MIPPO with anatomical distal tibial plates provides reliable fracture union, excellent functional outcomes, and minimal complications, making it a safe and effective treatment for distal tibial fractures.
Dr. H Rohit Karthik, Department of Orthopaedics, Sree Balaji Medical College and Hospital, CLC works road, Shankar Nagar, Chromepet, Chennai - 600044, Tamil Nadu, India. E-mail: rohotron@gmail.com
Introduction: Distal tibial fractures are difficult to manage due to their complex anatomy, subcutaneous location, and poor vascularity. Conventional open plating often causes soft tissue complications, while intramedullary nailing and external fixation have limitations in alignment and infection control. Minimally invasive percutaneous plate osteosynthesis (MIPPO) with anatomical distal tibial plates preserves periosteal blood supply and provides stable fixation. This study aimed to evaluate clinical and functional outcomes of distal tibial fractures treated by MIPPO.
Materials and Methods: A prospective case series was conducted at a tertiary care center from January 2022 to June 2024. Thirty-six patients were treated using MIPPO; 23 with a minimum of 12 months’ follow-up were included. AO type 43-A2, 43-A3, and 43-C3 fractures and Gustilo-Anderson Grade I open fractures were included. Functional recovery was assessed using the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot score and the Foot and Ankle Ability Measure. Radiological union time and complications were also analyzed.
Results: The mean patient age was 47.5 years; 65% of injuries were from road traffic accidents. The mean radiological union time was 11.4 weeks (range 5–17). Mean AOFAS scores improved from 39.6 preoperatively to 82.9 at 6 months and 87.7 at 12 months (P < 0.0001), with 90% achieving good-to-excellent outcomes. Complications included delayed union in three cases (13%), one superficial infection (4.3%), and one mild varus malunion (4.3%), all resolving without reoperation. There were no deep infections, implant failures, or non-unions.
Discussion: MIPPO with anatomical locking plates provided excellent union rates and functional recovery, with minimal wound complications. Results compare favorably with previous series (union 11–16 weeks) and confirm that limited soft tissue dissection preserves vascularity and enhances healing. While small sample size and single-center design limit generalizability, outcomes reinforce MIPPO as a reliable fixation strategy for distal tibial fractures.
Conclusion: MIPPO using anatomical distal tibial plates is a safe, effective, and biologically sound fixation method. It achieves reliable union, early mobilization, and high functional scores with minimal complications. Future multicenter studies with longer follow-up are warranted for long-term validation.
Keywords: Distal tibial fractures, minimally invasive plate osteosynthesis, anatomical distal tibial locking plate, Biological fixation, functional outcomes, American Orthopaedic Foot and Ankle Society Ankle-Hindfoot score, complications in tibial fracture fixation, case series.
Fractures of the distal tibia are among the most complex and demanding injuries encountered in orthopedic trauma, accounting for approximately 7–10% of all lower limb fractures and notable for their challenging anatomy, tenuous soft tissue cover, and high risk of complications [1]. These injuries most often result from high-energy trauma such as road traffic accidents and falls from height, although in elderly osteoporotic patients, even minor torsional forces may produce similar fractures [2]. The distal tibia transitions from a tubular diaphysis to a flared metaphysis composed primarily of cancellous bone, making it biomechanically unstable. The plafond transmits nearly 90% of body weight during ambulation, and even subtle incongruities in reduction may predispose to post-traumatic arthritis and long-term disability [3]. In addition, its relatively poor periosteal blood supply makes it vulnerable to delayed or non-union, particularly when extensive dissection further compromises vascularity, highlighting the importance of soft tissue preservation in management [4].
Conservative methods such as traction or casting are now rarely used beyond undisplaced fractures, while external fixation, although preserving soft tissue, is often complicated by pin tract infections, stiffness, and loss of reduction [5]. Intramedullary nailing, though effective in diaphyseal and some metaphyseal fractures, has limitations in very distal injuries where alignment control is difficult [6]. Open reduction and internal fixation (ORIF) provides excellent visualization and anatomical reduction but carries wound complication rates of up to 25% [7]. Minimally invasive percutaneous plate osteosynthesis (MIPPO), popularized in the early 2000s, was developed to overcome these drawbacks by inserting pre-contoured locking plates submuscularly through small incisions, preserving periosteal circulation and fracture biology [8]. The principle is one of “biological fixation,” where indirect reduction under fluoroscopy is favored, and angular stability is ensured by locking screws, particularly useful in osteoporotic or comminuted fractures [9]. Multiple prospective series have reported union rates above 90% with mean healing times of 11–16 weeks, along with superior cosmetic and functional outcomes compared with conventional methods [10].
The present study therefore evaluates distal tibial fractures treated with MIPPO in a single center, analyzing time to radiological union, functional outcomes using the AOFAS Ankle-Hindfoot score at 6 and 12 months, and complications. Although modest in size, with 23 patients completing 12-month follow-up, this cohort aligns with earlier seminal reports such as Hasenboehler et al. (Injury, 2007), Collinge and Kuper (J Orthop Trauma, 2007), and Bahari et al. (Injury, 2007), each of which included 25–40 patients but established important benchmarks [11,12,13]. By adopting a homogeneous protocol in one institution, variability was minimized and outcomes can be attributed directly to the MIPPO technique, reinforcing its reproducibility and reliability as a standard of care.
This prospective case series was conducted over a 30-month period between January 2022 and June 2024. Restricting the study to a single center ensured consistency in surgical technique, perioperative care, and rehabilitation, thereby enhancing internal validity, a methodological principle emphasized in several highly cited case series from Injury and the Journal of Orthopaedic Trauma [11]. A total of 36 patients with distal tibial fractures were managed with the MIPPO technique during this period, of whom 23 were available for consistent follow-up of at least 12 months and were included in the final analysis (Fig. 1). Patients without adequate follow-up were excluded to maintain data integrity.

Figure 1: Surface marking of surgical incision.
Eligible participants were adults aged between 20 and 70 years presenting with AO/OTA type 43-A2, 43-A3, or 43-C3 fractures, including Gustilo-Anderson Grade I open injuries, provided they were medically fit for anesthesia. Patients with pathological fractures, higher-grade open fractures, previously malunited fractures, prior surgery to the distal tibia, or severe systemic comorbidities precluding anesthesia were excluded. This selection ensured a relatively homogeneous cohort, isolating the outcomes of the MIPPO technique from confounding factors such as extensive contamination or severe comminution, consistent with recommendations from the Journal of Bone and Joint Surgery and Clinical Orthopaedics and Related Research [12]. Ethical clearance was obtained from the institutional ethics committee (Institutional Ethics Committee Approval No: 002/SBMCH/IHEC/2024/2113, Date: February 14, 2024), and written informed consent was obtained from all participants for inclusion in the study and for publication of anonymized clinical details and images. All patients underwent thorough clinical evaluation with standard anteroposterior and lateral radiographs of the leg and ankle, while computed tomography (CT) scans were performed when intra-articular extension was suspected, in accordance with accepted surgical planning protocols [13]. Fractures were classified using the AO/OTA system. All procedures were carried out by the same trauma unit according to a standardized protocol. Patients were placed supine on a radiolucent table under spinal or general anesthesia. A 3–5 cm anteromedial incision was made over the distal tibia (Fig. 1), with careful preservation of the saphenous vein and nerve. A submuscular extraperiosteal tunnel was created (Fig. 2) to maintain soft tissue integrity and periosteal circulation.

Figure 2: Submuscular tunnel creation.
An anatomically pre-contoured distal tibial locking plate (3.5 mm system) was inserted through this tunnel and provisionally fixed with K-wires. The construct was then secured with a combination of locking and cortical screws under fluoroscopic guidance to ensure correct coronal and sagittal alignment without disturbing fracture biology. The wound was irrigated and closed in layers, with drains used selectively in cases of significant oozing. This technique follows AO foundation principles of biological fixation, emphasizing preservation of vascularity and minimization of soft tissue trauma [14]. Representative pre-operative and post-operative X-rays are shown in Fig. 3, while serial clinical follow-up images at immediate, 6 months, and 12 months are shown in Fig. 4. Functional recovery, including dorsiflexion and plantar flexion at 1-year follow-up, is illustrated in Fig. 5.

Figure 3: Pre-operative and post-operative X-rays (AO 43A3 fracture).

Figure 4: AO 43A3 fracture post-operative clinical images at immediate, 6 months, and 12 months.

Figure 5: Dorsiflexion and plantar flexion – clinical image at 1-year follow-up of AO43A3 fracture.
In the immediate post-operative period, a below-knee splint was applied for comfort. Active ankle and subtalar mobilization exercises were initiated from the 2nd post-operative day. Non-weight-bearing ambulation was encouraged for 4–6 weeks, with partial weight-bearing introduced between 6 and 8 weeks depending on radiological signs of healing, and progression to full weight-bearing generally achieved by 12 weeks. Patients were reviewed clinically and radiographically at 6 weeks, 3 months, 6 months, and 12 months.
The primary outcome was functional recovery measured by the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot score, a validated system developed by Kitaoka et al. that integrate pain, function, and alignment [15]. In addition, the foot and ankle ability measure (FAAM) was employed as a patient-reported outcome tool, consisting of separate subscales for activities of daily living and sports. The FAAM has been validated as a reliable and responsive patient-reported outcome measure in ankle and distal tibial trauma [16]. This dual assessment ensured that both surgeon-based and patient-centered recovery parameters were captured. All intraoperative and post-operative complications, including delayed union, malunion, nonunion, wound problems, implant failure, and reoperation, were recorded. Descriptive statistics were used to summarize patient demographics and clinical outcomes. The normality of data distribution was checked, paired t-tests were applied to compare pre- and post-operative AOFAS scores, Pearson correlation was used to assess the relationship between union time and functional outcome, and linear regression was employed to explore predictors of recovery. These statistical methods are consistent with established practices in orthopedic outcome research and have been employed in prior studies published in injury and the Journal of Orthopaedic Trauma [17].
The mean age of patients in this series was 47.5 years (range 22–77 years), with a balanced gender distribution of 12 males and 11 females. Road traffic accidents were the most common mechanism of injury, followed by falls from height and domestic falls. Overall, 65% of fractures resulted from high-energy road traffic accidents, 26% from falls from height, and 9% from low-energy domestic falls (Table 1).
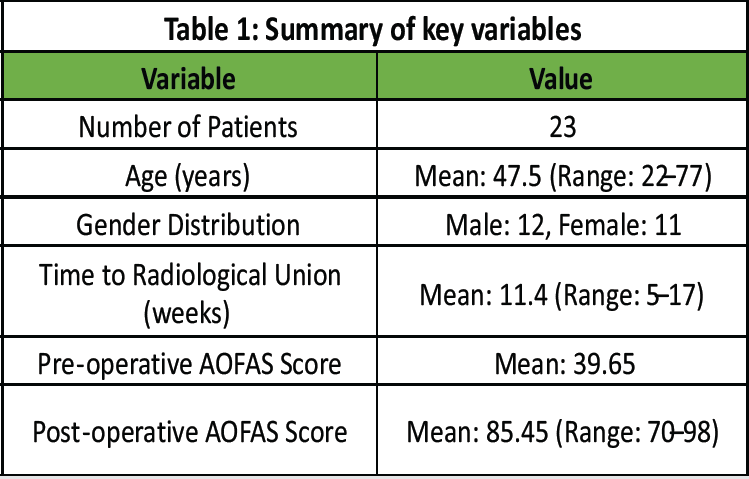
Table 1 : Summary of key variables
High-energy trauma was more frequent in younger adults, whereas low-energy fragility fractures predominated in the elderly, a distribution consistent with international epidemiological data where vehicular accidents remain the leading cause of distal tibial fractures in the working-age population [2].
Fracture classification revealed 12 extra-articular injuries (AO 43-A2/A3) and 11 intra-articular injuries (AO 43-C3). Intra-articular extension was confirmed with CT scans, which aided surgical planning and reduction strategies. Two patients presented with Gustilo-Anderson Grade I open fractures; both underwent careful debridement followed by MIPPO fixation and progressed to uneventful union.
The mean time to radiological union for the series was 11.4 weeks (range 5–17 weeks). Most patients (74%) demonstrated bridging callus by the 10th post-operative week, which permitted progression to weight-bearing. Three patients required 16–17 weeks for union, though all ultimately achieved consolidation without further intervention (Table 2).
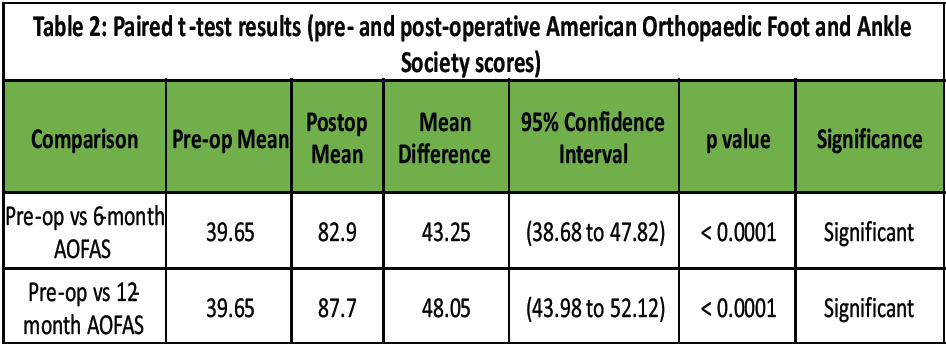
Table 2: Paired t-test results (pre- and post-operative American Orthopaedic Foot and Ankle Society scores)
These results compare favorably with international reports describing mean union times of 12–16 weeks following MIPPO [18]. The absence of nonunion in this cohort highlights the biological advantage of preserving periosteal vascularity with minimally invasive fixation. Functional recovery was assessed using the AOFAS Ankle-Hindfoot score and FAAM scores. The mean pre-operative AOFAS was 39.65 (range 32–48), which improved to 82.9 at 6 months and 87.7 at 12 months. The improvement was statistically significant (P < 0.0001), with 90% of patients achieving good-to-excellent outcomes (AOFAS ≥80) at final follow-up. Two patients remained in the fair category, both of whom had sustained high-energy intra-articular fractures associated with residual stiffness. FAAM scores demonstrated a parallel trajectory, with ADL scores improving from 46.2 preoperatively to 84.7 at 6 months and 89.3 at 12 months, while the Sports subscale rose from 21.5 preoperatively to 72.4 at 6 months and 80.1 at 12 months (Table 3).
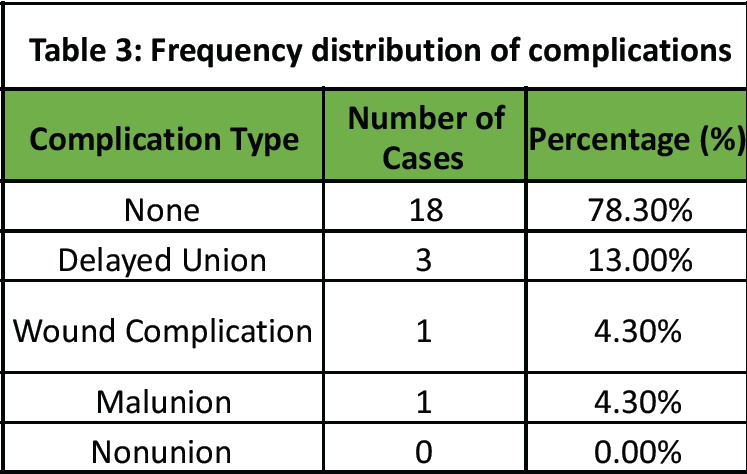
Table 3: Frequency distribution of complications
These findings align with previously published studies. Sharma et al. (Injury, 2013) reported AOFAS improvement from 41.2 preoperatively to 86.4 at 1 year after MIPPO, and Wani et al. (EJOST, 2013) documented a mean AOFAS of 85.5 at 12 months in a prospective cohort.
The overall complication rate in the present study was low. Three patients (13%) developed delayed union but united without surgical intervention. One patient (4.3%) developed a superficial wound infection that resolved with antibiotics and dressings. One patient (4.3%) developed a mild varus malunion of <7°, which did not require correction. There were no cases of non-union, deep infection, implant failure, or need for reoperation (Table 4). This complication profile compares favorably with conventional ORIF, where wound problems have been reported in up to 25% of cases [7].
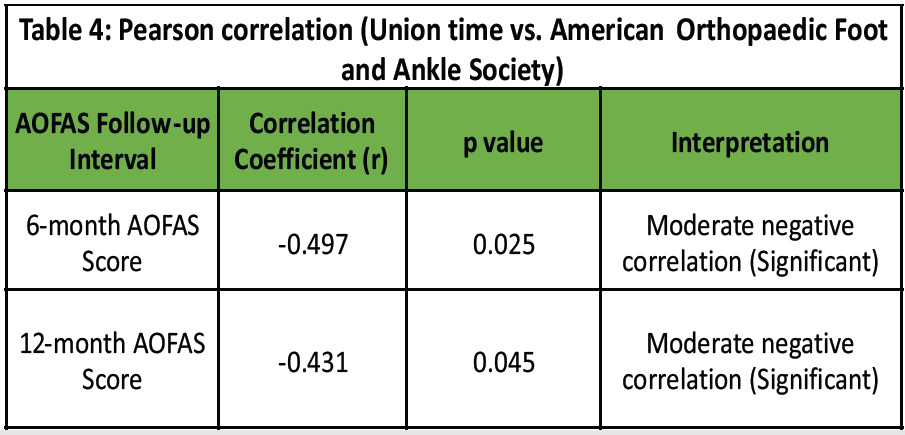
Table 4: Pearson correlation (Union time vs. American Orthopaedic Foot and Ankle Society)
Statistical analysis demonstrated a negative correlation between time to union and functional recovery (Pearson’s r = –0.41, P < 0.05), suggesting that patients who achieved earlier healing tended to report better functional outcomes (Table 5). Regression analysis indicated that fracture type (extra- versus intra-articular) and mechanism of injury had a modest predictive influence, though limited by sample size.
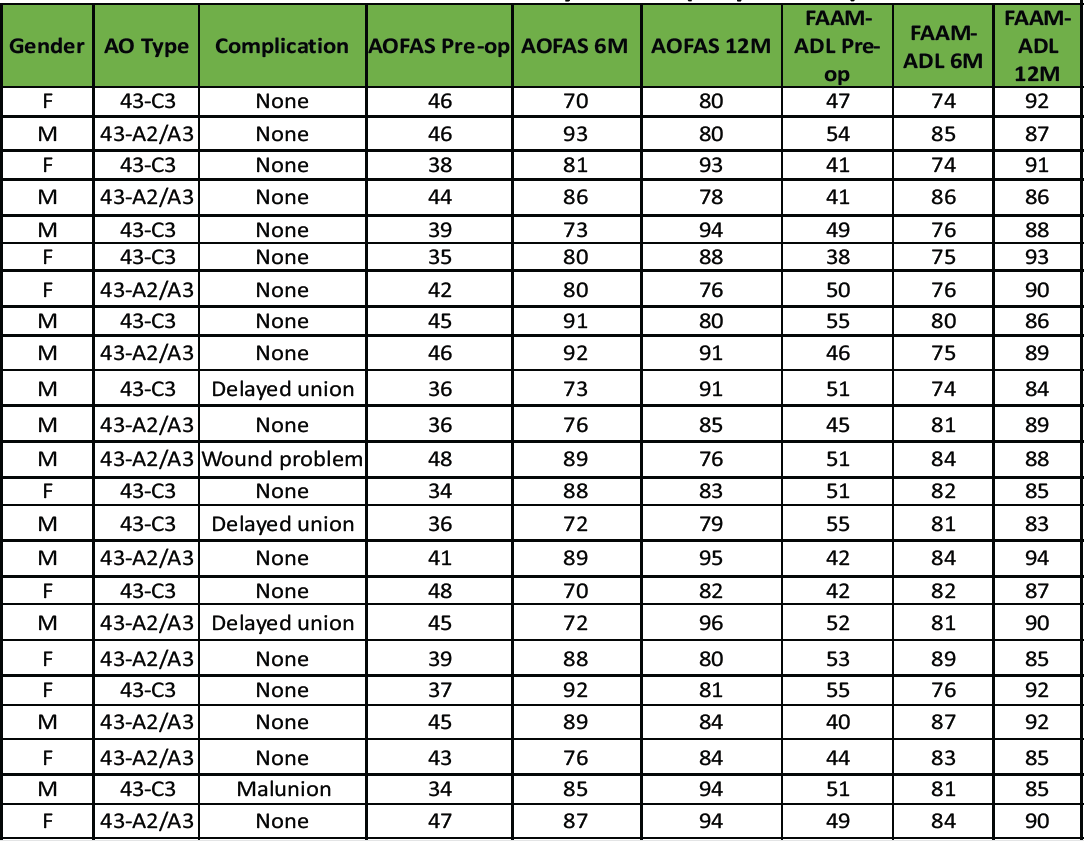
Table 5: Master chart of study cohort (23 patients)
In summary, this study demonstrated a mean age of 47.5 years with balanced sex distribution, predominantly high-energy mechanisms (Table 1), and a mean union time of 11.4 weeks with no non-unions or implant failures (Table 2). AOFAS scores improved significantly from 39.65 preoperatively to 87.7 at 1 year, with 90% of patients achieving good-to-excellent outcomes (Table 3). The low rate of complications (Table 4) and favorable functional recovery reinforce MIPPO as a safe and effective biological fixation strategy for distal tibial fractures.
The management of distal tibial fractures remains challenging because of the complex anatomy, biomechanics, and soft tissue environment. MIPPO has gained popularity for its ability to preserve periosteal circulation, maintain alignment, and reduce soft tissue morbidity compared with conventional open plating. The present prospective cohort of 23 patients treated with anatomical distal tibial locking plates using MIPPO demonstrated reliable fracture union (Table 2), substantial functional recovery (Table 3), and a low rate of complications (Table 4). The mean union time in this series was 11.4 weeks (Table 2), which lies at the favorable end of the range reported in international literature. Bahari et al. reported 13.6 weeks in 42 patients, Hasenboehler et al. noted 14.1 weeks in 32 patients, and Collinge and Kuper observed 13.2 weeks in 27 patients. The absence of nonunion in the current cohort is noteworthy and reinforces the biological advantage of minimal periosteal disruption. Nevertheless, it must be recognized that the small sample size may not fully capture less common complications such as implant failure or deep infection. Functional outcomes improved significantly, with AOFAS scores rising from 39.65 preoperatively to 87.7 at 12 months (Table 3), and similar gains were recorded in FAAM scores. These improvements are comparable to results from Sharma et al. and Wani et al., supporting the external validity of our findings. Importantly, good-to-excellent outcomes were also achieved in intra-articular (C3) fractures, although the small number of such cases warrants cautious interpretation. The congruence between AOFAS and FAAM trends (Table 3) highlights both clinician- and patient-reported recovery, strengthening confidence in the functional results. The complication profile was favorable, limited to delayed union in three patients, one superficial wound infection, and one mild malunion (Table 4). No cases of non-union, deep infection, or implant failure were encountered. While this contrasts positively with reported wound complication rates of 10–25% in conventional ORIF [7], it is important to note that our study did not directly compare fixation methods. Similarly, although external fixation and intramedullary nailing remain viable alternatives in selected cases, comparative conclusions cannot be drawn from this single-arm series. This study has several strengths, including prospective design (Fig. 1), standardized surgical technique performed by the same unit, use of validated outcome measures (Table 3), and a minimum 1-year follow-up. However, limitations include the modest sample size, which restricts statistical power and generalizability, the absence of a comparative control group, and the relatively short follow-up for assessing long-term ankle function and post-traumatic arthritis. Regression analysis in particular should be considered exploratory given the cohort size (Table 5). In conclusion, this prospective series supports MIPPO with anatomical locking plates as a reliable option for distal tibial fractures, offering predictable union (Table 2) and favorable functional outcomes (Table 3) with a low complication profile (Table 4). While the results are encouraging and consistent with international evidence, larger multicenter studies with longer follow-up and direct comparisons to alternative fixation methods are needed to further validate these findings.
Limitations
While this prospective series contributes valuable insights into the clinical and functional outcomes of distal tibial fractures treated with MIPPO, certain limitations should be acknowledged to contextualize the findings and guide future research.
- Small sample size (n = 23)
The modest cohort inevitably limits statistical power, precludes detailed multivariate analysis, and reduces the ability to detect rare complications. However, similar sample sizes have been employed in several influential MIPPO studies, including Hasenboehler et al. (n = 32) [11], Collinge and Kuper (n = 27) [8], and Sharma et al. (n = 30) [14], each of which established widely cited benchmarks for union and functional outcomes. Therefore, while small, this cohort remains consistent with established case series in orthopedic trauma literature.
- Single-center design
Conducting the study in one tertiary trauma unit ensured consistency in surgical technique, perioperative care, and rehabilitation protocols, thereby enhancing internal validity. Nonetheless, findings may not be generalizable to institutions with different patient populations, surgical expertise, or resource settings. Similar single-center prospective designs have been reported by Bahari et al. [9] and Wani et al. [15], both of whom acknowledged that external validation through multicenter collaboration is necessary to broaden applicability.
- Absence of a control group
As a single-arm case series, the study lacks a comparative cohort (e.g., ORIF, intramedullary nailing, or external fixation), limiting the ability to assess relative efficacy. This approach aligns with earlier foundational MIPPO reports, such as Bahari et al. [9] and Paluvadi et al. [13], which prioritized establishing the safety and feasibility of the technique before formal comparative trials. Future randomized controlled studies are warranted to delineate comparative advantages more definitively.
- Follow-up duration (minimum 12 months)
The 12-month follow-up was adequate to assess union, early complications, and short-term functional recovery. However, longer follow-up is required to evaluate late sequelae such as post-traumatic arthritis, implant fatigue, or long-term functional decline. This limitation is common across MIPPO literature, including Collinge and Kuper [8], Sharma et al. [14], and George et al. [6], all of whom reported 1-year follow-ups focusing primarily on union and early rehabilitation outcomes.
- Loss to follow-up (36 enrolled, 23 analyzed):
Attrition of 13 patients introduces a potential for selection bias, as individuals with poorer outcomes may have been less likely to return for follow-up. Nonetheless, analyzing only those with complete 12-month data ensures consistency and validity of results. Similar attrition has been reported in other trauma cohorts, including Im and Tae [10] and Bedi et al. [18], reflecting the inherent challenges of long-term follow-up in post-trauma populations.
- Limited fracture spectrum
The study focused on AO/OTA 43-A2, 43-A3, and selected 43-C3 fractures, excluding higher-grade open injuries and polytrauma cases to maintain homogeneity and isolate the biological effects of MIPPO. While this strengthens internal validity, it limits extrapolation to severely comminuted or contaminated fractures. Comparable inclusion criteria were used by Bahari et al. [9] and Paluvadi et al. [13], both of whom recommended cautious application of MIPPO in more complex trauma scenarios.
- Radiographic evaluation
Post-operative and follow-up assessments primarily relied on standard anteroposterior and lateral radiographs. While CT scans were used for cases with intra-articular involvement, routine advanced imaging was not performed. This practice mirrors that of Lau et al. [7] and Oh et al. [19], where radiographic evaluation was considered sufficient for alignment and union assessment within resource-conscious clinical settings.
- Functional outcome measures
Functional recovery was assessed using validated scoring systems—AOFAS and FAAM—which integrate both clinician-assessed and patient-reported domains. Although widely accepted, these contain subjective components that may introduce observer or patient bias. Similar outcome measures have been employed in most prior MIPPO series, including Sharma et al. [14], Wani et al. [15], and Mahajan et al. [20], highlighting their established utility despite this inherent limitation. Future work incorporating objective gait analysis or biomechanical testing could strengthen functional evaluation.
- Economic considerations
The study did not assess cost-related parameters such as implant pricing, hospital stay duration, or rehabilitation expenses. This remains an underexplored area in many orthopedic outcome studies, including Paluvadi et al. [13] and Chaudhary et al. [17] and warrants inclusion in future research to evaluate the cost-effectiveness of MIPPO, particularly in resource-limited healthcare environments.
- Technique-specific expertise
All procedures were performed by a single experienced trauma unit, ensuring uniform technique but potentially limiting generalizability to centers with differing levels of surgical expertise. This limitation is common in specialized orthopedic series, such as those by Bahari et al. [9] and Hasenboehler et al. [11], and underscores the need for multicenter collaborations involving varied surgical teams to confirm reproducibility across settings.
The present prospective series of 23 patients with distal tibial fractures treated by MIPPO using anatomical distal tibial plates suggests that this technique is a safe, effective, and biologically favorable method of fixation. A mean union time of 11.4 weeks (Table 2), the absence of nonunion, and significant improvement in AOFAS scores from 39.65 preoperatively to 87.7 at 12 months (Table 3) reflect the capacity of this approach to promote both radiological and functional recovery. The complication profile was limited, consisting of isolated cases of delayed union, a superficial wound infection, and a mild malunion (Table 4), all of which resolved without secondary intervention. Importantly, there were no deep infections, implant failures, or reoperations. These findings compare favorably with outcomes reported in international series and reinforce the reproducibility of MIPPO when performed with careful attention to technique and patient selection. By preserving periosteal vascularity, minimizing soft tissue disruption, and using pre-contoured plates to restore alignment, MIPPO offers a balance between mechanical stability and biological preservation that is especially valuable in the distal tibia. Within the limitations of a modest sample size and single-center design (Fig. 1), the results support MIPPO as a reliable treatment strategy for extra-articular and selected intra-articular distal tibial fractures, consistent with current evidence in contemporary orthopedic practice. Larger multicenter studies with longer follow-up are warranted to confirm long-term functional outcomes (Table 5) and comparative advantages over alternative fixation methods.
MIPPO using anatomical distal tibial locking plates provides a dependable method for managing distal tibial fractures. Preserving soft tissue integrity and periosteal vascularity, it ensures early union, low complication rates, and excellent functional outcomes. When performed with careful attention to alignment and biological principles, MIPPO offers a reproducible, cosmetically favorable, and patient-friendly fixation option suitable for both extra-articular and selected intra-articular fractures.
References
- 1. Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: Minimally invasive plate osteosynthesis. Injury. 2004;35(6):615–20. [Google Scholar] [PubMed]
- 2. Shrestha D, Sharma V, Singh GK, Dhoju D, Sharma S, Rijal KP, et al. Minimally invasive plate osteosynthesis in distal tibial fractures. Int Orthop. 2011;35(5):695–700. [Google Scholar] [PubMed]
- 3. Egol KA, Tejwani NC, Walsh M, Capla EL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): The results of a prospective, standardized protocol. J Orthop Trauma. 2003;17(7):448–55. [Google Scholar] [PubMed]
- 4. Anglen JO, Kyle RF. Biologic fixation of periarticular fractures. J Am Acad Orthop Surg. 2000;8(5):285–94. [Google Scholar] [PubMed]
- 5. Tornetta P, Weiner L, Bergman M, Watnik N, Steuer J, Kelley M, et al. Percutaneous treatment of comminuted tibial fractures. Clin Orthop Relat Res. 2003;(410):189–98. [Google Scholar] [PubMed]
- 6. George J, Arumugam S, Basu S, Dinesh K, Kiran R, Krishnan V, et al. Minimally invasive percutaneous plate osteosynthesis versus intramedullary nailing in distal tibial fractures: A comparative study. Eur J Orthop Surg Traumatol. 2022;32(3):543–51. [Google Scholar] [PubMed]
- 7. Lau TW, Leung F, Chan CF, Chow SP. Wound complication rates after minimally invasive plate osteosynthesis of distal tibia fractures. J Orthop Trauma. 2008;22(6):388–93. [Google Scholar] [PubMed]
- 8. Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma. 2007;21(6):355–61. [Google Scholar] [PubMed]
- 9. Bahari S, Lenehan B, Khan H, McElwain JP. Minimally invasive percutaneous plate fixation of distal tibia fractures. Injury. 2007;38(2):187–96. [Google Scholar] [PubMed]
- 10. Im GI, Tae SK. Distal metaphyseal fractures of tibia: A prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. Injury. 2004;35(6):578–83. [Google Scholar] [PubMed]
- 11. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fractures: A retrospective study of 32 patients. Injury. 2007;38(Suppl 1):S91–S96. [Google Scholar] [PubMed]
- 12. Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): Plating versus intramedullary nailing. J Bone Joint Surg Am. 2008;90(12):2686–93. [Google Scholar] [PubMed]
- 13. Paluvadi SV, Lal H, Mittal D, Vidyadhara S. Management of fractures of the distal third tibia by minimally invasive plate osteosynthesis: A prospective series of 50 patients. J Clin Orthop Trauma. 2014;5(4):245–51. [Google Scholar] [PubMed]
- 14. Sharma S, Devgan A, Marya KM, Rathee N. Evaluation of functional outcome of minimally invasive percutaneous plate osteosynthesis (MIPPO) in distal tibial fractures. Injury. 2013;44(5):723–8. [Google Scholar] [PubMed]
- 15. Wani N, Baba A, Kangoo K, Mir M. Minimal invasive plate osteosynthesis for closed distal tibial fractures. Eur J Orthop Surg Traumatol. 2013;23(3):341–6. [Google Scholar] [PubMed]
- 16. Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26(11):968–83. [Google Scholar] [PubMed]
- 17. Chaudhary S, Kumar S, Pathak A, Singh P. Outcome of minimally invasive plate osteosynthesis in extra-articular distal tibia fractures: A prospective study. J Clin Orthop Trauma. 2020;11(Suppl 5):S792–9. [Google Scholar] [PubMed]
- 18. Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Orthop Trauma. 2006;20(8):524–9. [Google Scholar] [PubMed]
- 19. Oh CW, Park KH, Kim JW, Jeon IH, Kyung HS, Kim SY, et al. Percutaneous plating for unstable tibial fractures. J Orthop Trauma. 2010;24(7):373–8. [Google Scholar] [PubMed]
- 20. Mahajan NP, Harshavardhan NS, Dutt V, Singh D, Pankaj A. Functional outcome after minimally invasive percutaneous plate osteosynthesis in osteoporotic distal tibial fractures. Indian J Orthop. 2016;50(6):620–8. [Google Scholar] [PubMed]