Robotic-assisted TKA with functional alignment using the CUVIS system provides superior early outcomes in valgus knees by achieving optimal gap balancing, reducing soft tissue releases, and preserving native knee phenotype compared to conventional mechanically aligned TKA.
Dr. Adarsh Krishna K Bhat, Department of Orthopaedic Surgery, Apollo Hospitals, Bengaluru, Karnataka, India. E-mail: adarshbhat118@gmail.com
Introduction: The robotic-assisted total knee arthroplasty (RA-TKA) facilitates real-time intra-operative balance assessment and accurate component positioning customized to the patient’s ligamentous behavior, enhancing procedural accuracy and precision. Preliminary findings suggest RA-TKA, using fully autonomous computed tomography based systems, such as Cuvis, result in better short-term outcomes and improved patient-reported outcome measures. Coronal plane alignment of the knee classification aids to decide pre-arthritic phenotype of the knee and soft tissue balance judgment.
Materials and Methods: This investigation was conducted as a retrospective matched-cohort observational study. We retrospectively analyzed a matched group of patients to compare RA TKA with functional alignment (n = 26) and mechanically aligned conventional-TKA (CM-TKA) (n = 24) in individuals with a valgus deformity Ranawat grade 1 and 2. The evaluation included radiographic assessments and PROMs over a 6-month period. The Western Ontario and McMaster University Osteoarthritis Index score and Oxford Knee Score (OKS) were used to determine the outcomes.
Results: The RA TKA cohort showed faster recovery than CM TKA patients. The RA TKA cohort required less soft tissue releases (P = 0.010). At the 3-month follow-up, there was a substantial reduction in pain in the RA TKA cohort (19.73 ± 2.38 vs. 25.71 ± 3.96, P = 0.000). However, over 6 months, pain reduction was found to be similar in both groups (13.27 ± 1.99 vs. 13.21 ± 2.04, P = 0.281). The improvement in OKS in RA TKA cohort was significant at 3 months (33.96 ± 3.88 vs. 31.04 ± 2.79, P = 0.006) and at 6 months (39.77 ± 2.97 vs. 36.46 ± 3.18, P = 0.136), and improved ROM in both groups (111.25 ± 13.29 vs. 116.96 ± 9.31, P = 0.083), with improvement in flexion (12.73 ± 5.85 vs. 7.08 ± 10.41, P = 0.210) in RA TKA compared to the CM-TKA cohort.
Conclusion: The CUVIS robotic system leads to optimum gap balancing throughout the range of motion, less soft tissue release, less post-operative pain, and improved function in short-term follow-up with optimum patella tracking in valgus knees.
Keywords: Robotic arthroplasty, knee arthroplasty, valgus deformity, functional alignment, Coronal plane alignment of the knee classification
The success of total knee arthroplasty (TKA) depends on precise component placement across all planes to ensure alignment and soft tissue balance [1]. Addressing valgus deformity during TKA involves specific technical challenges, notably in ligamentous balancing, lateral tibial plateau defects, external rotation deformity of the tibia, and is linked to poorer post-operative outcome and a higher revision risk compared to varus or neutral alignment [2,3,4]. In recent times, robotic assisted TKA (RA-TKA) has gained significant traction as an advanced technology. RA-TKA facilitates real-time intraoperative balance assessment and accurate component positioning customized to the patient’s ligamentous behavior, enhancing procedural accuracy and precision [5]. Recent advancements have introduced systems that enable the dynamic and continuous measurement of medial and lateral gaps throughout the full range of knee motion. One of such systems is the CUVIS® (Curexo Inc., South Korea). With the increasing adoption of RA-TKA among orthopedic surgeons, recent research supports its application in handling complex cases, such as valgus deformity [6,7]. A lot of data are available while comparing outcomes between RA-TKA and mechanically aligned conventional TKA (CM-TKA) in the varus deformity patient population. However, there is a paucity of studies assessing differences in clinical outcomes between patients who have pre-operative valgus deformity. This study aims to assess the post-operative outcomes between RA-TKA and CM-TKA in valgus coronal deformity. Our hypothesis was better outcomes with RA-TKA with functional alignment (FA) in the setting of valgus deformity using Cuvis robotic arthroplasty system, optimum ligamentous balance throughout range of motion (ROM), lesser soft tissue releases, improved ROM with early recovery, that is, improved patient-reported outcome measures (PROMs) Western Ontario and McMaster universities osteoarthritis index (WOMAC) score and Oxford Knee Score (OKS).
Ethics
With the principles of the Declaration of Helsinki (no. 2021-38), the study was held from November 1, 2023, to December 27, 2024, with the prior consent of all patients. Institutional Ethics Committee approval was taken September 27th, 2023 (Approval No: 159/2023).
Participants
A total of 702 patients who undergone TKA after failed non-operative management were screened retrospectively for possible inclusion. A total of 68 consecutive patients having knee osteoarthritis with valgus deformity (incidence 9.04%) were planned for TKA by a single senior surgeon with extensive experience in arthroplasty. The inclusion criterion was patients undergoing primary TKA for the treatment of knee osteoarthritis with valgus deformity – Ranawat Grade 1 and 2. The exclusion criteria were patients with varus deformity, ligamentous instability requiring a constrained condylar knee TKA design, the valgus deformity Ranawat Grade 3, flexion contracture >15° and those patients who did not complete the data set of PROMs and irregular follow-ups. After exclusion, 50 patients (26 in RA-TKA cohort and 24 in CM-TKA cohort) were included in our study. The design of the study is a retrospective matched-cohort observational study.
Pre-operative planning and imaging
All patients underwent pre-operative X-ray knee AP/Lateral/Skyline views, Alignment-X-ray of lower limbs in standing to evaluate knee alignment and assess the extent of deformities. The patients were classified according to Ranawat Classification for valgus knee deformity [8] and planned for surgery. The hip-knee-ankle angle (HKA), Lateral-distal-femoral angle (LDFA), Medial-distal-femoral angle, medial-proximal-tibial angle (MPTA) were calculated. All patients were classified according to coronal plane alignment of the knee (CPAK) phenotypes [9]. The Joint line obliquity (JLO) was derived after the addition of MPTA and LDFA [9].
Robotic system
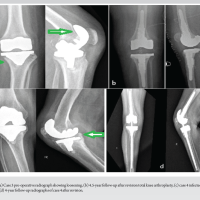
The patients in the RA-TKA cohort underwent a low-dose computed tomography (CT) scan additionally. The CT scans were transferred to advanced planning software (J-Planner), providing a three-dimensional visualization of the knee anatomy. The planning software aided in determining the optimal levels of bone resection and sizing of TKA components, necessary to achieve FA. Intraoperative mediolateral gaps were assessed by stretching ligaments in varus and valgus stress in both extension and flexion. Using a RA system (CUVIS® robotic joint system), the cuts were performed incorporating principles of FA for optimum ligamentous balance [10]. The final alignment did not exceed 3° off the neutral in the coronal plane or more than 2° of rotational change compared to the surgical epicondylar axis. The residual ligamentous balance was then achieved according to Ranawat inside-out lateral release technique [8], same as that of CM-TKA (Fig. 1).
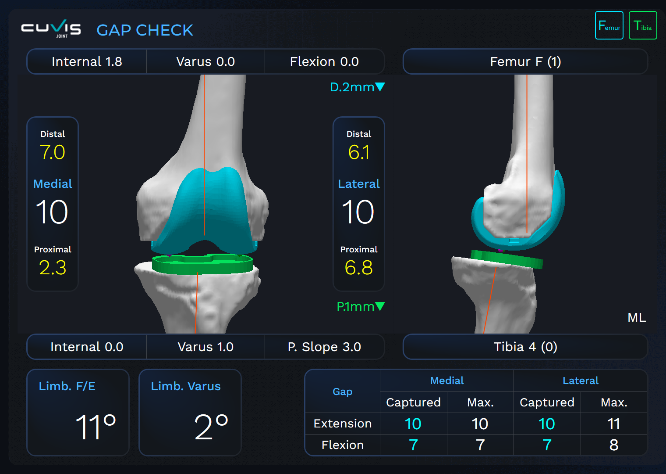
Figure 1: Balanced mediolateral gaps after intra-operative adjustments.
Surgical technique
The patients underwent a medial parapatellar arthrotomy. The tourniquet was used only at the time of cementing and final implantation. The femoral and tibial bony cuts and soft tissue releases were performed according to gap balancing techniques and mechanical alignment in CM-TKA [8], whereas, in RA-TKA, the cuts were decided as per FA principles and considering the native JLO. The data of soft tissue release was recorded for reference. All participants received a cemented TKA with a posterior stabilized tibial insert (Maxx Freedom TKA System®). The trial prosthesis is inserted and kinematics tested, including patellofemoral joint tracking. The definitive prosthesis is inserted, and routine closure commenced. All patients in both cohorts had no instances of lateral retinaculum release and use of constrained poly.
Clinical outcomes measurements
The PROMs that is, WOMAC score [11] and OKS [12], were collected for all patients pre- and post-operatively at 3 months and 6 months. The WOMAC score is a standardized questionnaire used to evaluate pain, stiffness, and physical function in patients with knee osteoarthritis. Higher scores indicate worse symptoms and greater disability.
The OKS is a 12-item patient-reported questionnaire used to assess pain and functional outcomes after knee surgery, especially knee replacement. Scores range from 0 to 48, with higher scores indicating better knee function and less pain.
Other measures studied were complications and improvement in flexion/change in ROM at 3 months post-operatively.
Radiological outcomes measurements
Post-operative check, X-ray, and Alignment X-ray were obtained at 3-month follow-up. The HKA, deformity correction, LDFA, and MPTA were calculated. The post-operative knee phenotype and JLO were derived.
Data analyses
Statistical analysis was made using the Statistical Package for the Social Sciences (Version 16). Statistical methods included the unpaired t-test, repeated measures analysis of variance, correlation analysis, and the area under the curve.
Demographics
The variables, such as age, sex, body mass index, type of surgical anesthesia, and pre-operative degree of valgus deformity, did not vary significantly between CM-TKA and RA-TKA cohorts. Demographic details are mentioned in Table 1.
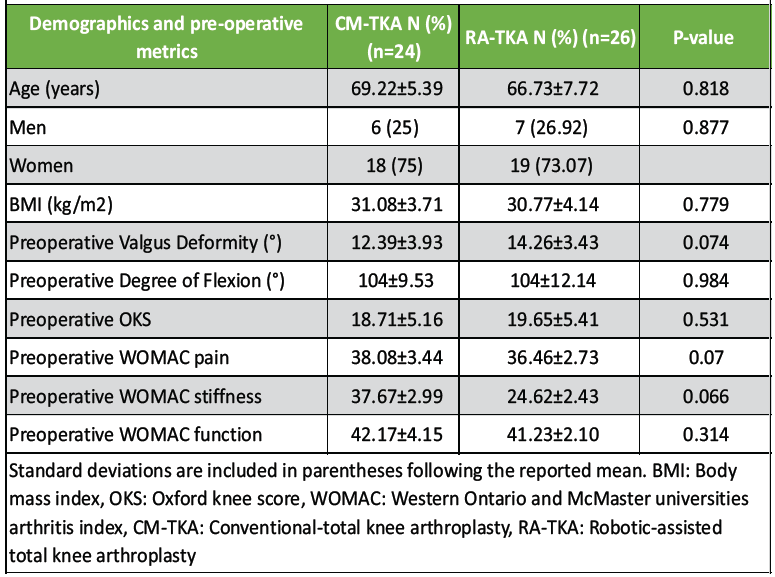
Table 1: Comparison of demographic and pre-operative metrics between CM-TKA and RA-TKA cohorts
Deformity, ROM, soft tissue release
Among the total 50 patients, 30 (60%) were classified as Ranawat Grade 1. The remaining 20 patients (40%) were categorized as Ranawat Grade 2. The difference between the groups was not statistically significant. The distribution of valgus grades in both cohorts is given in Table 2.
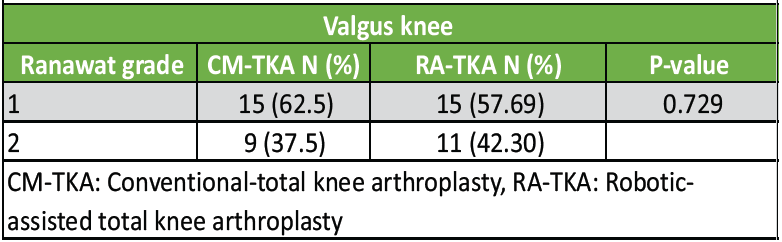
Table 2: Distribution of grade of valgus deformity in CM-TKA and RA-TKA cohorts
The average radiological correction of deformity was assessed at 3-month follow-up. It was 12.22 (±3.91) in the CM-TKA and 11.65 (±3.49) in the RA-TKA cohort, with no statistical difference (P = 0.587). There was no statistical difference in the pre-operative degree of flexion in both cohorts (P = 0.984). The mean pre-operative flexion was comparable in both the cohorts; 104 (±9.53) in the CM-TKA cohort and 104 (±12.14) in the RA-TKA cohort (Table 1). However, the ROM improved at 3 months in both cohorts, 111.25 (±13.29) in the CM-TKA and 116.96 (±9.31) in the RA-TKA cohort. The improvement (change in flexion) was significant in the RA-TKA cohort (P = 0.021) (Table 3).
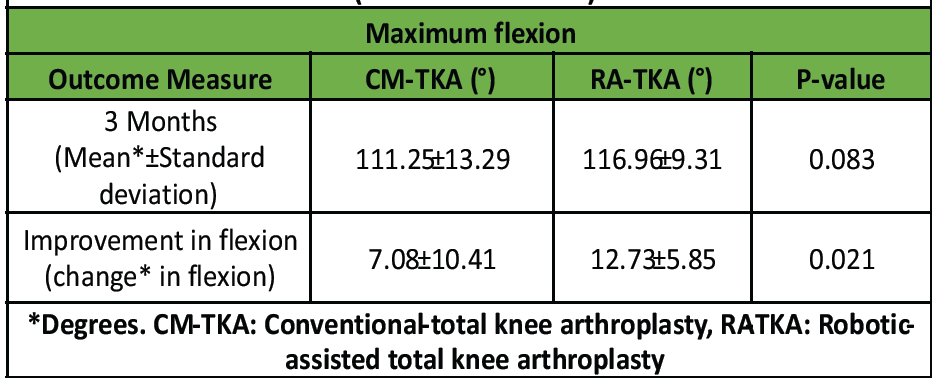
Table 3: Pre-operative and post-operative range of motion (maximum flexion)
The soft tissue intervention was done according to the Ranawat technique in both cohorts. It was observed that the soft tissue intervention was extensively required in the CM-TKA group, whereas the RA-TKA cohort required less release with significance (P = 0.0104) (Table 4). The mean duration of surgery was almost similar in both cohorts.
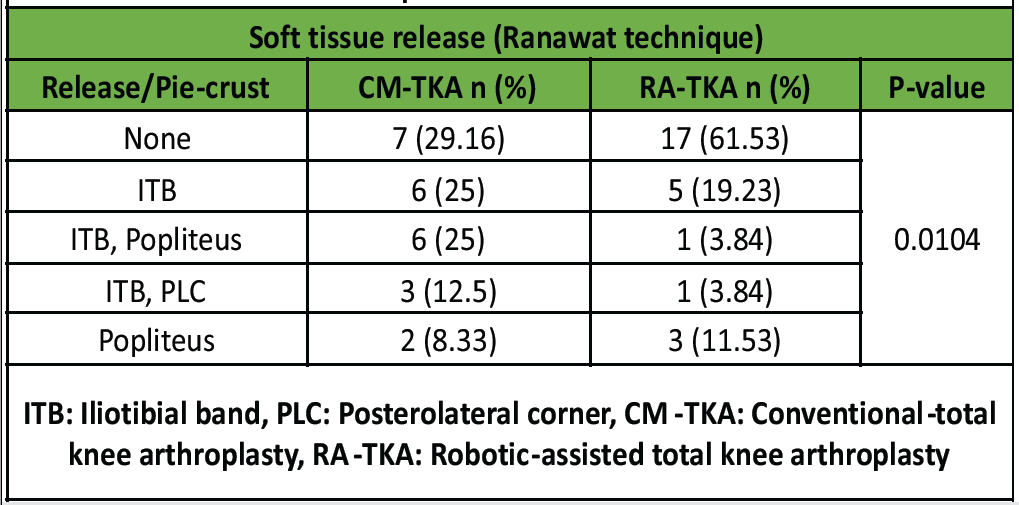
Table 4: Intra-operative soft tissue intervention
PROMs
At the 3-month follow-up, both groups showed significant improvement in OKS. Statistical analysis revealed a high significant difference in OKS score between the two groups (P = 0.006), suggesting that robotic-assisted Total knee replacement (TKR) led to better functional recovery compared to the CM technique. The consistently higher OKS in the robotic group at both 3 and 6 months indicates that patients undergoing robotic-assisted TKR experienced greater improvements in knee function and overall quality of life post-operatively (Table 5).
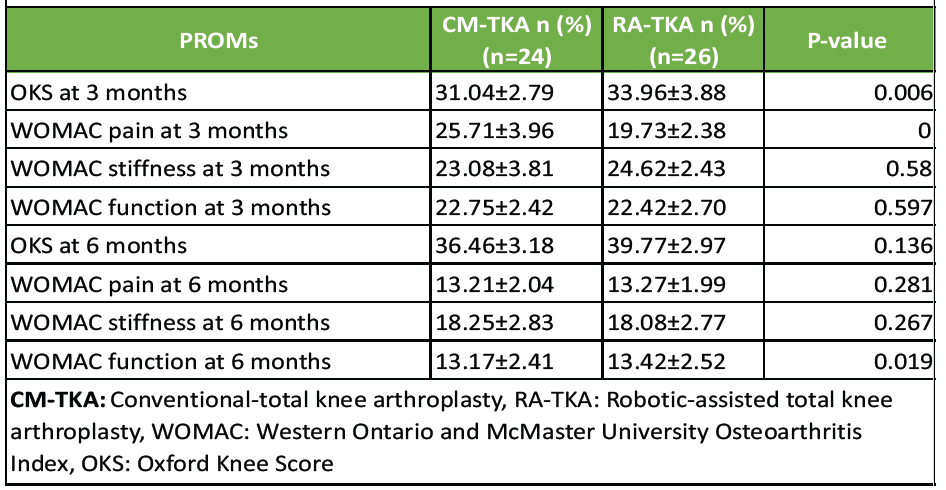
Table 5: Patient reported outcome measures at 3 months and 6 months follow-up
The RA-TKA group revealed a high statistical significance (P = 0.000) at 3 months of follow-up, the CM-TKA cohort had an average WOMAC Pain score of 25.71 ± 3.96, compared to a 19.73 ± 2.38 in the RA-TKA cohort (Table 5). However, this trend does not persist at 6 months of follow-up (P = 0.281). There was no difference in rate of improvement in post-operative WOMAC Stiffness scores at 3 months (P = 0.580) or 6-month follow-up (P = 0.267) between CM-TKA and RA-TKA groups. CM-TKA cohort had WOMAC Function score of 22.75 ± 2.42 as compared to 22.42 ± 2.70 in RA-TKA cohort at 3-month follow-up; this difference was not statistically significant (P = 0.597). WOMAC Function score at 6-month follow-up, RA-TKA group revealed a statistically significant higher improvement 13.42 ± 2.52 as compared to 13.17 ± 2.41 (P = 0.019) (Fig. 2).
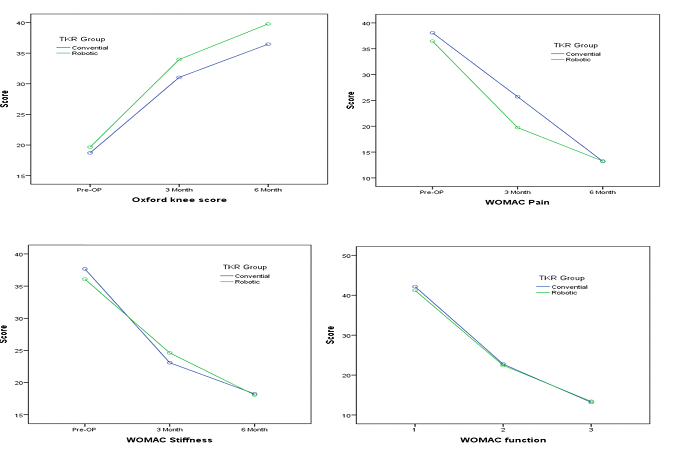
Figure 2: Trend of Oxford knee score and Western Ontario and McMaster universities osteoarthritis index scores over 3 and 6 months follow-up.
Pre and post-operative phenotypes in CM-TKA and RA-TKA cohorts are shown in Table 6.
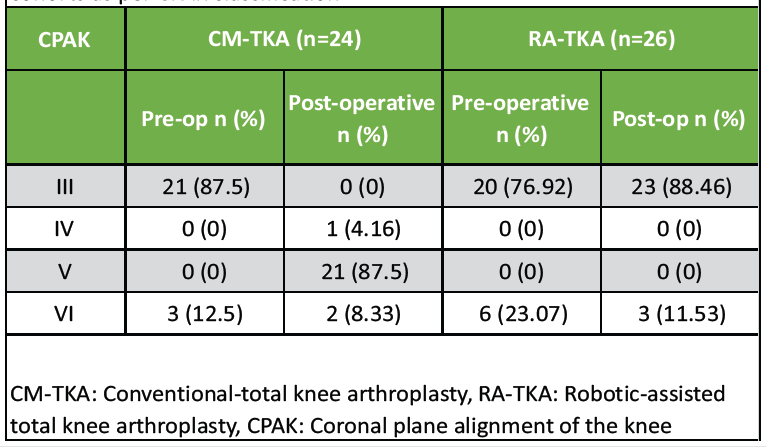
Table 6: Pre-operative and post-operative knee phenotypes in both cohorts as per CPAK classification
There was no significant difference in pre-operative CPAK classification between CM-TKA and RA-TKA. In CM-TKA, most cases had an altered phenotype, with only 8.33% inheriting the pre-operative phenotype. On the other hand, 88.46% cases inherited pre-operative phenotype in the RA-TKA cohort. Analysis of the change in proportion between pre-operative and post-operative phenotypes (McNemar test) is given in Table 7. The proportion of change in CPAK was very high in the CM-TKA cohort (P = 0.783) than RA-TKA cohort (P = 0.250).
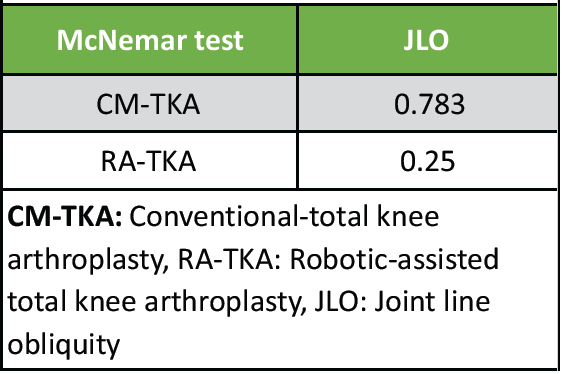
Table 7: Analysis of the change in proportion between pre-operative and post-operative phenotypes
Complications
The majority of patients had no wound complications, two cases of delayed healing at the pin track were observed exclusively in the robotic group. This may be attributed to the additional instrumentation required for robotic-assisted surgery. The RA-TKA cohort had one case with increased lateral patellar tilt angle in the skyline view after consideration of internal rotation. However, the patient did not complaint of anterior knee pain or patellar subluxation.
Valgus knees involve surgical challenges to achieve alignment and soft tissue balancing throughout the ROM – flexion, extension, and mid-flexion [10,13]. RA-TKA has developed a new era of real-time balancing, precise component positioning, and yields an advantage in such challenging valgus knees. The inherent accuracy of the CT-based robotic system aids to achieve optimum gap balance. The pre-operative planning (J planner in CT-based CUVIS system in our cohort) delivers an important aspect to plan the placement of femoral and tibial components. Intra-operative adjustments were made for gap balancing, which incorporated the principles of FA. Gap-balancing in the CUVIS robotic system requires anticipation of opening in the compartment after the planned bony cuts. During intra-operative gap balancing, if the opening in the medial or lateral compartment is more than 1 mm on giving a valgus or varus stretch, then chances of an increased gap are more after the bony cuts. After giving a neutral or varus stretch in a valgus knee, if the knee reverts back into valgus spontaneously, then it denotes that the lateral structures are tight; hence, additional release after the bony cuts can be commenced. However, the amount of release required for gap balancing throughout the ROM was comparatively less in RA-TKA cohort with the FA setup. When considering the optimal alignment, the relationship between the prosthesis and the soft tissue envelope may be more important than neutral mechanical alignment [14]. The CPAK classification makes us to calculate the pre-operative MPTA. One can also judge the extra-articular tibia-valga morphology during pre-operative planning, as it is commonly associated with valgus knee deformity. The authors believed that, while we aim to regain the same CPAK phenotype of the knee, MPTA is the most important factor to consider specifically in tibia-valga morphology. The tibia cut was kept in valgus in cases of extra-articular tibia-valga and otherwise neutral or varus in the absence of tibia-valga, which counters medial compartment laxity. Important factor to note- in cases of extra-articular tibia-valga, if the tibia cut is kept in neutral or even varus, this might necessitate increased internal rotation of the femoral component, which may balance the mediolateral gaps but leads to patellar instability. The overall alignment was kept within the “safe zone” up to 3° of valgus in the RA-TKA cohort. Excessive valgus not more than 3° was to avoid erratic component positioning and recurrence of valgus deformity. FA is based on a blend of inherent bony anatomy and an evaluation of soft-tissue laxity [10,15,16,17]. In the RA-TKA cohort, overall limb alignment was targeted within neutral to 3° valgus in the coronal plane based on the arithmetic HKA or pre-operative knee phenotype according to CPAK classification. Multiple studies have been conducted based on FA philosophy using a CT-based robotic platform in the varus knee [15,16]. However, these studies lack application of FA in patients with valgus deformity. Oussedik et al., studied the FA suggested overall limb alignment to be kept within the 0° ± 3° “safe zone” of coronal alignment, and also highlighted on possibility of change in the zones with further research [10]. In the study done by Clark et al, overall limb alignment of between 3° valgus and 6° varus was kept as the safe zone [17]. The role of femoral component rotation plays an important role in case of valgus knee with lateral compartment bony deficiencies and estimation of epicondylar axis is critical. Even in experienced hands, clinical estimation of the epicondylar axis is inaccurate and should not be relied upon as the sole determinant of femoral rotation [18]. Wherein the CT-based CUVIS system is able to estimate the exact surgical epicondylar axis using J planner. As we followed FA in the RA-TKA cohort, the femoral component was rotated internally (to surgical epicondylar axis) up to 2° in 6 cases after a tibial component valgus of up to 2° to achieve equal mediolateral gaps in flexion and extension. The optimum soft tissue tension was achieved in all compartments with good patellar tracking. All 6 patients underwent an additional skyline view X-ray and CT scan at 3-month follow-up to evaluate patella tilt (Fig. 3). However, among those, a single patient revealed increased lateral tilt on skyline view X-ray at 3-month follow-up (Fig. 4).
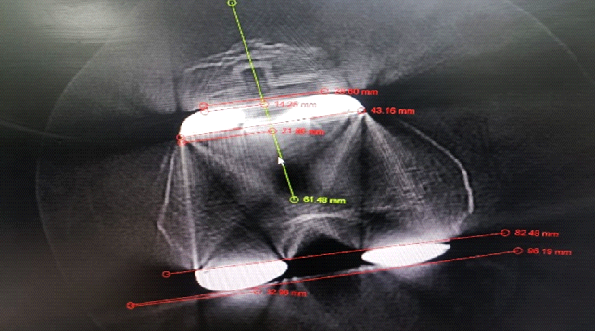
Figure 3: Post-operative computed tomography knee of a patient who received internal rotation in femoral component internally to 2° with reference to surgical epicondylar axis and equivalent valgus rotation of the tibia component.

Figure 4: Excessive lateral tilt in the patella is probably secondary to increased internal rotation of the femoral component.
The 0–3° of internal rotation can be optimum according to FA principles [10,15,16,17]. However, we noticed that this rotation (internal rotation in our case) can be considered as “optimum” only up to the amount of degree where posteromedial and posterolateral condylar resections are equal. As the posterolateral condyle resection exceeds the posteromedial condyle resection, it can lead to patella subluxation. The neutral tibia cut in tibia-valga leads to medial compartment laxity. To balance it in flexion, we end up considering more internal rotation of the femoral component, which leads to patella subluxation. Thus, the authors suggest that the consideration of the surgical epicondylar axis and MPTA is most important while dealing with the FA. In our study, we observed significant improvement in OKS at 3 and 6 months follow-ups. There was a substantial reduction in WOMAC pain score at 3 months; however, this effect was comparable at 6-month follow-up. The short-term improvement in RA-TKA is reported in the literature and our findings are consistent with their studies. In a meta-analysis, Zhang et al., found that the RA-TKA results in improved WOMAC scores than CM-TKA at short to midterm follow-up (average of 8.6 months), with a mean difference of 3.72 (P = 0.009); however, the authors did not report average pre-operative alignment and pre-arthritic knee phenotype. Furthermore, the discussion about confounding variables due to the use of multiple robotic systems is lacking [19]. Gorur et al., concluded that the RA-TKA cohort showed faster improvement in PROMs in comparison with CM TKA (37.16 ± 18.8 versus 25.74 ±17.7, P¼ 0.02) [20]. However, the study did not specify the technique and frequency of soft tissue releases in the RA-TKA cohort.
Limitations
Our study is based on a retrospective review of data that was collected prospectively, with patients, themselves choosing either robotic or CM TKA, introducing selection bias, but all surgeries were performed by a single surgeon at a single institution using the same implant manufacturer. Therefore, there is a potential for biases stemming from the surgeon’s expertise, the selection of patients, and specific institutional practices. These factors may limit the generalizability of the findings to other healthcare environments, surgeons, or patient groups. This study has a short duration of follow-up of six months. The long-term follow-ups are required to understand the trend in PROMs and revision rate in RA-TKA setups. The study’s sample size is small and larger multicentric randomized control trials with this technique are required to establish and solidify the findings of this study.
The gap balancing and accurate component positioning using CUVIS (CT-based) robotic system leads to optimum gap balancing throughout the ROM, less soft tissue release, less post-operative pain, and improved function. The RA-TKA with FA shows an early patient recovery with improved ROM as compared to CM-TKA in valgus deformity. The RA-TKA inherited pre-operative knee phenotype according to the CPAK classification with optimal patellar tracking. The pre-operative planning should involve evaluation of MPTA and surgical epicondylar axis, which stand as the most important factor while dealing with the FA for valgus knees. Perhaps the long-term analysis is required to study and solidify the outcomes in RA-TKA.
Robotic-assisted TKA with functional alignment using the CUVIS system offers superior early outcomes in valgus knees by achieving optimal gap balancing, reduced soft tissue releases, and better preservation of the native knee phenotype. Accurate pre-operative planning focusing on MPTA and the surgical epicondylar axis is essential for optimal alignment and patellar tracking.
References
- 1. Cho Y, Lee MC. Rotational alignment in total knee arthroplasty. Asia Pac J Sports Med Arthrosc Rehabil Technol 2014;1:113-8. [Google Scholar] [PubMed]
- 2. Stucinskas J, Robertsson O, Sirka A, Lebedev A, Wingstrand H, Tarasevicius S. Moderate varus/valgus malalignment after total knee arthroplasty has little effect on knee function or muscle strength. Acta Orthop 2015;86:728-33. [Google Scholar] [PubMed]
- 3. Triangga AF, Magetsari RM, Purnomo G, Rahmansyah N, Riyadli M, Sibarani T. A case series of total knee arthroplasty with a non-constrained implant in 2nd and 3rd degree valgus deformity in knee osteoarthritis and medial collateral ligament insufficiency. Int J Surg Case Rep 2023;106:108162. [Google Scholar] [PubMed]
- 4. Mazzotti A, Perna F, Golinelli D, Quattrini I, Stea S, Bordini B, et al. Preoperative valgus deformity has twice the risk of failure as compared to varus deformity after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019;27:3041-7. [Google Scholar] [PubMed]
- 5. Adamska O, Modzelewski K, Szymczak J, Świderek J, Maciąg B, Czuchaj P, et al. Robotic-assisted total knee arthroplasty utilizing NAVIO, CORI imageless systems and manual TKA accurately restore femoral rotational alignment and yield satisfactory clinical outcomes: A randomized controlled trial. Medicina (Kaunas) 2023;59:236. [Google Scholar] [PubMed]
- 6. Bae DK, Song SJ, Park CH, Ko YW, Lee H. A comparison of the medium-term results of total knee arthroplasty using computer-assisted and conventional techniques to treat patients with extraarticular femoral deformities. J Arthroplasty 2017;32:71-8. [Google Scholar] [PubMed]
- 7. Huang TW, Chuang PY, Lee CY, Lin SJ, Huang KC, Shen SH, et al. Total knee arthroplasty in patients with Ranawat type-II valgus arthritic knee with a marked coronal femoral bowing deformity: Comparison between computer-assisted surgery and intra-articular resection. J Orthop Surg Res 2016;11:88. [Google Scholar] [PubMed]
- 8. Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 2005;87 Suppl 1:271-84. [Google Scholar] [PubMed]
- 9. MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB. Coronal plane alignment of the knee (CPAK) classification. Bone Joint J 2021;103-B:329-37. [Google Scholar] [PubMed]
- 10. Oussedik S, Abdel MP, Victor J, Pagnano MW, Haddad FS. Alignment in total knee arthroplasty. Bone Joint J 2020;102-B:276-9. [Google Scholar] [PubMed]
- 11. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833-40. [Google Scholar] [PubMed]
- 12. Oxford University Innovation. The Oxford Knee Score (OKS); 2016. Available from: https://innovation.ox.ac.uk/outcome-measures/oxford-knee-score-oks (Last Accessed on May 30th, 2025) [Google Scholar] [PubMed]
- 13. Lange J, Haas SB. Correcting severe valgus deformity: Taking out the knock. Bone Joint J 2017;99-B(1 Suppl A):60-4. [Google Scholar] [PubMed]
- 14. Aflatooni JO, Wininger AE, Park KJ, Incavo SJ. Alignment options and robotics in total knee arthroplasty. Front Surg 2023;10:1106608. [Google Scholar] [PubMed]
- 15. Shatrov J, Battelier C, Sappey-Marinier E, Gunst S, Servien E, Lustig S. Functional Alignment Philosophy in Total Knee Arthroplasty – Rationale and technique for the varus morphotype using a CT based robotic platform and individualized planning. SICOT J 2022;8:11. Erratum in: SICOT J 2022;8:18. [Google Scholar] [PubMed]
- 16. Rajashekhar KT, Bhat AK, Biradar N, Patil AR, Mangsuli K, Patil A. Gap balancing technique with functional alignment in total knee arthroplasty using the cuvis joint robotic system: Surgical technique and functional outcome. Cureus 2025;17:e78914. [Google Scholar] [PubMed]
- 17. Clark GW, Steer RA, Khan RN, Collopy DM, Wood D. Maintaining joint line obliquity optimizes outcomes of functional alignment in total knee arthroplasty in patients with constitutionally varus knees. J Arthroplasty 2023;38(7 Suppl 2):S239-44. [Google Scholar] [PubMed]
- 18. Kinzel V, Ledger M, Shakespeare D. Can the epicondylar axis be defined accurately in total knee arthroplasty? Knee 2005;12:293-6. [Google Scholar] [PubMed]
- 19. Zhang J, Ndou WS, Nathan NG, Gaston P, Simpson PM, Macpherson GJ, et al. Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2022;30:2677-95. [Google Scholar] [PubMed]
- 20. Gorur A, Czerwonka N, El-Othmani MM, Held MB, Neuwirth AL, Geller JA. Outcomes of image-free robotic assisted total knee arthroplasty in patients who have valgus knee deformities. J Arthroplasty 2024;39(9S2):S235-40. [Google Scholar] [PubMed]