PRP injections offer a longer-lasting and more effective alternative to corticosteroids and saline for managing chronic shoulder impingement syndrome, highlighting the role of biologic therapies in enhancing tendon healing and reducing pain in degenerative shoulder conditions.
Dr. Adnan Asif, Department of Orthopaedics, M S Ramaiah Medical College, Bengaluru, Karnataka, India. E-mail: adnan.asif1092@gmail.com
Introduction: Shoulder impingement syndrome (SIS) is a common cause of chronic shoulder pain, often impairing daily function. Various subacromial injection therapies are employed, including corticosteroids and platelet-rich plasma (PRP), though their comparative efficacy remains under investigation.
Aims and Objectives: This study aims to assess and compare the effectiveness of subacromial injections of PRP, corticosteroids, and normal saline on pain relief in chronic SIS using the Visual Analog Scale (VAS).
Materials and Methods: This descriptive epidemiological study involved 150 patients aged over 40 years with shoulder pain lasting more than 3 months and positive clinical signs of impingement. Patients were randomly divided into three groups of 50 each: PRP Group, Steroid Group, and Normal Saline Group. A single subacromial injection was administered through the posterior approach. VAS scores were recorded during overhead activities at 4, 12, and 24 weeks post-injection.
Results: All three groups were comparable in terms of demographic and baseline clinical characteristics. Significant pain reduction was observed in the PRP group across all follow-up intervals compared to the steroid and saline groups. The steroid group showed early pain relief, which diminished over time, while the saline group showed minimal change.
Conclusion: PRP injections demonstrated superior and sustained pain relief in patients with chronic SIS compared to corticosteroids and saline. PRP offers a promising, minimally invasive treatment alternative with long-term benefits, whereas corticosteroids may be more suitable for short-term symptom control.
Keywords: Shoulder impingement syndrome, platelet-rich plasma, Visual Analog Scale, subacromial injection, corticosteroid injection
Shoulder impingement syndrome (SIS) is a prevalent cause of chronic shoulder pain, particularly in individuals over the age of 40 years, leading to significant functional limitations in daily and occupational activities. It is characterized by pain exacerbated by overhead movements, often resulting from compression of the rotator cuff tendons beneath the acromion. Conservative treatment modalities include physiotherapy, oral analgesics, and various forms of subacromial injections. Among these, corticosteroids have been widely used due to their potent anti-inflammatory effects. However, recent interest has shifted towards biologic therapies such as platelet-rich plasma (PRP), which may offer longer-lasting relief by promoting tissue healing. Despite the growing use of PRP, there remains a need to establish its clinical efficacy in comparison to corticosteroids and placebo (normal saline). This study aims to evaluate and compare the effectiveness of a single subacromial injection of PRP, corticosteroid, and normal saline in alleviating pain associated with chronic SIS using the Visual Analog Scale (VAS). The main objectives of the study were:
- To assess the effect of subacromial injection of PRP, corticosteroid, and normal saline on pain in patients with chronic SIS.
- To compare the changes in VAS scores at multiple time points post-injection among the three treatment groups.
This hospital-based, descriptive epidemiological study was conducted in the Department of Orthopaedics, Rajiv Gandhi Medical College and Chhatrapati Shivaji Maharaj Hospital, Kalwa, Thane, Maharashtra, India. After obtaining approval from the Institutional Ethics Committee and informed written consent from all participants, 150 patients fulfilling the inclusion criteria were enrolled. Inclusion criteria consisted of age ≥40 years, with shoulder pain duration >3 months, and with a positive clinical test of SIS. Patients with a history of traumatic shoulder pain were excluded from the study.
Participants were randomly assigned to three groups, with patients blinded to their group allocation (n = 50 each):
- Group A: Received a single subacromial injection of PRP
- Group B: Received a single injection of corticosteroid (1 mL of 40 mg/mL methylprednisolone acetate + 5 mL of 1% lidocaine)
- Group C: Received a single injection of normal saline.
All injections were administered via the posterior approach with the patient in a seated upright position. The needle was inserted 1 cm medially and inferiorly to the posterolateral corner of the acromion and directed cephalad, anteriorly, and medially toward the subacromial bursa. The corticosteroid injection fluid contained 1 mL of 40 mg/mL methylprednisolone acetate and 5 mL of 1% lidocaine hydrochloride. For preparation of PRP, 30 cc of peripheral blood was drawn from the antecubital region into tubes containing 3.2% sodium citrate. PRP was prepared using a manual single-spin technique (1800 rpm for 8 min), and the final 2.5 mL PRP was activated with 5.5% calcium chloride (50 μL in 1 mL PRP), before injection to induce the rapid formation of the fibrin clot. All patients were provided with a standardized physiotherapy protocol post the administration of the injection. Pain was assessed using the VAS for overhead activities at baseline, and at 4, 12, and 24 weeks post-injection. VAS scores ranged from 0 (no pain) to 100 (worst imaginable pain), based on a 10 cm scale (1 mm = 1 point).
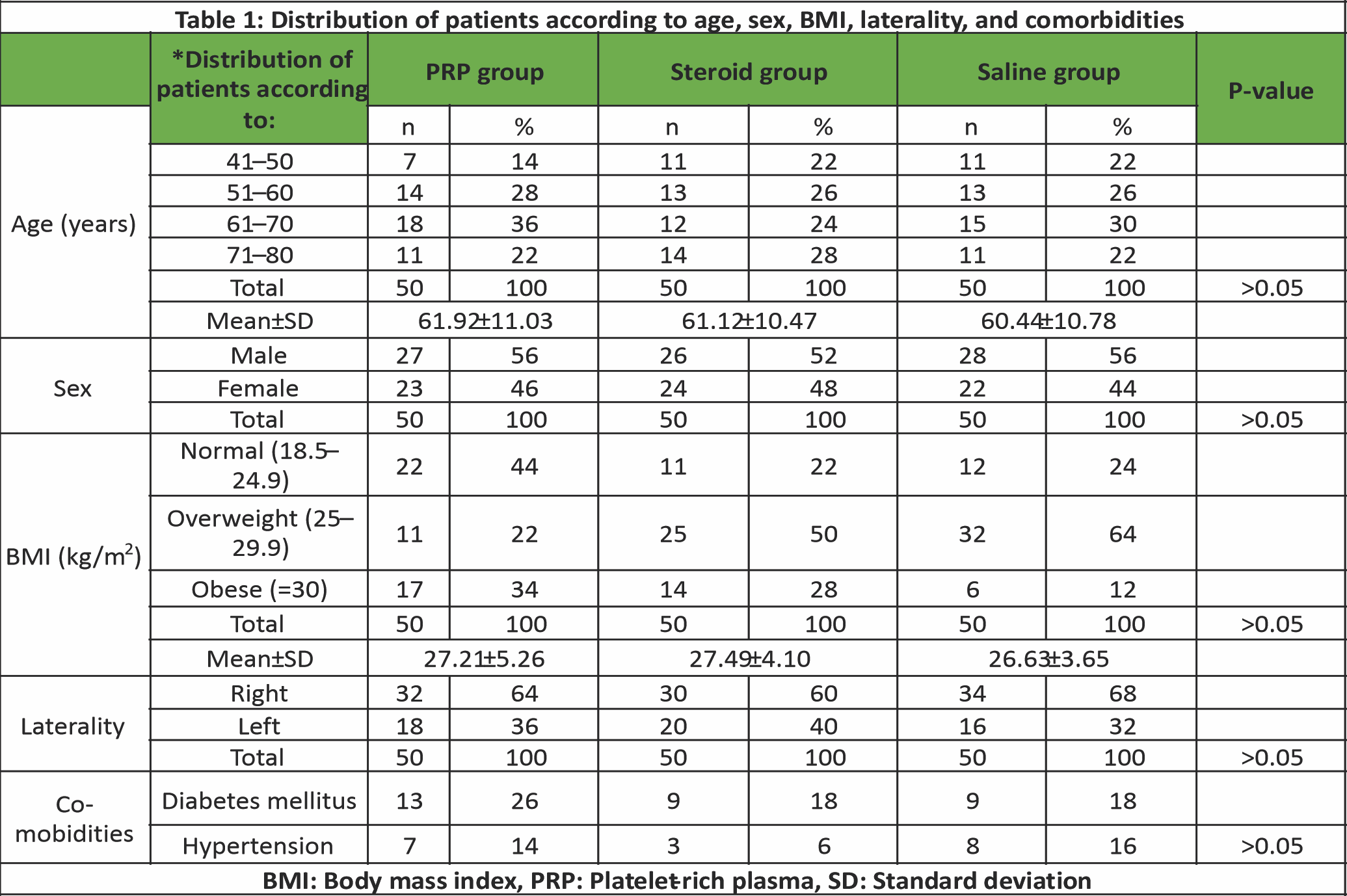
Demographic characteristics showed no statistically significant differences among the three groups in terms of age, sex, body mass index (BMI), side of involvement, or presence of comorbidities (P > 0.05). The mean age across groups was approximately 61 years, with a slight male predominance. The right shoulder was more frequently affected. Comorbid conditions such as diabetes and hypertension were similarly distributed (Table 1).
 The mean symptom duration was 5.85 ± 1.63 months in the PRP group, 5.74 ± 1.23 months in the steroid group, and 5.52 ± 0.96 months in the saline group, with no significant intergroup difference (Table 2).
The mean symptom duration was 5.85 ± 1.63 months in the PRP group, 5.74 ± 1.23 months in the steroid group, and 5.52 ± 0.96 months in the saline group, with no significant intergroup difference (Table 2).
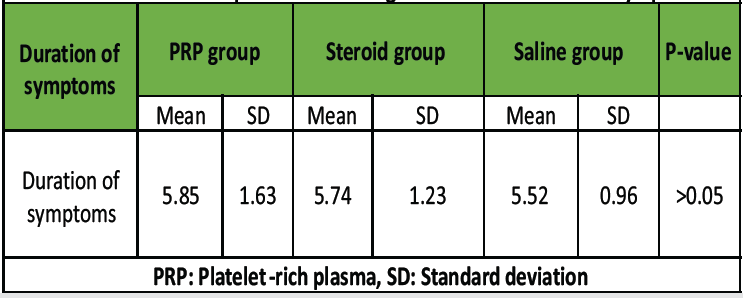
Table 2: Distribution of patients according to the mean duration of symptoms
As far as pain reduction was concerned, all three groups demonstrated statistically significant reductions in VAS scores over time (P < 0.05, analysis of variance). In the PRP group, the VAS reduced from 7.30 ± 0.48 at baseline to 2.51 ± 0.67 at 24 weeks. Similarly, in the Steroid group, VAS reduced from 7.30 ± 0.48 to 4.42 ± 0.50, and the VAS in the saline group reduced from 7.39 ± 0.80 to 5.54 ± 0.50, respectively. Among the three groups, the PRP group showed the greatest and most sustained improvement (Table 3).
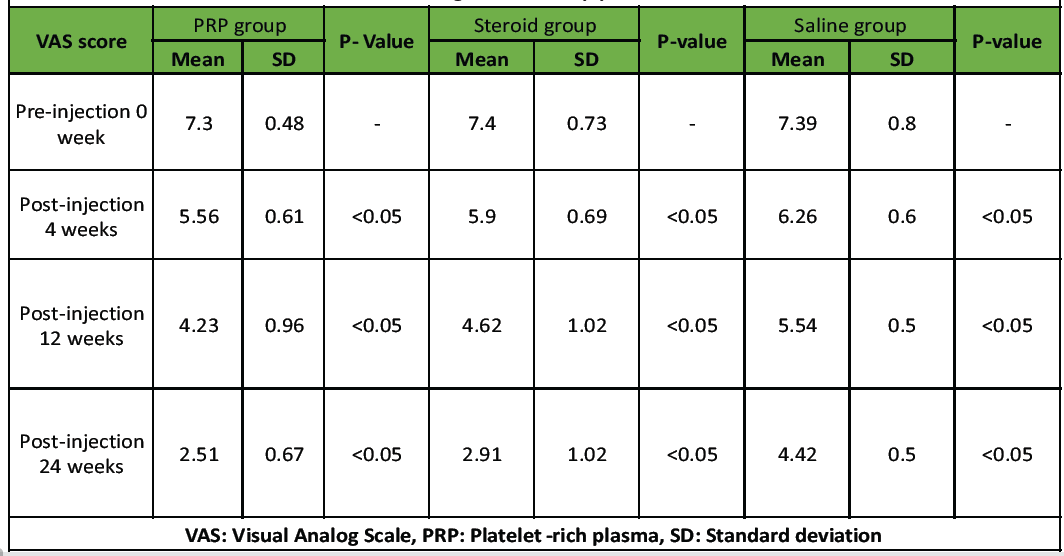
Table 3: Comparison of VAS score within the PRP group, steroid group, and normal saline group, respectively, during the follow‐up period
Based on follow-ups done at 4, 12, and 24 weeks, the PRP group demonstrated significantly superior pain relief compared to the steroid and saline groups (P < 0.05). While the steroid group showed early benefits, its effect plateaued by 12 weeks. The saline group showed the least improvement throughout the follow-up period (Table 4 and Graph 1).
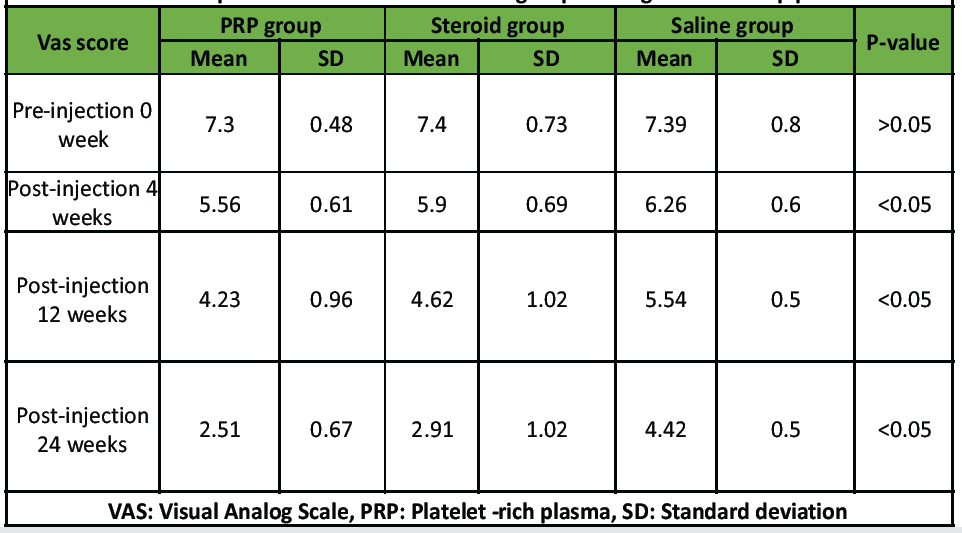
Table 4: Comparison of VAS score between groups during the follow‐up period
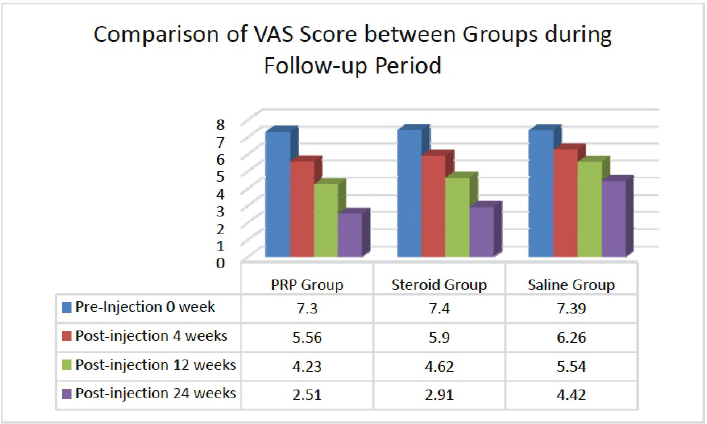
Graph 1: Comparison of Visual Analog Scale score between groups during the follow‐up period.
SIS is a leading cause of chronic shoulder pain, particularly in individuals above 40 years of age. Inflammation, fibrosis, and degeneration of the rotator cuff tendons and subacromial bursa are implicated in its pathophysiology [1,2,3]. Subacromial injections, particularly of corticosteroids and biologics such as PRP, have been widely studied as non-operative treatment options aimed at mitigating pain and enhancing functional recovery. PRP contains a concentrated mixture of platelets suspended in plasma, releasing growth factors such as platelet-derived growth factor, transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF), which play critical roles in angiogenesis, collagen synthesis, and cell proliferation [4,5,6]. This biological potential has positioned PRP as a promising alternative to steroids, particularly in degenerative conditions with poor vascular supply. In the present study, all three treatment groups were comparable with respect to age, gender distribution, BMI, laterality, and comorbidities such as diabetes and hypertension (P > 0.05), minimizing confounding variables. The mean age ranged from 60.44 to 61.92 years, with male predominance noted in all groups, aligning with previous reports [7,8,9,10,11]. The mean BMI was slightly higher in the steroid group (27.49 kg/m2), although not statistically significant (P > 0.05), and a right-sided shoulder dominance was consistently observed across all groups. These findings support the hypothesis that mechanical overuse may contribute to symptom onset and progression, particularly in the dominant limb. VAS score analysis demonstrated that both PRP and corticosteroid injections significantly reduced pain during overhead activity, with PRP showing superior and sustained improvement across all follow-up intervals. The PRP group exhibited a marked reduction from a baseline VAS of 7.30 ± 0.48–2.51 ± 0.67 at 24 weeks, indicating a consistent decline in pain severity over time. This was notably better than the steroid group, where VAS decreased from 7.30 ± 0.48 to 4.42 ± 0.50, and the saline group, which showed the least improvement (7.39 ± 0.80–5.54 ± 0.50). These findings corroborate with prior studies, including those by and Labib, and et al., all of which demonstrated significantly better outcomes in PRP-treated patients over longer follow-up periods [7,9 & 10]. The ability of PRP to release alpha-granules containing biologically active moieties such as TGF-β and VEGF helps to stimulate fibroblast activity, neovascularization, and collagen production, key processes in tendon healing [7,12,13]. Furthermore, the platelet count in PRP is critical for therapeutic efficacy. A platelet concentration 2.5–4 times higher than the peripheral baseline is generally considered optimal [14,15]. In our study, the PRP was activated using calcium chloride, a standard protocol to trigger growth factor release, enhancing local tissue repair. Steroid injections, while effective for short-term pain relief, demonstrated a declining effect by 12–24 weeks, consistent with existing literature [7,11,16]. This highlights their role as a short-term palliative measure rather than a regenerative solution. Normal saline, serving as the control, showed statistically significant but clinically minimal improvement, emphasizing the necessity of active biological or pharmacological intervention for meaningful results. Our findings are further supported by other contemporary studies, including those by Wang et al., Hamid et al., Shams et al., Say et al., and Pasin et al., all of which emphasize the durable analgesic and regenerative benefits of PRP in chronic tendinopathies and impingement syndromes [8,11,16,17,18]. This study has certain limitations that should be acknowledged. As a single-center trial, the results may not be widely generalizable to other populations or healthcare systems with different patient profiles, resources, or procedural expertise. The follow-up period was restricted to 24 weeks, providing only short- to mid-term outcomes and limiting conclusions regarding the long-term durability of PRP or the possibility of late recurrence of pain. Pain relief was evaluated solely using the VAS. While VAS is a reliable tool for pain measurement, the absence of functional outcome scores prevented a more comprehensive assessment of patient recovery. The preparation of PRP in this study was based on a manual single-spin technique, but platelet and growth factor concentrations were not quantified due to the unavailability of equipment. Moreover, no radiological investigation was performed during the study to correlate with the observed clinical findings.
The results of this study support the clinical use of PRP for the management of chronic SIS, demonstrating statistically and clinically superior outcomes compared to corticosteroids and saline. PRP not only alleviates pain but may also enhance tissue regeneration through its biologically active components. While corticosteroids remain helpful for short-term relief, PRP offers a promising longer-term alternative with fewer adverse effects. Larger multi-center trials with longer follow-up and standardized protocols are needed to confirm durability, clarify regenerative effects, and establish cost-effectiveness before PRP can be widely adopted in routine clinical practice.
PRP provides superior and sustained pain relief compared to corticosteroids and saline in chronic SIS. As a safe, minimally invasive, and biologically active treatment, PRP should be considered a preferred non-operative option for long-term management.
References
- 1. Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol) 2003;18:369-79. [Google Scholar] [PubMed]
- 2. Consigliere P, Haddo O, Levy O, Sforza G. Subacromial impingement syndrome: Management challenges. Orthop Res Rev 2018;10:83‐91. [Google Scholar] [PubMed]
- 3. Garving C, Jakob S, Bauer I, Nadjar R, Brunner UH. Impingement syndrome of the shoulder. Dtsch Arztebl Int 2017;114:765‐76. [Google Scholar] [PubMed]
- 4. Kon E, Filardo G, Delcogliano M, Presti ML, Russo A, Bondi A, et al. Platelet‐rich plasma: New clinical application: A pilot study for treatment of jumper’s knee. Injury 2009;40:598-603. [Google Scholar] [PubMed]
- 5. Sanchez M, Anitua E, Orive G, Mujika I, Andia I. Platelet‐rich therapies in the treatment of orthopaedic sport injuries. Sports Med 2009;39(5):345-54. [Google Scholar] [PubMed]
- 6. Nixon AJ, Watts AE, Schnabel LV. Cell‐and gene‐based approaches to tendon regeneration. J Shoulder Elb Surg 2012;21:278-94. [Google Scholar] [PubMed]
- 7. Šmíd P, Hart R, Komzák M, Paša L, Puskeiler M. Léčba impingement syndromuramenapomocíinjekce PRP [Treatment of the shoulder impingement syndrome with PRP injection]. Acta Chir Orthop Traumatol Cech 2018;85:261‐5. [Google Scholar] [PubMed]
- 8. Pasin T, Ataoglu S, Pasin O, Ankarali H. Comparison of the effectiveness of platelet-rich plasma, corticosteroid, and physical therapy in subacromial impingement syndrome. Arch Rheumatol 2019;34:308‐16. [Google Scholar] [PubMed]
- 9. Mahajan A. Clinical and functional outcome comparison for platelet-rich plasma with steroid injection in patients with isolated subacromial impingement syndrome. J Orthop Traumatol Rehabil 2019;11:79‐83. [Google Scholar] [PubMed]
- 10. El Gharbawy NH, Labib HS. Role of platelet rich plasma (PRP) injection in treatment of rotator cuff tear. Egypt Rheumatol Rehabil 2020;47:30. [Google Scholar] [PubMed]
- 11. Wang C, Zhang Z, Ma Y, Liu X, Zhu Q. Platelet‐rich plasma injection vs corticosteroid injection for conservative treatment of rotator cuff lesions: A systematic review and meta‐analysis. Medicine (Baltimore) 2021;100:e24680. [Google Scholar] [PubMed]
- 12. Creaney L, Hamilton B. Growth factor delivery methods in the management of sports injuries: The state of play. Br J Sports Med 2008;42:314‐20. [Google Scholar] [PubMed]
- 13. De Mos M, Van Der Windt AE, Jahr H, Van Schie HT, Weinans H, Verhaar JA, et al. Can platelet-rich plasma enhance tendon repair? A cell culture study. Am J Sports Med 2008;36:1171‐8. [Google Scholar] [PubMed]
- 14. Anitua E. Plasma rich in growth factors: Preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants 1999;14:529-35. [Google Scholar] [PubMed]
- 15. Pietrzak WS, Eppley BL. Platelet rich plasma: Biology and new technology. J Craniofac Surg 2005;16:1043‐54. [Google Scholar] [PubMed]
- 16. Hamid MS, Sazlina SG. Platelet‐rich plasma for rotator cuff tendinopathy: A systematic review and meta‐analysis. PLoS One 2021;16:e0251111. [Google Scholar] [PubMed]
- 17. Shams A, El‐Sayed M, Gamal O, Ewes W. Subacromial injection of autologous platelet‐rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur J Orthop Surg Traumatol 2016;26:837-42. [Google Scholar] [PubMed]
- 18. Say F, Gürler D, Bülbül M. Platelet‐Rich plasma versus steroid injection for subacromial impingement syndrome. J Orthop Surg (Hong Kong) 2016;24:62‐6. [Google Scholar] [PubMed]