Arthroscopic microfracture remains an effective first-line surgical option for small, well-contained osteochondral lesions of the talus (OLT). Prognostic factors such as lesion size, containment, and strict adherence to postoperative rehabilitation significantly influence outcomes. MRI-based evaluation (MOCART score) can provide objective evidence of repair quality and correlates well with functional recovery. Biologic augmentation strategies may enhance the durability of repair tissue and represent the future direction of OLT management.
Dr. Lionel John, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: johnlioneljohn@gmail.com
Introduction: Osteochondral lesions of the talus (OLTs) are focal injuries of the articular cartilage and subchondral bone, most often secondary to ankle trauma. Arthroscopic microfracture has become the most widely used to evaluate the effectiveness of arthroscopic microfracture as a treatment for small, well-contained OLTs by stimulating marrow-derived repair tissue formation and assessing clinical as well as radiological outcomes.
Materials and Methods: Study Report: In our series, patients with symptomatic OLTs underwent arthroscopic microfracture and were evaluated clinically and radiologically. Functional outcomes were measured using the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, while postoperative repair in selected patients was assessed with magnetic resonance imaging (MRI) using the magnetic resonance observation of cartilage repair tissue scoring system. Postoperative rehabilitation included strict non-weight-bearing for the first 6 weeks, followed by gradual return to activity. Postoperatively, patients demonstrated significant improvement in AOFAS scores, reflecting enhanced pain relief, function, and alignment. MRI-based evaluation revealed satisfactory cartilage fill and surface congruity in most cases, correlating with clinical recovery. Better outcomes were observed in patients with smaller (<15 mm), contained lesions and those who adhered to the rehabilitation protocol. In contrast, larger or cystic lesions and poor compliance were associated with delayed recovery or persistent symptoms.
Conclusion: Arthroscopic microfracture is a safe, minimally invasive, and effective joint-preserving treatment for small OLTs, especially in young, active individuals. Careful patient selection, early intervention, and compliance with rehabilitation are critical to optimizing outcomes. Biologic augmentation may further enhance long-term durability of cartilage repair.
Keywords: Osteochondral lesion, talus, arthroscopy, microfracture, ankle cartilage repair, magnetic resonance observation of cartilage repair tissue, American Orthopaedic Foot and Ankle Society
Osteochondral defects (OCDs) of the talus are focal injuries that involve both the articular cartilage and the underlying subchondral bone. They are most frequently associated with traumatic events such as ankle sprains or fractures, although non-traumatic etiologies including ischemia and repetitive microtrauma have also been described [1,2]. Clinically, these lesions often present with persistent ankle pain, swelling, stiffness, and mechanical symptoms such as catching or locking, which can significantly impair daily function and quality of life if left untreated [2,3]. Several treatment strategies have been described, ranging from non-operative care to advanced cartilage restoration procedures. Among the surgical options, arthroscopic microfracture has become the most widely adopted first-line technique, especially for small and well-contained lesions. The principle of microfracture is to perforate the exposed subchondral bone with multiple small holes, allowing mesenchymal stem cells and marrow elements to migrate into the defect. This results in the formation of a fibrin clot that eventually matures into fibrocartilage [1,3,4]. Although fibrocartilage lacks the mechanical strength and durability of native hyaline cartilage, clinical studies have shown that it can restore joint congruence and provide significant pain relief and functional improvement in the short to mid-term [2,3,5]. Microfracture is generally recommended for lesions smaller than 15 mm in diameter and those without advanced subchondral cysts or degenerative arthritis [3,4]. For larger, uncontained, or cystic lesions, alternative procedures such as osteochondral grafting, autologous chondrocyte implantation, or scaffold-based techniques may be more appropriate [4]. Despite these limitations, microfracture remains a valuable procedure because it is minimally invasive, technically straightforward, and cost-effective [2,4,5]. However, long-term studies have raised concerns regarding the durability of fibrocartilage repair tissue, which may deteriorate over time and compromise functional outcomes [2,6]. To address this, recent research has focused on biologic augmentation methods such as platelet-rich plasma (PRP), bone marrow aspirate concentrate (BMAC), and collagen or hyaluronic acid-based scaffolds. These adjuncts have shown promising results in improving cartilage repair quality and long-term clinical outcomes [7,8,9,10].
Aims and objectives
Aim of the study
The aim of the study is to evaluate the functional outcomes of arthroscopic microfracture treatment for OCDs of the talus in patients at tertiary care hospital.
Objectives of the study
The objective of the study is to assess the functional outcomes of arthroscopic microfracture for talus OCDs using the American Orthopaedic Foot and Ankle Society (AOFAS) and magnetic resonance observation of cartilage repair tissue (MOCART) scoring systems to evaluate radiological findings through magnetic resonance imaging (MRI).
Study design
This is a prospective cohort study that will monitor outcomes longitudinally in patient who will be treated with arthroscopic microfracture surgery for talus OCDs.
Study duration
Data collection and follow-up of 18 months by undertaking baseline evaluation, intraoperative information, and follow-up of 1 year to 18 months at appropriate time intervals with functional and radiological assessment for monitoring of the progress.
Sample size calculation
The sample size calculation for the estimation of mean for 15 patients where computed the minimal detectable mean difference d for n = 15, α = 0.05, power = 0.8, using a few plausible SDs of the differences (typical scores like AOFAS often falls in ~8–15 points depending on population; pick from literature if possible); if σ (SD of differences) = 8, minimal detectable mean change with n = 15 ≈ 5.8 points; if σ = 10, minimal detectable mean change ≈ 7.2 point; if σ = 12, minimal detectable mean change ≈ 8 points; if σ = 15, minimal detectable mean change ≈ 10.9 points.
(Computation used Z values 1.96 and 0.842)
Inclusion criteria
- Age above 18 years
- Patients of either sex
- Patients having osteochondral lesion of the talus (stage 2 and stage 3) of Berndt and Harty classification
- Patients who are fit for surgery.
Exclusion criteria
- Age below 18 years
- Patients unfit for surgery and/or anesthesia
- Ipsilateral and contralateral to any lower limb fracture associated with study is not considered.
Functional outcome measurement tool
For functional outcome variables such as pain, function, and ankle alignment, the AOFAS scoring system will be utilized. The higher the score, the better the functionality with minimal pain. Standard MRI will be performed to analyze characteristics before as well as after surgery, and radiological data will be noted down for comparison with functional MOCART scores.
Surgical procedure
Arthroscopic microfracture technique
The anterior or posterior two-portal approach is selected based on the location of the osteochondral lesion of the talus (OLT). Patients undergoing the anterior approach were positioned supine position. An anteromedial and anterolateral two-portal approach was made (Fig. 1 and 2). Just medial to the tibialis anterior tendon helps define the anteromedial portal and the anterolateral portal just laterals to the peroneus tertius tendon. Arthroscopic microfracture is a reparative cartilage procedure performed under direct visualization to address OLTs (Fig. 3). For reference, Figure 4 shows osteochondral lesion over the talus.

Figure 1: Anteromedial portal.
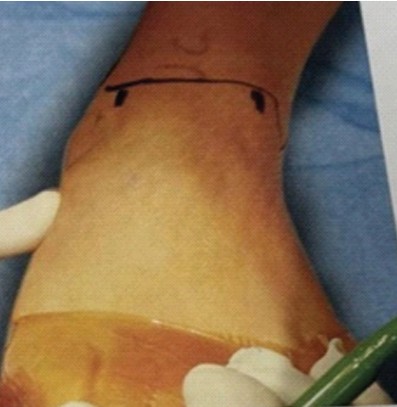
Figure 2: Anterolateral portal.

Figure 3: Arthroscopic view of microfracture.
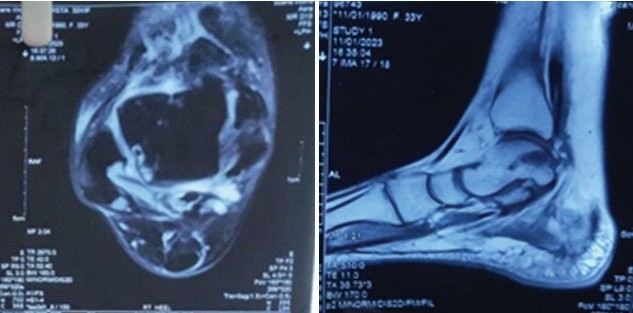
Figure 4: The above images show osteochondral lesion over the talus.
After diagnostic arthroscopy, identifying the OCD a shaver or curette was used to remove the unstable cartilage and subchondral necrotic bone. The sclerotic zone was completely debrided; the lesion is thoroughly debrided to remove unstable cartilage, exposing a stable rim of healthy cartilage and a clean subchondral base.
After diagnostic arthroscopy, identifying the OCD a shaver or curette was used to remove the unstable cartilage and subchondral necrotic bone (Fig. 5).
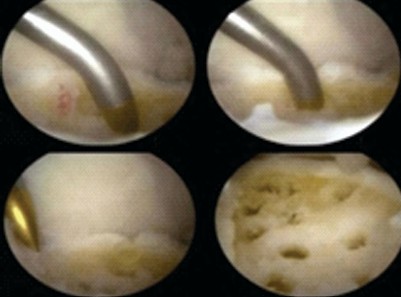
Figure 5: Intraoperative arthroscopic images.
The sclerotic zone was completely debrided; the lesion is thoroughly debrided to remove unstable cartilage, exposing a stable rim of healthy cartilage and a clean subchondral base. A microfracture awl or 1.4-mm Kirschner wire or a 2-mm drill through the portal was used to drill several holes in the base of the OCD of talus used to create multiple evenly spaced perforations (approximately 3–4 mm apart) into the subchondral bone, penetrating 2–4 mm deep. This induces bleeding from the underlying marrow cavity, forming a fibrin clot rich in mesenchymal stem cells and growth factors. The resulting clot provides a biodegradable scaffold that (a) fills the OCD, (b) supports mesenchymal cell infiltration and chondrogenic differentiation, (c) has appropriate porosity/mechanics, and (d) degrades at a rate matching matrix deposition.
Post-operative rehabilitation
0–6 weeks: Non-weight bearing – Ankle range of motion exercises. Pain management with nonsteroidal anti-inflammatory drugs
6–12 weeks: Gradual partial weight-bearing – Begin strengthening exercises. Avoid impact/loading activities
3–6 months: Full weight-bearing as tolerated
6–12 months: Return to sport-specific training gradually – Avoid high-impact sports until
9–12 months: Clinical evaluation+functional scoring (AOFAS) – Reassess with MRI (MOCART score) if symptoms persist.
OLTs remain a significant challenge in orthopedic practice, as they frequently lead to persistent ankle pain and functional limitation after trauma. Arthroscopic microfracture has gained widespread acceptance as an initial surgical option because it is minimally invasive, cost-effective and can be performed reproducibly with relatively low morbidity. The biological rationale of the technique lies in disrupting the subchondral bone to release marrow elements rich in mesenchymal stem cells and growth factors, which form a fibrin clot that matures into repair tissue [3,4,5]. In our series, we found a clear improvement in functional outcomes as measured by the AOFAS score, with postoperative values indicating significant pain relief, better joint function, and improved alignment. This trend mirrors previous reports. Lee et al. (2009) highlighted that lesions <15 mm in diameter and contained within intact cartilage margins show particularly favorable results after microfracture [3]. Chuckpaiwong et al. (2008) also emphasized lesion size and early intervention as the most important predictors of long-term outcome [1]. Imaging findings further reinforced these results. In patients who underwent postoperative MRI, MOCART scores demonstrated satisfactory cartilage fill and surface congruity. This supports the concept that structural repair is closely related to clinical improvement. Yang et al. (2020) confirmed a significant correlation between MOCART score and functional outcomes, suggesting that MRI remains a valuable tool for objective evaluation of repair quality [8]. Compliance with the postoperative rehabilitation protocol was another important determinant of success. Patients who adhered to the recommended 6 weeks of non-weight-bearing generally had superior recovery, whereas poor compliance led to delayed improvement or persistent symptoms. While short- and mid-term results of microfracture are generally satisfactory, concerns remain regarding long-term durability. Fibrocartilage lacks the biomechanical resilience and durability of native hyaline cartilage, and several studies, including those by Ferkel et al. (2008) and Ross et al. (2019), have shown a gradual decline in functional scores with longer follow-up [2,6]. Larger or cystic lesions, in particular, are less likely to achieve durable benefit with microfracture alone. Emerging biologic strategies have shown promise in addressing these limitations. Adjunctive treatments such as PRP, BMAC, and collagen or hyaluronic acid scaffolds have been investigated as means of improving the quality of repair tissue. Randomized controlled trials, such as those by Lee et al. (2022) and Yoon et al. (2020), have reported superior outcomes when microfracture was combined with biologic augmentation compared to microfracture alone [7,9]. These findings suggest that future management of OLTs may increasingly rely on combining traditional techniques with biologic enhancers to optimize both structural and clinical outcomes. Despite these advances, arthroscopic microfracture continues to serve as an effective, accessible, and relatively low-cost first-line surgical option. For young, active patients with small, contained OLTs, it provides reliable pain relief and functional restoration. In contrast, larger or recurrent lesions may benefit from advanced restorative or replacement procedures, though these come with higher costs and technical demands.
Arthroscopic microfracture is an effective and safe treatment for OCDs of the talus. The procedure showed significant functional improvements as evidenced by the progression of AOFAS scores, with 12 patients resulting in good to excellent outcomes and 3 patients had moderate outcome at 1 year, supported by MRI, with complete cartilage regeneration. Post-operative complications were minimal and manageable, further confirming the safety of this approach. In conclusion, arthroscopic microfracture is an option that offers significant improvement in function and quality of life in the management of OLT. The study contributes value to understanding the effectiveness of the procedure and, therefore, should be seen in the light of further research for optimizing patient selection, surgical techniques, and post-operative care.
Arthroscopic microfracture is a safe, minimally invasive, and cost-effective first-line treatment for small, contained OCDs of the talus. It provides significant short- to mid-term pain relief and functional improvement, particularly in carefully selected patients. Lesion size, containment, and strict adherence to postoperative rehabilitation are key predictors of successful outcomes. Larger or cystic lesions may require alternative or biologically augmented procedures for durable long-term results.
References
- 1. Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: Outcome analysis and outcome predictors of 105 cases. Am J Sports Med 2008;36:286-92. [Google Scholar] [PubMed]
- 2. Ferkel RD, Zanotti RM, Komenda GA, Sgaglione NA, Cheng MS, Applegate GR, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: Long-term results. Am J Sports Med 2008;36:1750-62. [Google Scholar] [PubMed]
- 3. Lee KB, Bai LB, Park JG, Yoon TR. A prospective study of osteochondral lesions of the talus treated with microfracture: Prognostic significance of lesion size and containment. Am J Sports Med 2009;37(Suppl 1):83S-8. [Google Scholar] [PubMed]
- 4. Van Bergen CJ, De Leeuw PA, Van Dijk CN. Arthroscopic surgery in ankle osteochondral defects: An evidence-based approach. Instr Course Lect 2013;62:143-53. [Google Scholar] [PubMed]
- 5. Gök K, Aydin AT, Tuncay I. Evaluation of arthroscopic treatment of osteochondral lesions of the talus using MRI and clinical assessment. Acta Orthop Belg 2017;83:610-7. [Google Scholar] [PubMed]
- 6. Ross KA, Hannon CP, Deyer TW, Smyth NA, Hogan MV, Do HT, Kennedy JG. Radiographic and clinical evaluation of osteochondral lesions of the talus following microfracture. Foot & Ankle International. 2019;40(8):903–911. [Google Scholar] [PubMed]
- 7. Yoon HS, Lee M, Kang J, Lee KB. Midterm outcomes of microfracture with and without platelet-rich plasma. Foot Ankle Int 2020;41:385-92. [Google Scholar] [PubMed]
- 8. Yang HY, Park KB, Kim HW, Kim SH. Association of MRI-based MOCART score and clinical outcome in patients with osteochondral lesions of the talus treated with microfracture. Knee Surg Sports Traumatol Arthrosc 2020;28:220-6. [Google Scholar] [PubMed]
- 9. Lee DH, Lee KB, Jung ST, et al[1.1]. Randomized controlled trial of bone marrow aspirate concentrate with collagen scaffold in osteochondral lesions of the talus. Orthop J Sports Med 2022;10:23259671221084332[2.1]. [Google Scholar] [PubMed]
- 10. Zhang Y, Wang F, Chen Y, et al[3.1]. Comparison of arthroscopic microfracture with and without debridement for osteochondral lesions of the talus. J Orthop Surg Res 2023;18:56. [Google Scholar] [PubMed]