was used to assess radiological healing; a score of ≥12 was regarded as unified. Assessments were performed at 6-week intervals until union was confirmed. Weeks were used to measure the healing period between the date of the injury and the official union date.
Data analysis
Data were entered into a secure database and analyzed using statistical software. Depending on the data distribution, continuous variables were either expressed as a median with interquartile range or as mean ± standard deviation. Frequencies and percentages were used to represent categorical variables. Pearson’s or Spearman’s correlation coefficients were used to evaluate the relationship between Vitamin D levels and healing times. The Student’s t-test, analysis of variance, or their non-parametric counterparts were used for group comparisons. P < 0.05 was regarded as statistically significant.
The investigation comprised 120 patients with acute fractures of the lower limbs. The study population had a male-to-female ratio of 1.6:1 and an average age of 44.8 ± 13.2 years. The most frequent fracture site was the tibial shaft (42.5%), which was followed by the distal tibia/fibula (10.9%), ankle (28.3%), and femoral shaft (18.3%). The leading causes of injuries were automobile accidents (63.3%), falls (31.7%), and other mechanisms (5.0%). Table 1 provides a summary of baseline characteristics.
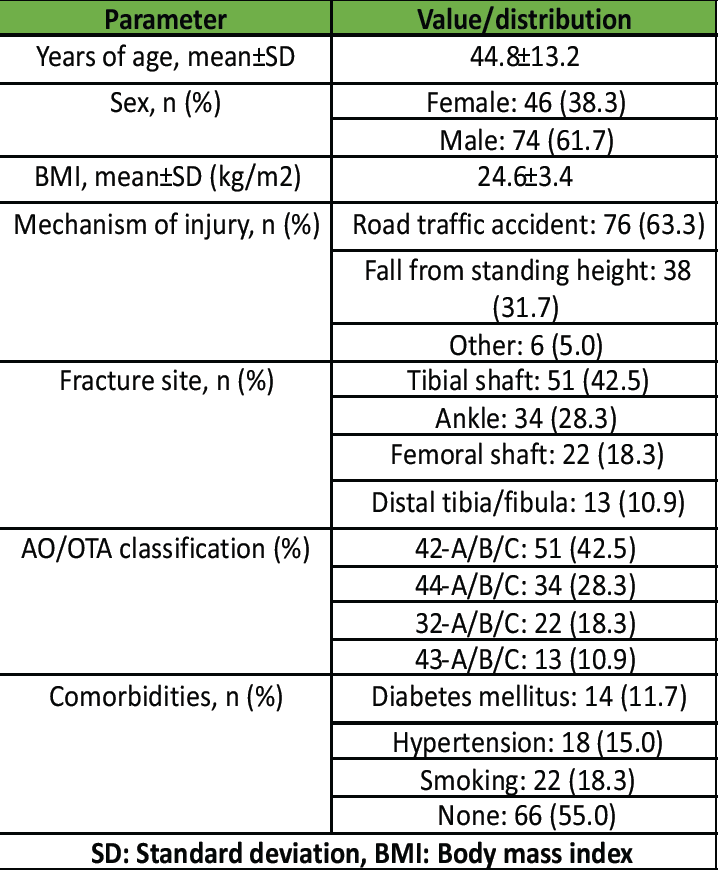
Table 1: Baseline demographic and injury characteristics of the study population. Values are expressed as mean±SD for continuous variables and as frequency (percentage) for categorical variables (n=120)
Vitamin D status distribution
The mean serum 25(OH)D level at baseline was 21.6 ± 8.4 ng/mL. 54 patients (45.0%) had Vitamin D deficiency (<20 ng/mL), 38 patients (31.7%) had insufficiency (20–30 ng/mL), and 28 patients (23.3%) had sufficiency (>30 ng/mL).
Healing time by Vitamin D status
The overall mean fracture healing time was 16.4 ± 3.8 weeks. Patients with sufficient Vitamin D levels healed significantly faster (14.8 ± 2.9 weeks) compared to those with insufficient (16.7 ± 3.2 weeks) and deficient levels (17.9 ± 3.9 weeks) (P < 0.001). These results are shown in Table 2.
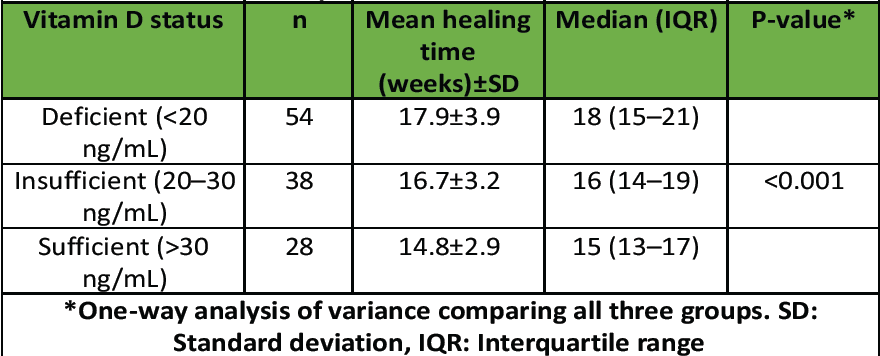
Table 2: Fracture healing time according to Vitamin D status. Healing time is expressed as mean±SD in weeks
Vitamin D levels and healing time correlation
Pearson’s correlation analysis revealed a significant negative correlation between serum Vitamin D levels and healing time (r = −0.62, 95% confidence interval [CI] −0.74–−0.48, P < 0.001), indicating that higher Vitamin D levels were associated with shorter healing durations (Fig. 1).
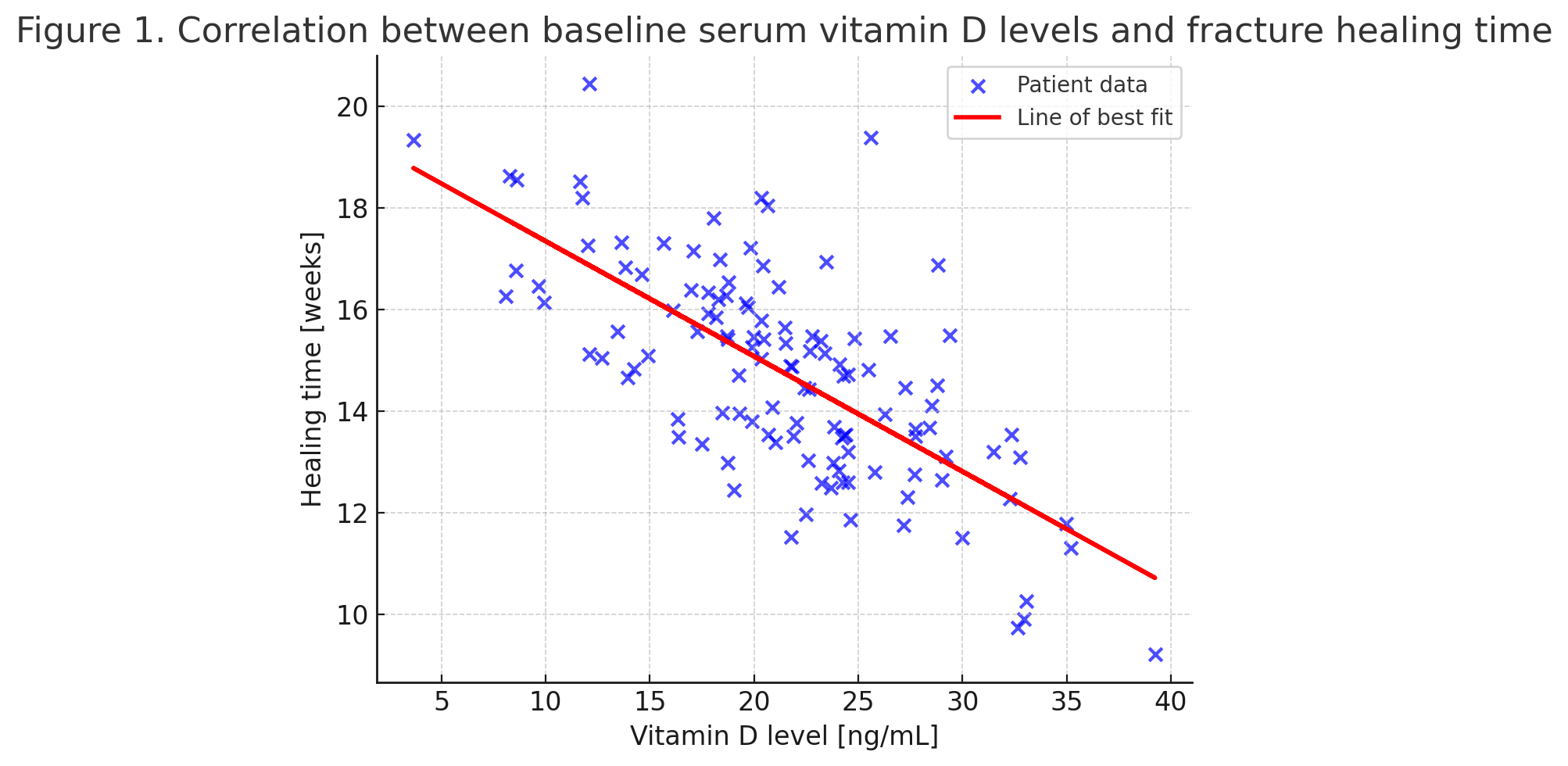
Figure 1: Scatter plot showing the correlation between baseline serum Vitamin D levels (ng/mL) and fracture healing time (weeks). The red line represents the line of best fit, demonstrating a significant negative correlation (r = −0.62, P < 0.001)
Multivariate linear regression adjusting for age, sex, body mass index (BMI), fracture type, and comorbidities confirmed that baseline Vitamin D level was an independent predictor of fracture healing time (β = −0.41, 95% CI −0.56–−0.27, P < 0.001), with a moderate effect size (Cohen’s f2 = 0.18).
Analysis of regression
Multivariate linear regression adjusting for age, sex, BMI, fracture type, and comorbidities confirmed that baseline Vitamin D level was an independent predictor of fracture healing time (β = −0.41, P < 0.001).
Union rates at follow-up
In 97.5% of patients, union was attained at 24 weeks. In comparison to the insufficient (2.6%) and sufficient (0%) groups, the deficient group had a substantially higher delayed union rate (7.4%) (P = 0.048) (Fig. 2).
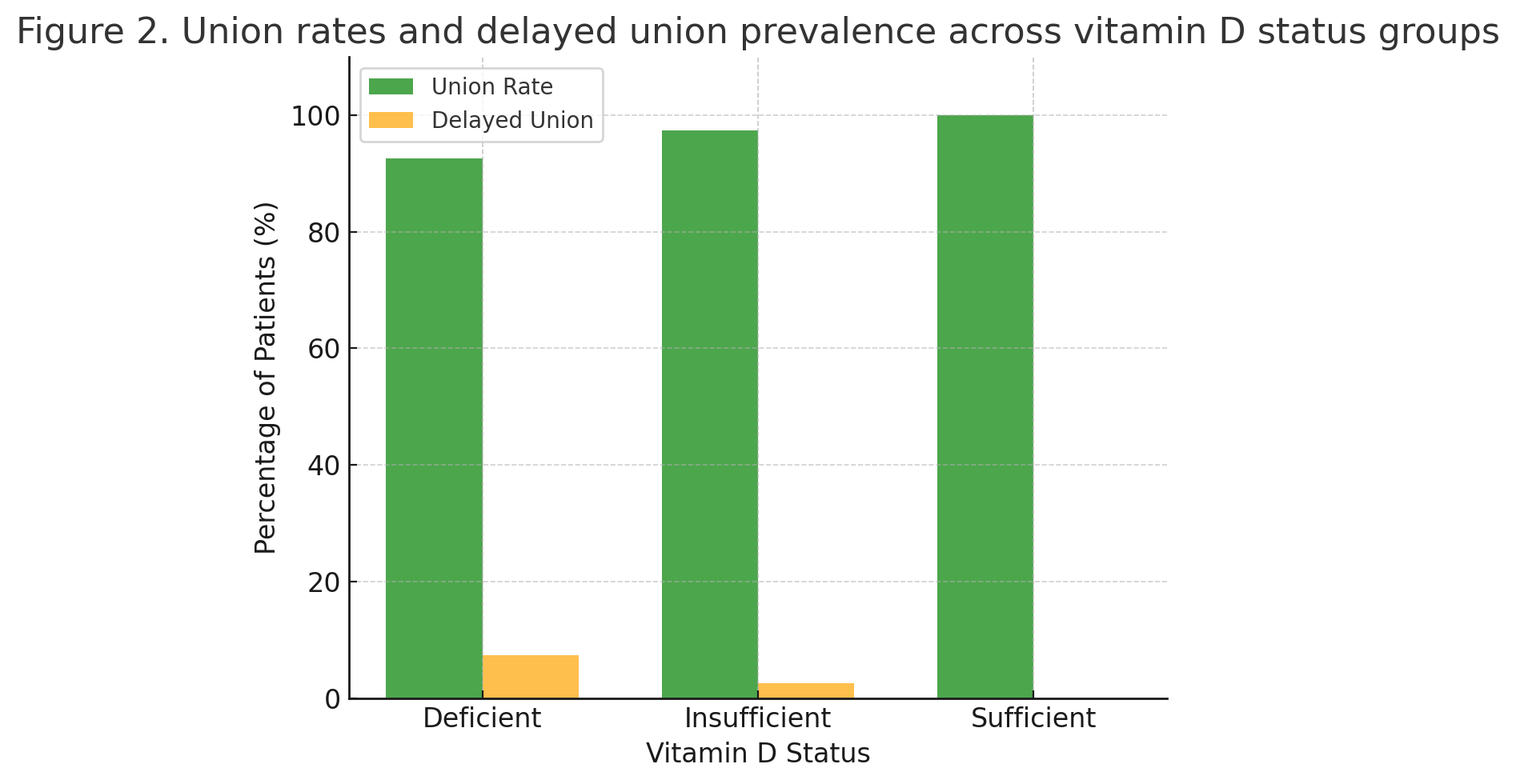
Figure 2: Bar chart comparing union rates and delayed union prevalence across Vitamin D status groups (deficient, insufficient, sufficient). Union rate is shown in green and delayed union prevalence in orange.
The relationship between baseline serum Vitamin D levels and fracture healing time in adult patients with lower limb fractures was assessed in this prospective multi-center investigation. The results demonstrated that patients with sufficient Vitamin D healed significantly faster than those with deficiency or insufficiency, and that serum Vitamin D level was an independent predictor of healing duration. These results are consistent with other studies that linked poor Vitamin D level to delayed fracture union and support the biological plausibility of Vitamin D as an associated but not definitively causal factor in fracture repair.
Our results imply that when evaluating patients who have had lower limb fractures, baseline Vitamin D levels should be taken into account. Identifying and correcting deficiency early could potentially shorten healing time, improve functional recovery, and reduce the incidence of delayed union. However, since this study did not directly evaluate supplementation, any recommendations for Vitamin D correction remain suggestive rather than evidence-based. Future research should focus on randomized controlled trials targeting deficient patients, with standardized dosing protocols and fracture-site-specific analyses. Serial measurements of Vitamin D during the healing process would also clarify whether declines occur consistently and whether ongoing supplementation is warranted. Larger studies with balanced subgroup sizes, especially patients with sufficient Vitamin D, are needed to strengthen statistical power. In addition, trials incorporating standardized supplementation protocols tailored to different fracture types will be essential to establish definitive causality and clinical guidelines.
Our cohort’s significant prevalence of Vitamin D insufficiency (31.7%) and deficiency (45.0%) is in line with previous research in populations with orthopedic injuries. Smith et al. reported deficiency rates exceeding 50% in patients with foot and ankle fractures [4], while Ribbans et al. identified widespread insufficiency among lower-limb trauma patients, particularly in older adults [5]. Brinker et al. found that low Vitamin D was the most frequent metabolic abnormality in patients with established fracture non-union [6], suggesting that early identification could be critical in preventing adverse healing outcomes.
Warner et al.’s research, which found that lower perioperative Vitamin D connected with worse functional recovery after ankle fracture fixation, is consistent with our finding that higher Vitamin D levels were linked to quicker healing times [1]. Similarly, Ettehad et al. documented a progressive decline in serum Vitamin D during fracture healing, implying an increased metabolic demand during bone regeneration [8]. The present study extends these findings by providing quantitative evidence of a moderate-to-strong negative correlation (r = −–0.62) between baseline Vitamin D and healing time. It was true when age, fracture type, BMI, and comorbidities were taken into account.
Vitamin D plays a variety of roles in bone repair. At the cellular level, 1,25-dihydroxyvitamin D stimulates osteoblastic development and improves intestinal calcium absorption, and modulates osteoclastic resorption in a manner that supports coupled bone remodeling [10,11]. In fracture healing, in addition to stabilizing callus structure and promoting the mineralization of woven bone, Vitamin D also has immunomodulatory properties that may maximize the inflammatory phase [12]. Experimental studies have shown that deficiency can impair chondrocyte maturation and reduce the biomechanical strength of the healing callus [13]. These biological pathways provide a plausible explanation for the delayed healing observed in deficient patients in our study.
Randomized controlled trials evaluating Vitamin D supplementation in fracture healing have produced mixed results. Slobogean et al., in a phase II trial involving tibial and femoral fractures, found no statistically significant reduction in time to union with high-dose Vitamin D3 supplementation; however, subgroup analysis suggested slower healing in severely deficient patients [2]. Gatt et al., in a recent systematic review, concluded that while supplementation may benefit patients with deficiency, the evidence remains heterogeneous due to variability in dosing regimens, fracture sites, and outcome measures [3]. Our study did not include supplementation as an intervention, but the observed correlation supports the rationale for targeted correction of deficiency in fracture patients.
The variability in trial outcomes may partly stem from differences in baseline Vitamin D status. Studies enrolling predominantly sufficient patients may fail to detect a benefit from supplementation, whereas those with high proportions of deficiency may observe a more pronounced effect [17]. This underscores the importance of screening fracture patients at presentation and considering early correction, particularly in high-risk groups, such as the elderly, those with limited sun exposure, or individuals with comorbidities affecting Vitamin D metabolism [18].
Risk of non-union and delayed union
According to our results, the Vitamin D-deficient group had a noticeably greater delayed union rate than the adequate group. This result is in line with Jensen et al.’s systematic study, which found Vitamin D insufficiency to be one of the possible risk factors for tibial shaft non-union [9]. Christianson et al. also reported that nutritional indicators, including low 25(OH)D, were frequently observed in non-union cases across multiple fracture sites [7].
Metabolic screening in non-union cases often reveals multiple abnormalities. However, Vitamin D insufficiency is still one of the most frequently found [6,14]. The relationship is likely multifactorial, with deficiency contributing to suboptimal callus mineralization and possibly influencing muscle strength and gait, thereby altering mechanical loading on the healing fracture [19].
Public health and epidemiological context
The high prevalence of deficiency in fracture patients mirrors broader epidemiological data. Bergin et al. and Sleiman et al. have highlighted the frequent occurrence of low Vitamin D in orthopedic cohorts, often exceeding rates seen in the general population [14,15]. This may be due to reduced outdoor activity, seasonal variation, and pre-existing comorbidities. Addressing this modifiable factor could have implications beyond fracture healing, potentially reducing fall risk and subsequent fractures through improved muscle function [16,20].
According to population-based research, older persons with greater serum 25(OH)D concentrations have improved lower-extremity function (Bischoff-Ferrari et al., for example) [16]. In addition, observational research by Maier et al. emphasized the importance of maintaining sufficient Vitamin D to support not only bone integrity but also muscular coordination, which is vital during post-fracture rehabilitation [21].
This study’s prospective design, multi-center recruitment, and standardized testing of Vitamin D within a week of injury are among its strong points. We reduced confounding and identified the association between Vitamin D status and healing time by eliminating patients with diseases known to impact bone metabolism. The use of both clinical and radiological criteria (RUST score) provided a robust assessment of fracture union.
Several limitations should be acknowledged. Although the total sample size was reasonable (n = 120), subgroup distribution was uneven, particularly the sufficient Vitamin D group (n = 28), which may have reduced statistical power for subgroup comparisons. First, although multi-center, the sample size may limit subgroup analyses, particularly for individual fracture types. Second, inter-observer variability in radiological scoring (RUST) was not assessed, which may have introduced bias into fracture healing evaluation. Third, serum Vitamin D levels were only measured at baseline and not serially during follow-up. Some patients may have corrected deficiency through diet, sunlight exposure, or supplementation during the healing period, which could have acted as a confounding factor. Fourth, although pathological fractures and metabolic bone diseases were excluded, comorbidities, such as diabetes mellitus and smoking, were not excluded. These factors may independently influence bone healing and complicate the interpretation of results. Sixth, the study did not include a supplementation intervention arm, which limits the ability to establish causality and to directly evaluate whether correction of deficiency accelerates fracture healing. Seventh, blinding of assessors during RUST scoring was not performed, which could have introduced observer bias. Eighth, other biochemical markers, such as calcium, parathyroid hormone, and nutritional indices, were not measured, which limits the ability to fully account for confounding metabolic influences. Ninth, the study did not include a supplementation intervention arm, which limits the ability to establish causality and to directly evaluate whether correction of deficiency accelerates fracture healing. Finally, as an observational study, causation cannot be established, and residual confounding cannot be fully excluded.
Implications for practice and future research
Our results imply that when evaluating patients who have had lower limb fractures, baseline Vitamin D levels should be taken into account. Identifying and correcting deficiency early could potentially shorten healing time, improve functional recovery, and reduce the incidence of delayed union. However, since this study did not directly evaluate supplementation, any recommendations for Vitamin D correction remain suggestive rather than evidence-based. Future research should focus on randomized controlled trials targeting deficient patients, with standardized dosing protocols and fracture-site-specific analyses.
A substantial inverse relationship between baseline serum Vitamin D levels and fracture healing time in lower limb fractures was found in this prospective multi-center investigation. Vitamin D insufficiency was linked to a higher risk of delayed union, while adequate Vitamin D levels were associated with quicker union. These results demonstrate the possible benefits of early Vitamin D screening for fracture patients and imply that prompt insufficiency therapy may potentially improve recovery, although the direct clinical benefit of supplementation remains uncertain without randomized controlled trial evidence. Routine incorporation of Vitamin D assessment into fracture management protocols could represent a simple, cost-effective strategy to optimize healing in this high-risk population.
Baseline Vitamin D assessment in patients with lower-limb fractures can help identify those at risk for delayed healing. Early correction of deficiency is a simple, low-cost intervention that may shorten recovery time and improve overall fracture outcomes.
References
- 1. Warner SJ, Garner MR, Nguyen JT, Lorich DG. Perioperative vitamin D levels correlate with clinical outcomes after ankle fracture fixation. Arch Orthop Trauma Surg 2016;136:339-44. [Google Scholar] [PubMed]
- 2. Slobogean GP, Mulpuri K, Cole PA, Pelletier ME, Levine MA, Beland M, et al. Effect of vitamin D3 supplementation on acute fracture healing: A phase II randomized controlled trial. JBMR Plus 2022;7:e10705. [Google Scholar] [PubMed]
- 3. Gatt T, Grech A, Borg M, Camilleri L, Zrinzo R, Formosa C. The effect of vitamin D supplementation for bone healing in fracture patients: A systematic review. JBJS Rev 2023;11:e2200035. [Google Scholar] [PubMed]
- 4. Smith JT, Halim AT, Palacios A, Koman LA, Karunakar MA. Prevalence of vitamin D deficiency in patients with foot and ankle trauma. Foot Ankle Int 2014;35:8-13. [Google Scholar] [PubMed]
- 5. Ribbans WJ, Aujla RS, Murphy A. Vitamin D and foot and ankle trauma: An individual and population perspective. Foot Ankle Surg 2019;25:255-9. [Google Scholar] [PubMed]
- 6. Brinker MR, O’Connor DP, Monla YT, Earthman TP. Metabolic and endocrine abnormalities in patients with nonunions. J Orthop Trauma 2007;21:557-70. [Google Scholar] [PubMed]
- 7. Christianson E, Ariyo O, Anderson JT, Taitsman LA, Castillo RC, O’Toole RV, et al. Nutritional indicators of bone nonunion: A systematic review. JBJS Rev 2024;12:e2300128. [Google Scholar] [PubMed]
- 8. Ettehad H, Mirbolook A, Mohammadi F, Mousavi M, Ebrahimi H, Fard SA. Changes in serum level of vitamin D during fracture healing. Trauma Mon 2014;19:e15266. [Google Scholar] [PubMed]
- 9. Jensen SS, Andresen AD, Nielsen M, Colov NP, Petersen MM. Risk factors for nonunion following surgically managed tibial shaft fractures: A systematic review. EFORT Open Rev 2022;7:552-64. [Google Scholar] [PubMed]
- 10. Holick MF. Vitamin D: Physiology, Molecular Biology, and Clinical Applications. 3rd ed. Totowa: Humana Press; 2013. [Google Scholar] [PubMed]
- 11. Christakos S, Dhawan P, Verstuyf A, Verlinden L, Carmeliet G. Vitamin D: Metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev 2016;96:365-408. [Google Scholar] [PubMed]
- 12. Takeda S, Yoshizawa T, Nagai Y, Yamato H, Fujita T. Genomic structure and vitamin D-dependent transcription of the mouse osteopontin gene. J Biol Chem 1999;274:7037-44. [Google Scholar] [PubMed]
- 13. Kurokawa T, Mizuno K, Ohkawa H. Effects of vitamin D3 on fracture healing in rats. J Bone Miner Res 1996;11:1027-33. [Google Scholar] [PubMed]
- 14. Sleiman A, Rahme E, Atallah N. Metabolic abnormalities underlying nonunion in the adult population. J Clin Orthop Trauma 2024;39:102064. [Google Scholar] [PubMed]
- 15. Bergin PF, Njus GO, Bostrom MP. The prevalence of metabolic and endocrine disturbances in fracture nonunion. J Orthop 2022;32:162-7. [Google Scholar] [PubMed]
- 16. Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, et al. Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged ≥60 y. Am J Clin Nutr 2004;80:752-8. [Google Scholar] [PubMed]
- 17. Gorter EA, Krijnen P, Schipper IB. Vitamin D status and adult fracture healing. J Clin Orthop Trauma 2016;7:183-7. [Google Scholar] [PubMed]
- 18. Aspray TJ, Bowring C, Fraser W, Gittoes N, Javaid K, Macdonald H, et al. National osteoporosis society vitamin D guideline summary. Age Ageing 2014;43:592-5. [Google Scholar] [PubMed]
- 19. Holick MF, Chen TC. Vitamin D deficiency: A worldwide problem with health consequences. Am J Clin Nutr 2008;87:1080S-6. [Google Scholar] [PubMed]
- 20. Ceglia L. Vitamin D and skeletal muscle tissue and function. Mol Aspects Med 2008;29:407-14. [Google Scholar] [PubMed]
- 21. Maier GS, Horas K, Seeger JB, Roth KE, Kurth AA, Maus U. The role of vitamin D and vitamin D deficiency in orthopaedics and traumatology-a narrative overview of the literature. Ann Transl Med 2021;9:826. [Google Scholar] [PubMed]