Enchondroma of the hand, though often mimicking other lesions, is effectively managed by simple curettage with autologous bone grafting and prophylactic fixation, with early mobilization ensuring excellent functional recovery.
Dr. Gourab Biswas, Department of Orthopaedics, Max Superspeciality Hospital, Delhi NCR, India. E-mail: gourabbiswas2013@gmail.com
Introduction: Enchondroma is the most common benign cartilaginous tumor of the small tubular bones of the hand. Although typically indolent, it may present with pain, swelling, or pathological fracture, and requires careful differentiation from low-grade chondrosarcoma. Management strategies range from observation in asymptomatic cases to surgical curettage with or without grafting in symptomatic lesions.
Case Report: We present three cases of hand enchondroma involving the phalanges in patients aged 20–37 years. Clinical features included fusiform swelling, pain, and, in one case, pathological fracture. Radiographs showed well-circumscribed lytic lesions with chondroid matrix. All cases were treated with intralesional curettage, cavity filling with cancellous autograft harvested from the olecranon, and prophylactic K-wire fixation. Histopathology confirmed enchondroma in each case. Postoperatively, patients underwent short-term immobilization followed by physiotherapy. At 12 weeks, all achieved full functional recovery with radiological consolidation and no recurrence or complications.
Conclusion: Enchondroma of the hand, though benign, requires timely recognition and appropriate surgical management. Curettage with autologous bone grafting and prophylactic fixation offers reliable outcomes with minimal morbidity, while early mobilization reduces the risk of post-operative stiffness, even in cases with pathological fracture.
Keywords: Enchondroma, hand tumors, curettage, bone grafting, pathological fracture.
Enchondromas are slow-growing, benign cartilaginous tumors that usually remain asymptomatic and are often discovered incidentally on radiographs. The natural history is generally indolent, although lesions may present with pain, swelling, or pathological fracture. Rarely, malignant transformation into low-grade chondrosarcoma can occur, particularly in syndromic conditions such as Ollier disease and Maffucci syndrome [1,2]. Management depends on symptoms and fracture risk. Small, asymptomatic enchondromas may be observed with serial radiographs [3]. Symptomatic lesions or those complicated by fracture are typically treated surgically with intralesional curettage. Options for filling the defect after curettage include autologous cancellous bone graft, allograft, synthetic substitutes, or bone cement [3,4]. Some studies suggest that leaving the void unfilled may yield equivalent results [4], while others recommend grafting to enhance consolidation and reduce fracture risk [3,5]. Prophylactic fixation using K-wires or plates may be required when structural stability is compromised [6]. Overall, the prognosis following adequate curettage is excellent, with high rates of bone healing and functional recovery. Recurrence is uncommon provided that meticulous removal is achieved [1,6].
Case 1
A 21-year-old male presented with a 2-month history of painless swelling of the left little finger, which gradually increased in size and caused mild discomfort on gripping. On examination, a fusiform, firm, non-tender bony swelling was palpable over the proximal phalanx with intact skin and preserved digital motion, though mild restriction of terminal flexion was noted. Radiographs revealed a well-circumscribed, expansile lytic lesion with chondroid matrix, consistent with enchondroma. Surgery was performed using a dorsal midline approach; intralesional curettage was followed by filling with cancellous autograft from the ipsilateral olecranon and prophylactic K-wire fixation. Histopathology showed lobules of mature hyaline cartilage containing small, uniform chondrocytes in lacunae, without nuclear atypia or mitoses, confirming benign enchondroma. At 12-week follow-up, radiographs showed complete graft incorporation, and the patient regained full pain-free range of motion with return to daily activities.
Case 2
A 37-year-old female presented with 4 months of pain and swelling in the right index finger, interfering with writing and daily chores. Clinical examination revealed diffuse fusiform swelling of the proximal phalanx, mildly tender to palpation, with partial restriction of flexion at the proximal interphalangeal joint. Radiographs demonstrated a well-defined intramedullary lytic lesion with cortical thinning but no fracture. Surgical management involved curettage through a cortical window, cavity irrigation, and filling with morselized olecranon cancellous graft. Histopathological analysis confirmed enchondroma with typical cartilage lobules and absence of atypical features. The finger was immobilized in a below-elbow splint for 2 weeks, after which physiotherapy was commenced. At 10 weeks, the patient achieved full motion and reported complete resolution of pain, with no radiological evidence of recurrence (Fig. 1).
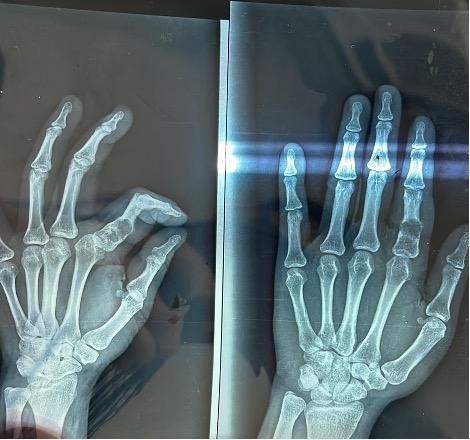
Figure 1: Clinical photograph of fusiform swelling over the proximal phalanx of the right index finger (Case 2) before surgery.
Case 3
A 20-year-old female sustained trivial trauma to the left little finger, followed by acute pain, swelling, and deformity. Radiographs showed an enchondroma of the proximal phalanx complicated by a pathological fracture with cortical breach. A similar dorsal approach was employed; after curettage and grafting with olecranon cancellous bone, prophylactic K-wire fixation was used to stabilize the fracture site. Histopathology demonstrated mature cartilage with uniform chondrocytes, confirming enchondroma without evidence of malignancy. Sutures were removed at 2 weeks, and K-wires at 6 weeks, followed by physiotherapy. By 12 weeks, radiographs showed satisfactory union with graft consolidation. The patient achieved complete functional recovery, including grip and pinch strength, and resumed regular household activities without restriction.
Treatment
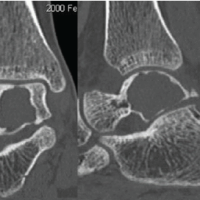
Surgical management was undertaken in all cases. Using a dorsal midline approach, an oval cortical window was created with a low-speed drill. The tumor contents were curetted, the cavity irrigated with hydrogen peroxide and saline, and filled with morselized cancellous bone graft harvested from the ipsilateral olecranon. Prophylactic K-wire fixation was employed to maintain stability and prevent post-operative fracture (Fig. 2). The excised tissue was sent for histopathological evaluation, which confirmed the diagnosis of enchondroma.

Figure 2: Intraoperative image showing creation of dorsal cortical window and curettage of lesion contents.
Follow-up
Sutures were removed at 2 weeks. Physiotherapy was initiated after K-wire removal to prevent stiffness. Radiographs at 6 and 12 weeks demonstrated consolidation of grafts and obliteration of cavities (Fig. 3). All patients regained full range of motion and resumed normal activities without recurrence or complications.

Figure 3: Clinical photograph at follow-up showing restored finger mobility and full range of motion.
Enchondroma is the most frequent benign tumor of the hand, accounting for nearly 70% of primary bone tumors in this region [1,2]. The clinical dilemma lies in distinguishing these indolent lesions from low-grade chondrosarcomas, which often share overlapping radiographic features [1]. Surgical management with intralesional curettage remains the standard of care. The role of post-curettage augmentation continues to be debated. Several authors have demonstrated that void augmentation may not be essential, with comparable recurrence and consolidation rates observed even when the defect is left unfilled [3,4]. Others, however, emphasize the benefits of grafting or substitutes to minimize the risk of fracture and hasten incorporation [5,7]. Our results support the use of locally harvested cancellous autograft, which is easily available, cost-effective, and avoids donor site morbidity associated with iliac crest harvesting.
The timing of surgery in the presence of a pathological fracture is another point of controversy. While some recommend delaying curettage until fracture healing to reduce stiffness [8,9], others have successfully performed immediate intervention with fixation [1]. In our series, prophylactic K-wire stabilization allowed early mobilization, which is critical for maintaining digital motion. Reported complications following enchondroma surgery include joint stiffness, recurrence, and contractures [5,10]. In a large retrospective review, Figl and Leixnering [6] found favorable functional outcomes with low recurrence when meticulous curettage and structured rehabilitation protocols were followed. Similarly, in our cohort, no recurrence or major complication was observed during follow-up, reinforcing the efficacy of early mobilization and structured physiotherapy in optimizing results.
Intralesional curettage with autologous bone grafting and prophylactic fixation provides a safe and effective treatment for symptomatic enchondroma of the hand. Early mobilization following stable fixation minimizes stiffness and optimizes functional recovery, even in the presence of pathological fracture.
Hand enchondromas, though benign, require timely recognition and surgical management. Simple curettage with local autograft and prophylactic fixation offers excellent outcomes with minimal complications.
References
- 1. Sassoon AA, Fitz-Gibbon PD, Harmsen WS, Moran SL. Enchondromas of the hand: Factors affecting recurrence, healing, motion, and malignant transformation. J Hand Surg Am 2012;37:1229-34. [Google Scholar] [PubMed]
- 2. Simon MJ, Pogoda P, Hövelborn F, Krause M, Zustin J, Amling M, et al. Incidence, histopathologic analysis and distribution of tumours of the hand. BMC Musculoskelet Disord 2014;15:182. [Google Scholar] [PubMed]
- 3. Bachoura A, Rice IS, Lubahn AR, Lubahn JD. The surgical management of hand enchondroma without postcurettage void augmentation: Authors’ experience and a systematic review. Hand (N Y) 2015;10:461-71. [Google Scholar] [PubMed]
- 4. Hasselgren G, Forssblad P, Tornvall A. Bone grafting unnecessary in the treatment of enchondromas in the hand. J Hand Surg Am 1991;16:139-42. [Google Scholar] [PubMed]
- 5. Haase SC. Treatment of pathologic fractures. Hand Clin 2013;29:579-84. [Google Scholar] [PubMed]
- 6. Figl M, Leixnering M. Retrospective review of outcome after surgical treatment of hand enchondroma. J Hand Surg Eur 2011;36:450-4. [Google Scholar] [PubMed]
- 7. Yalcinkaya M, Akman YE, Bagatur AE. Recurrent metacarpal enchondroma treated with strut allograft: 14-year follow-up. Orthopedics 2015;38:e647-50. [Google Scholar] [PubMed]
- 8. Lubahn JD, Bachoura A. Enchondroma of the hand. J Am Acad Orthop Surg 2016;24:625-33. [Google Scholar] [PubMed]
- 9. Pietramala S, Rovere G, Ravaioli C, Mignano C, Smakaj A, Fidanza A, Farsetti P, Rocchi L, Fulchignoni C. Surgical Treatment of Enchondromas of the Hand: Our Experience in Curettage Only and Early Mobilization. Diseases. 2025 Mar 16;13(3):84. [Google Scholar] [PubMed]
- 10. Hamoudi C, Bouillet B, Martins A. Malignant transformation of a phalangeal enchondroma into a recurrent grade II chondrosarcoma requiring successive transcarpal amputations: a case report. Case Rep Plast Surg Hand Surg. 2022;9(1):179-84. [Google Scholar] [PubMed]