Ochronosis should be suspected in joint degeneration with pigmentation and intervertebral disk calcification findings.
Dr. Kumar Parth, Department of Orthopaedics, Seth Gs and Kem Hospital, Mumbai, Maharashtra, India. E-mail: k23parth@gmail.com
Introduction: Alkaptonuria is a rare autosomal recessive metabolic disorder caused by deficiency of homogentisic acid (HGA) oxidase, leading to the accumulation of HGA. The polymerized oxidation products of HGA deposit in connective tissues, a condition known as ochronosis. These deposits primarily affect cartilage and joints, resulting in progressive degeneration. Clinical manifestations typically appear after the age of 30 and include dark urine, bluish-black connective tissue pigmentation, and early-onset arthritis, especially of the spine and large joints.
Case Report: A 75-year-old female presented with right hip and wrist fractures following a fall. She had a 15-year history of stooped posture and a family history of similar symptoms. Radiographs revealed a transcervical femur fracture, distal radius fracture, and calcified intervertebral disks with kyphotic spinal deformity. Routine labs were within normal limits. During hip surgery, blackish discoloration of the femoral head and acetabulum was observed. Similarly, the flexor carpi radialis tendon appeared black during wrist surgery. Clinical re-evaluation revealed black scleral pigmentation and bluish-black ear cartilage. A urine HGA test confirmed ochronosis. HLA-B27 testing was negative, excluding seronegative spondyloarthropathies. Post-operative recovery was uneventful.
Conclusion: This case highlights the importance of considering ochronosis in elderly patients presenting with joint degeneration and intervertebral disk calcification. Characteristic pigmentation observed intraoperatively should prompt further investigation. Early recognition is crucial to differentiate from other degenerative conditions and guide appropriate management. Clinicians should maintain a high index of suspicion, particularly when supported by clinical history and radiological findings.
Keywords: Alkaptonuria, ochronosis, pigmentation.
Alkaptonuria is a rare autosomal recessive metabolic disorder characterized by the deposition of homogentisic acid (HGA) in connective tissue [1]. This results from a deficiency of HGA oxidase, an enzyme involved in the catabolism of tyrosine and phenylalanine [2]. In alkaptonuria, ochronotic pigment is deposited in connective tissues, especially cartilage. An acidic environment induces an inflammatory response in joints and disrupts articular cartilage metabolism, promoting cartilage degeneration [1].
The three major features of alkaptonuria are:
- Dark urine or urine that darkens on standing,
- Ochronosis (bluish-black pigmentation in connective tissue), and
- Arthritis of the spine and larger joints.
Ochronosis can occur in tendons, ligaments, sclera, heart valves, blood vessel intima, and the skin [3]. The irreversible binding of homopolymeric oxidation products of HGA to collagen leads to degenerative changes in connective tissue structure [4]. Ochronosis usually appears after the age of 30 and, over time, causes black and brittle bones and cartilage, and early-onset osteoarthritis [5]. Patients typically present in their 5th decade of life with back pain and arthritic changes in the hips and knees. Biochemical diagnosis is based on detecting significant levels of HGA in the urine. Molecular diagnosis involves identifying biallelic pathogenic variants in the homogentisate 1,2-dioxygenase (HGD) gene [6].
A 75-year-old female presented to the emergency department with an alleged history of a slip and fall, sustaining injuries to the right hip and right wrist. Radiographic evaluation of the right hip revealed a transcervical femur fracture, and imaging of the right wrist showed an extra-articular distal radius fracture (Fig. 1).
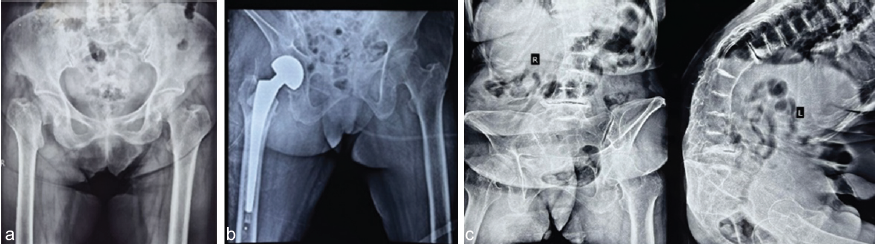
Figure 1: (a) Pre-operative X-ray showing right transcervical neck of femur fracture. (b) Post-operative X-ray showing right cemented bipolar hemiarthroplasty. (c) X-ray of spine suggestive of intervertebral disk calcification and degenerative changes.
The patient reported walking with a stooped posture for the past 15 years. She also had a family history of her parents walking with a stooped posture. Radiographic evaluation of the spine demonstrated calcification of intervertebral disks and degenerative changes, resulting in severe angular kyphotic deformity (Fig. 2).
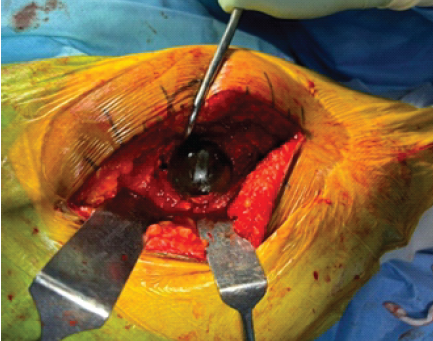
Figure 2: Ochronotic deposits in joint cartilage found intraoperatively.
Routine laboratory investigations were within normal limits. A cemented bipolar hemiarthroplasty of the right hip was performed. Intraoperatively, upon opening the hip joint capsule, blackish discoloration of the femoral head and acetabular cavity was noted. During volar plating for the distal radius fracture, the flexor carpi radialis tendon appeared black (Fig. 3).
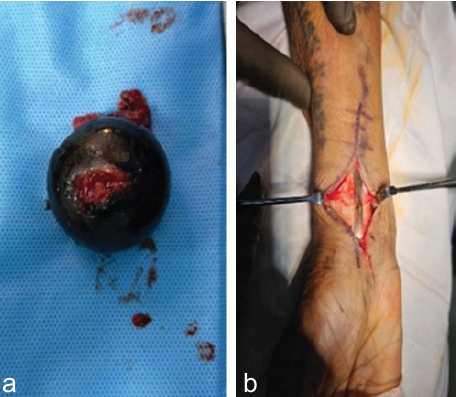
Figure 3: (a) Intraoperative resected portion of femoral head. (b) Intraoperative finding showing blackening of flexor carpi radialis tendon.
Upon re-examination, the patient was found to have blackish scleral pigmentation and bluish-black discoloration of the ear cartilage. A urine HGA test confirmed ochronosis. HLA-B27 testing was negative, ruling out seronegative arthropathies. Bilateral knee radiographs revealed osteoarthritic changes. The patient progressed well postoperatively.
This case emphasizes the importance of considering ochronosis in patients presenting with early-onset joint degeneration and intervertebral disk calcification, especially when intraoperative findings reveal characteristic pigmentation. Although often asymptomatic until joint involvement, ochronosis can mimic other degenerative conditions, such as ankylosing spondylitis. However, hallmark signs like connective tissue pigmentation aid in diagnosis. Current treatments, including nitisinone and dietary modifications, may reduce HGA levels but show limited effectiveness in reversing degenerative changes. This case is rare in that ochronosis was identified incidentally during surgery. Clinicians should include ochronosis in the differential diagnosis of intervertebral disk calcification [7]. It can be distinguished from ankylosing spondylitis by evaluating the sacroiliac joints and HLA-B27 status. Diagnosis is confirmed through quantitative measurement of urinary HGA and mutation analysis of the HGD gene. However, routine genetic testing remains controversial due to cost and limited impact on treatment. The exact mechanism of cartilage destruction remains unclear. HGA oxidation produces benzoquinone acetic acid, which inhibits lysine hydroxylase, impairing collagen fiber cross-linking [8]. Ligament degradation reduces joint stability, further aggravating cartilage damage. At present, there are no drugs proven to reverse ochronotic degeneration. Nitisinone, which inhibits 4-hydroxyphenylpyruvate dioxygenase (an upstream enzyme in tyrosine metabolism), shows promise and is approved for hereditary tyrosinemia. However, its role in reversing ochronotic arthropathy is yet to be confirmed [9,10]. Vitamin C can suppress urinary excretion of benzoquinone acetic acid, though its long-term benefits remain unproven. Restricting tyrosine and phenylalanine intake may reduce HGA levels, but risks nutritional deficiencies. This case underlines the importance of understanding the pathological mechanisms of ochronotic arthropathy, recognizing its clinical signs, and conducting thorough patient and family history assessments.
This case report highlights the importance of recognizing ochronosis in patients with joint degeneration and intervertebral disk calcification, particularly when intraoperative findings reveal characteristic pigmentation of cartilage and tendons. Early recognition and diagnosis are essential to guide appropriate management and avoid misdiagnosis.
Ochronosis should be considered in patients with early-onset joint degeneration, spinal disk calcification, and pigmentation of connective tissues observed intraoperatively. Awareness of this rare metabolic disorder is crucial to avoid misdiagnosis with other arthropathies. Diagnostic confirmation through urinary HGA testing and recognition of characteristic signs can guide appropriate management and help prevent further joint deterioration.
References
- 1. Garrod AE. The incidence of alkaptonuria: A study in chemical individuality. 1902. Mol Med 1996;2:274-82. [Google Scholar] [PubMed]
- 2. Ranganath LR, Norman BP, Gallagher JA. Ochronotic pigmentation is caused by homogentisic acid and is the key event in alkaptonuria leading to the destructive consequences of the disease-a review. J Inherit Metab Dis 2019;42:776-92. [Google Scholar] [PubMed]
- 3. Wu K, Bauer E, Myung G, Fang MA. Musculoskeletal manifestations of alkaptonuria: A case report and literature review. Eur J Rheumatol 2018;6:98-101. [Google Scholar] [PubMed]
- 4. Chang SS, Ek ET, Pliatsios V. Black bones: A case of incidental discovery of ochronotic arthropathy. Med J 2009;190:390. [Google Scholar] [PubMed]
- 5. Hamdi N, Cooke TD, Hassan B. Ochronotic arthropathy: Case report and review of the literature. Int Orthop 1999;23:122-5. [Google Scholar] [PubMed]
- 6. Santos J, Silva M, Silva E, et al. Ochronotic arthropathy: Case report and review of the literature. Acta Reumatol Port 2018;43:141-5. [Google Scholar] [PubMed]
- 7. Taylor AM, Boyde A, Wilson PJ, Jarvis JC, Davidson JS, Hunt JA, et al. The role of calcified cartilage and subchondral bone in the initiation and progression of ochronotic arthropathy in alkaptonuria. Arthritis Rheum 2011;63:3887-96. [Google Scholar] [PubMed]
- 8. Ventura-Ríos L, Hernández-Díaz C, Gutiérrez-Pérez L, Bernal-González A, Pichardo-Bahena R, Cedeño-Garcidueñas AL, et al. Ochronotic arthropathy as a paradigm of metabolically induced degenerative joint disease. A case-based review. Clin Rheumatol 2016;35:1389-95. [Google Scholar] [PubMed]
- 9. Ranganath LR, Timmis OG, Gallagher JA. Progress in alkaptonuria-are we near to an effective therapy? J Inherit Metab Dis 2015;38:787-9. [Google Scholar] [PubMed]
- 10. Arora A, Asnake G, Pandav K. Total Knee Arthroplasty in Ochronosis: A Rare Condition. Cureus. 2023 Jan 8;15(1):e33523. Doi: 10.7759/cureus.33523.. PubMed PMID: 36779093. [Google Scholar] [PubMed] [CrossRef]











