Tarlov cysts, though often incidental, should be considered in patients, especially females presenting with unexplained vulvar pain. A minimally invasive, image-guided caudal epidural steroid injection, combined with targeted pelvic floor rehabilitation, can offer effective and sustained relief, avoiding the need for surgical intervention.
Dr. J S R G Saran, Department of Orthopaedics, M S Ramaiah University of Applied Sciences, M S R Nagar, New B E L Road, Bengaluru - 560054, Karnataka, India. E-mail: jsaran868@gmail.com
Introduction: Tarlov cysts, or perineural cysts, are cerebrospinal fluid-filled sacs typically located in the sacral region. Although often asymptomatic, larger cysts can compress adjacent nerve roots, leading to radicular pain, pelvic discomfort or dysfunction. Neurogenic vulvodynia caused by such cysts is rare and frequently misdiagnosed, particularly in women with normal gynecological and dermatological evaluations.
Case Report: A 31-year-old nulliparous female presented with a 1-year history of sharp, burning vulvar pain radiating to the perianal region and posterior thigh, significantly impairing daily and sexual activities. Examination was unremarkable except for right ischial spine tenderness. Magnetic resonance imaging revealed a 1.7 × 1.2 × 1.3 cm Tarlov cyst at the right S2 neural foramen compressing the nerve root. After failure of conservative therapy, she underwent fluoroscopy-guided injection of triamcinolone and bupivacaine into the S2 dorsal root sleeve, along with continued physiotherapy and pregabalin.
Results: Within 2 weeks, the patient experienced near-complete symptom relief. At 3 and 6-month follow-ups, she remained asymptomatic. Objective scores improved significantly: Visual Analog Scale reduced from 10 to 2, Oswestry disability index from 44% to 14%, and pelvic floor distress inventory-20 score to zero. She resumed normal activities, including pain-free sexual function.
Conclusion: This case highlights the importance of considering sacral Tarlov cysts in the differential diagnosis of vulvodynia. A multidisciplinary, minimally invasive approach can offer significant symptom relief. However, longer-term studies are warranted to assess durability and recurrence risk.
Keywords: Tarlov cyst, vulvodynia, caudal epidural steroid injection, kegel exercises, bupivacaine, triamcinolone.
Tarlov cysts, or perineural cysts, are cerebrospinal fluid (CSF)-filled sacs most commonly found in the sacral region within the dorsal root ganglion. While often asymptomatic, larger cysts can cause radicular pain, perineal discomfort, bladder or bowel dysfunction and sexual disturbances due to neural compression. Vulvodynia, a chronic vulvar pain lasting over 3 months without an identifiable cause, is a complex condition with a broad differential diagnosis. Neurogenic causes, such as sacral Tarlov cysts, are rarely considered but may underlie persistent symptoms, especially in female patients with negative gynecologic and dermatologic evaluations. Due to their non-specific presentation, symptomatic cysts are frequently misdiagnosed or overlooked. Magnetic resonance imaging (MRI) remains the gold standard for diagnosis, as these cysts are often invisible on plain radiographs. Treatment varies from conservative measures to minimally invasive or surgical interventions, guided by symptom severity and neurological involvement. This case report highlights a rare presentation of symptomatic sacral Tarlov cyst masquerading as vulvodynia in a middle-aged woman, successfully managed through a minimally invasive image-guided injection, underlining the importance of a multidisciplinary and individualized treatment approach.
A 31-year-old nulliparous female presented with a 1-year history of sharp, burning pain localized to the right vulvar region, radiating to the perianal area and posterior thigh. The pain was spontaneous in onset, exacerbated by sitting and prolonged standing and significantly interfered with her daily routine, particularly her ability to engage in sexual activity. There was no history of recent trauma, infection or dermatologic lesions. Multiple prior therapeutic trials, including antifungals, topical steroids, tricyclic antidepressants and Gabapentinoids, offered minimal relief. On clinical examination, the vulvar skin appeared normal, without signs of inflammation or dermatologic pathology. Digital rectal examination revealed localized tenderness over the right ischial spine, suggestive of pudendal nerve irritation. There was no evidence of pelvic organ prolapse, perianal anesthesia or anal sphincter laxity. Her pelvic floor distress inventory-20 (PFDI-20) score was 7.13/300, consistent with minimal distress at presentation. The radiographs were unremarkable (Fig. 1). MRI of the lumbo-sacral spine, including T1-weighted, T2-weighted and short tau inversion recovery sequences, revealed a well-defined perineural (Tarlov) cyst measuring 1.7 × 1.2 × 1.3 cm at the right S2 neural foramen, with displacement and compression of the adjacent S2 nerve root. Mild disc bulges were also noted at L2-L3 and L3-L4 levels (Fig. 2). The lesion was classified as a Type II perineural cyst per Nabor’s classification and no other spinal abnormalities were detected. A diagnosis of neurogenic vulvodynia secondary to S2 nerve root irritation from the Tarlov cyst was established.
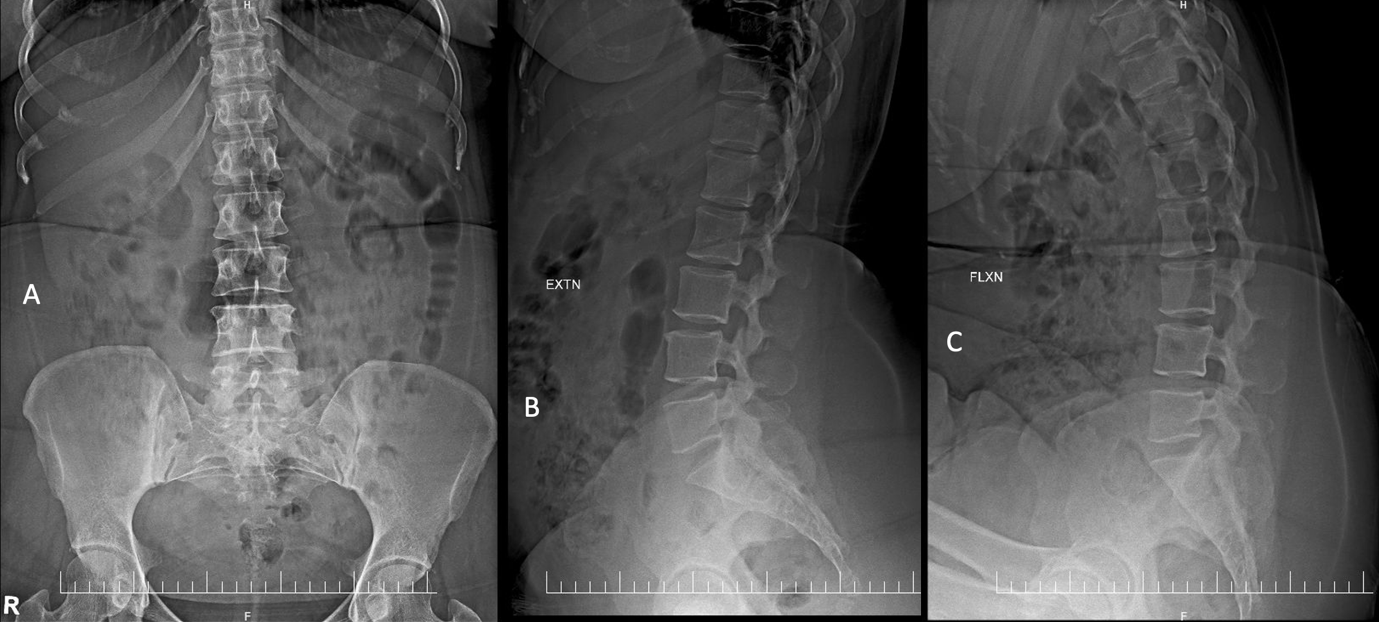
Figure 1: Radiographs of the lumbosacral spine in (a) anteroposterior and lateral extension (b) and flexion (c) views.
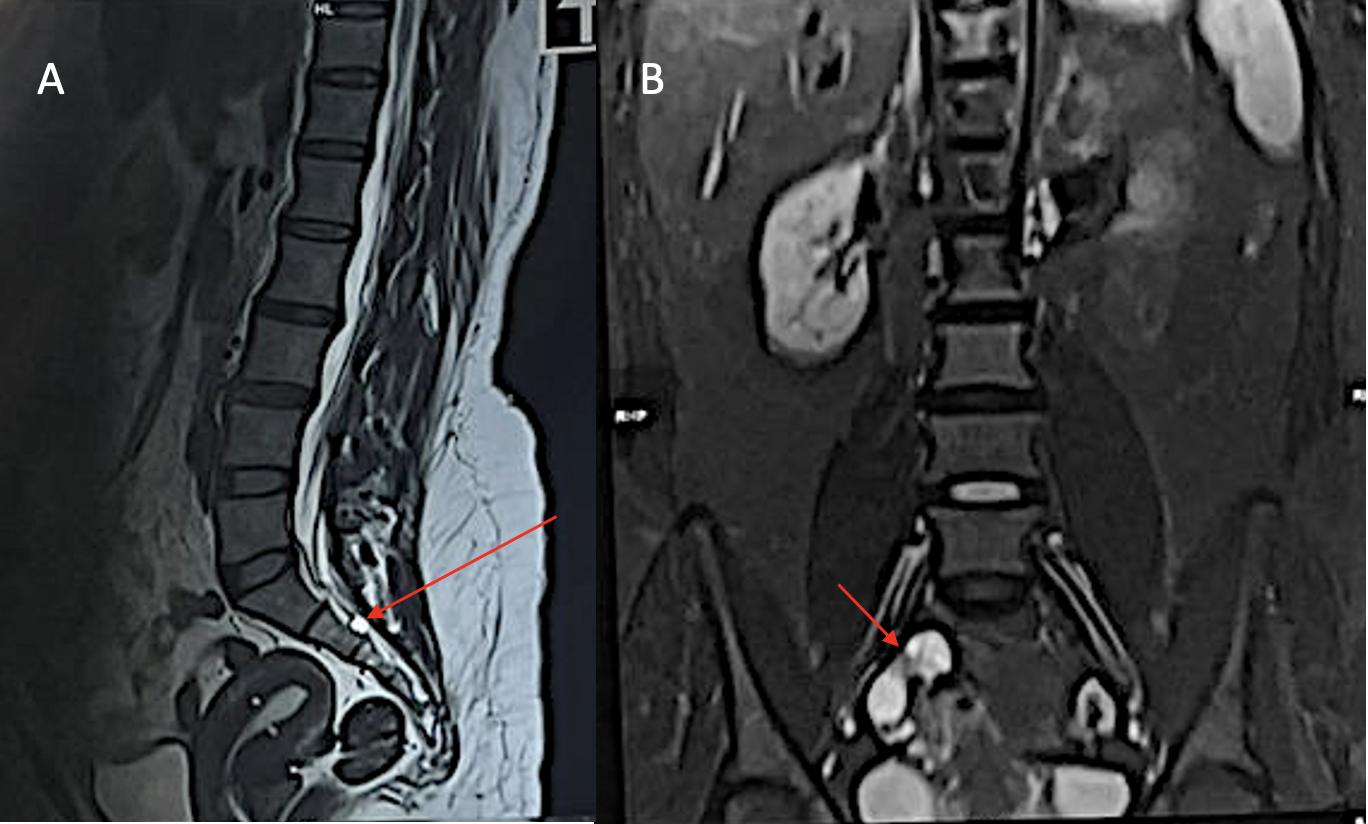
Figure 2: Magnetic resonance imaging showing the Tarlov cyst in T2-weighted sagittal view (a) and the cyst arising from the foramen seen in T2-weighted coronal view (b).
Given the failure of conservative measures and the focal neural compression evident on imaging, the patient underwent a fluoroscopy-guided percutaneous injection targeting the right S2 dorsal root sleeve. Under strict aseptic precautions and prone positioning, the sacral hiatus was localized by palpation. A 22-gauge Crawford epidural needle was advanced under fluoroscopic guidance. After confirming epidural placement with iohexol (Omnipaque) contrast showing the classical “Christmas tree” appearance of the caudal nerve rootlets, 1 mL of 40 mg/mL triamcinolone was combined with 1 mL of 0.5% bupivacaine and injected directly into the affected S2 dorsal root sleeve (Fig. 3). The procedure was uneventful and the patient was discharged the same day (Fig. 4).
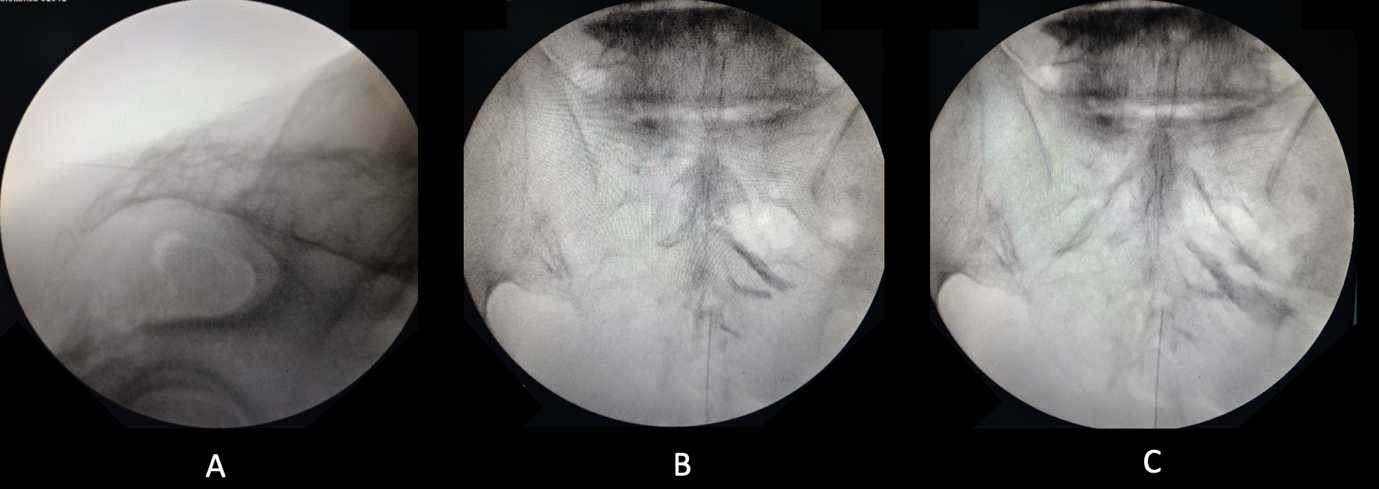
Figure 3: Fluoroscopic image (a) depicting the epidural needle made parallel to the sacrum. Images (b) and (c) show the proper placement of the needle and injection of the iohexol dye, leading to a Christmas tree appearance.
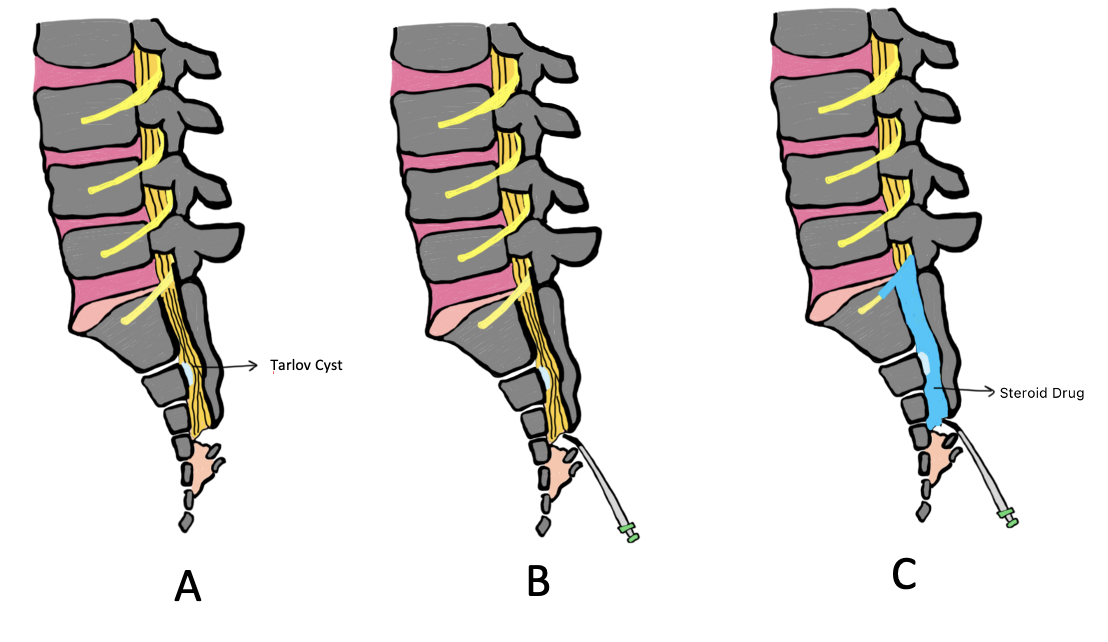
Figure 4: The pictorial representation of the instillation of the caudal epidural steroid drug within the sacral canal.
Post-injection, she was prescribed a tapering course of pregabalin (75 mg daily), non-steroidal anti-inflammatory drugs (NSAIDs) and advised to continue pelvic floor physiotherapy, including Kegel exercises to optimize neuromuscular control and reduce pelvic floor hypertonicity. While the individual contribution of each modality could not be isolated, their synergistic effect likely underpinned the therapeutic success. The patient reported near-complete pain relief within 2 weeks. At 3 and 6-month follow-ups, she remained asymptomatic, had resumed normal occupational activities and was sexually active without discomfort. Her outcome measures demonstrated marked improvement: Visual Analog Scale (VAS) score reduced from 10 to 2, Oswestry disability index (ODI) from 44% to 14% and PFDI-20 score to zero, reflecting complete resolution of pelvic floor-related symptoms. However, the patient was lost to follow-up beyond 6 months, limiting our understanding of the long-term durability of symptom relief and the potential for recurrence. In addition, while the intervention yielded a dramatic short-term benefit, the relative contributions of steroid injection versus concurrent physiotherapy and pharmacotherapy cannot be definitively quantified, and the placebo effect cannot be excluded.
A meningeal cyst or diverticulum is a fluid-filled sac found in the posterior or lateral epidural space of the spinal canal, which is surrounded by fibrous tissue similar to dura mater, but without the presence of the arachnoid membrane [1]. Spinal meningeal cysts are categorized based on the classification system proposed by Nabors et al., which delineates three primary types. Type I cysts are extradural meningeal cysts that do not contain neural tissue and are further subdivided into Type Ia, referring to extradural spinal arachnoid cysts and Type Ib, representing sacral meningoceles. Type II cysts are extradural but differ in that they contain neural elements, with Tarlov cysts being the most recognized example. Type III cysts are entirely intradural and consist of spinal arachnoid cysts [2]. This classification aids in accurate diagnosis and guides appropriate management strategies in clinical practice. In our case, the cyst comes under Type II, i.e., Tarlov cyst. Tarlov cysts are relatively uncommon, with a global prevalence estimated at approximately 4.27%, according to the most recent meta-analysis. In the United States, the prevalence is slightly lower, reported at 3.82%. These cysts demonstrate a higher incidence in females, with a prevalence of 7.01% compared to 4.05% in males. Notably, while the majority of Tarlov cysts are asymptomatic, the same study indicated that approximately 15.59% of cases present with clinical symptoms [3]. In our case, the patient was a symptomatic female, consistent with the demographic and clinical profile more commonly associated with Tarlov cysts. The underlying mechanisms contributing to the formation and progression of Tarlov cysts remain incompletely understood. One hypothesis, originally proposed by Dr. Tarlov, suggests that trauma-induced hemorrhage may lead to hemosiderin accumulation and impaired venous outflow within the nerve sheath, ultimately resulting in cyst formation. Alternatively, a congenital predisposition involving aberrant arachnoid cell proliferation around sacral nerve roots has also been implicated. These cysts typically maintain communication with the subarachnoid space. The most accepted theory regarding their enlargement involves a one-way valve mechanism, where CSF enters the cyst during pulsatile flow but is unable to exit, leading to progressive distension. This expansion may compress adjacent neural elements, contributing to neurological symptoms. In some cases, the pressure exerted by the growing cyst can cause erosion of the sacral bone and irritation of the periosteum, further contributing to pain and functional impairment [4]. In our case, the prior history of fall could be the instigating factor for the formation of the cyst. Since the sacral region is the most frequent site of Tarlov cysts, associated symptoms may include perineal pain, bowel – bladder dysfunction and dyspareunia [5]. In our patient, vulvodynia was the predominant complaint, surpassing back pain in severity and impact. Tarlov cysts are not detectable on plain radiographs and require advanced imaging modalities such as contrast-enhanced computed tomography or, preferably, MRI for accurate visualization. Currently, MRI is considered the gold standard for identifying these thin-walled cystic lesions within the spinal canal [6]. On MRI, they typically appear hypointense on T1-weighted images and hyperintense on T2-weighted sequences [7]. A primary concern during evaluation is the exclusion of cauda equina syndrome, which constitutes a neurosurgical emergency requiring prompt decompression. This was not the case in our patient. Management of symptomatic Tarlov cysts is nuanced and typically individualized. Options range from conservative analgesia to invasive surgical procedures such as cyst fenestration, resection or laminectomy. However, these carry substantial risks, including CSF leaks, infection and iatrogenic nerve injury. In cases with significant symptomatology, percutaneous aspiration followed by sealant injection has been reported to provide symptomatic relief [8]. Image-guided, minimally invasive interventions have emerged as a safer and effective alternative for select patients. Surgical excision is generally reserved for refractory cases where conservative and minimally invasive approaches have failed. Freidenstein et al. reported two cases in which patients presenting with urinary urgency and pain, consistent with interstitial cystitis were treated successfully using caudal epidural anesthesia targeting sacral nerve root Tarlov cysts, with sustained symptom relief observed over a 2-year follow-up period [9]. In our case, a fluoroscopy-guided percutaneous steroid injection into the S2 dorsal root sleeve was performed, using 1 mL of triamcinolone (40 mg/mL) and 1 mL of 0.5% bupivacaine. This approach was chosen due to its favourable risk profile and technical feasibility, despite fluoroscopy offering lower soft-tissue resolution than computed tomography or MRI. The combination of corticosteroid and local anesthetic aimed to reduce inflammation and interrupt the pain pathway, potentially prolonging analgesia. Concurrent pelvic floor physiotherapy, including Kegel exercises and a tapering course of pregabalin and NSAIDs, was also continued. Although the relative contribution of each modality cannot be definitively isolated, their synergistic effect likely played a role in the favorable outcome. While some studies suggest no significant difference in pain outcomes between bupivacaine alone and its combination with agents such as pethidine or triamcinolone, we opted for this combination to potentially extend analgesic duration and facilitate early rehabilitation [10]. The functional and symptomatic status of the patient was evaluated using multiple validated instruments. Pain intensity was assessed using the VAS, ranging from 0 (no pain) to 10 (worst imaginable pain) [11]. Functional disability due to back pain was measured using the ODI, a 10-item questionnaire scored out of 50, with results expressed as a percentage. ODI scores between 21 and 40% are considered moderate disability, whereas scores below 20% indicate minimal disability [12]. To assess pelvic floor dysfunction and rule out underlying visceral, neurological, or localized pelvic causes, the PFDI-20 was utilized. This tool includes three subscales: The pelvic organ prolapse distress inventory-6, colorectal-anal distress inventory-8, and urinary distress inventory-6, each scored from 0 to 100, with a combined total score ranging from 0 to 300. Higher scores indicate greater symptom burden, whereas scores below 30 are generally considered minimal or asymptomatic [13]. In our case, the patient demonstrated significant clinical and functional improvement across all domains following intervention. The VAS improved from 10 to 2, the ODI score decreased from 22/50 (44%) to 7/50 (14%), indicating a shift from moderate to minimal disability and the PFDI-20 score reduced to 0, reflecting complete resolution of pelvic floor-related symptoms. The rehabilitation protocol focused on core and paraspinal strengthening, along with dedicated pelvic floor re-education. Similar to the findings of Johansson et al., who reported improved outcomes with sacral nerve-targeted physiotherapy, our patient benefited substantially from this integrated regimen [14]. Despite the encouraging short-term results, several limitations merit discussion. First, the diagnosis was based solely on clinical-radiological correlation without histopathological confirmation. No adjunctive investigations, such as CSF pressure studies, electromyography, nerve conduction studies or urodynamic tests were conducted to strengthen the evidence of sacral nerve dysfunction. Second, while validated tools such as ODI and PFDI were used, broader quality-of-life measures (e.g., 36-item short form survey, female sexual function index) were not employed, potentially underestimating patient-reported outcomes. Another limitation is the relatively short duration of follow-up, i.e., 6 months, beyond which the patient was lost to follow-up. As such, the long-term durability of the intervention and the risk of cyst recurrence remain uncertain. In addition, selection bias may have influenced outcomes, as the patient presented to a tertiary care setting after failing multiple prior therapies, possibly representing a more severe or refractory phenotype. Furthermore, the lack of a control group limits the ability to draw causal inferences regarding the specific efficacy of the steroid injection versus the concurrent therapies. However, the marked clinical response following the intervention, along with sustained functional gains, supports the potential utility of this minimally invasive strategy in selected cases of symptomatic Tarlov cysts.
This case underscores the importance of considering sacral Tarlov cysts as a rare but treatable neurogenic cause of vulvodynia, especially in patients with negative gynecological, dermatological and urological evaluations. MRI remains essential for diagnosis, given the cysts’ radiolucency on conventional imaging. A multidisciplinary, individualized approach combining image-guided steroid injection, physiotherapy and pharmacologic support can yield substantial symptom relief and functional improvement. While short-term outcomes were favorable, further studies with longer follow-up and comparative analyses are needed to validate the durability and efficacy of minimally invasive treatments for symptomatic Tarlov cysts.
This case underlines the importance of considering sacral Tarlov cysts in the differential diagnosis of chronic vulvar or perineal pain, especially when conventional workup is inconclusive. Image-guided minimally invasive intervention, combined with a structured rehabilitation program can offer safe and effective symptom control, reducing the need for invasive surgery.
References
- 1. Tarlov IM. Spinal perineurial and meningeal cysts. J Neurol Neurosurg Psychiatry 1970;33:833-43. [Google Scholar] [PubMed]
- 2. Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 1988;68:366-77. [Google Scholar] [PubMed]
- 3. Klepinowski T, Orbik W, Sagan L. Global incidence of spinal perineural Tarlov’s cysts and their morphological characteristics: A meta-analysis of 13,266 subjects. Surg Radiol Anat 2021;43:855-63. [Google Scholar] [PubMed]
- 4. Lucantoni C, Than KD, Wang AC, Valdivia-Valdivia JM, Maher CO, La Marca F, et al. Tarlov cysts: A controversial lesion of the sacral spine. Neurosurg Focus 2011;31:E14. [Google Scholar] [PubMed]
- 5. Hulens MA, Dankaerts W, Rasschaert R, Bruyninckx F, Willaert ML, Vereecke C, et al. Can patients with symptomatic Tarlov cysts be differentiated from patients with specific low back pain based on comprehensive history taking? Acta Neurochir (Wien) 2018;160:839-44. [Google Scholar] [PubMed]
- 6. Lim Y, Selbi W. Tarlov cyst. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. [Google Scholar] [PubMed]
- 7. Kim K, Chun SW, Chung SG. A case of symptomatic cervical perineural (Tarlov) cyst: Clinical manifestation and management. Skeletal Radiol 2012;41:97-101. [Google Scholar] [PubMed]
- 8. Murphy K, Oaklander AL, Elias G, Kathuria S, Long DM. Treatment of 213 patients with symptomatic Tarlov cysts by CT-guided percutaneous injection of fibrin sealant. AJNR Am J Neuroradiol 2016;37:373-9. [Google Scholar] [PubMed]
- 9. Freidenstein J, Aldrete JA, Ness T. Minimally invasive interventional therapy for Tarlov cysts causing symptoms of interstitial cystitis. Pain Physician 2012;15:141-6. [Google Scholar] [PubMed]
- 10. Hashemi S, Soltani H, Jabalameli M, Mirhoseyni SA, Soleymani B. Addition of triamcinolone or pethidine to epidural bupivacaine can-not improve postoperative pain relief in lumbar discectomy. Med J Islamic World Acad Sci 2011;19:131-6. [Google Scholar] [PubMed]
- 11. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008;31:165-9. [Google Scholar] [PubMed]
- 12. Mehra A, Baker D, Disney S, Pynsent PB. Oswestry disability index scoring made easy. Ann R Coll Surg Engl 2008;90:497-9. [Google Scholar] [PubMed]
- 13. De Arruda GT, de Andrade DF, Virtuoso JF. Internal structure and classification of pelvic floor dysfunction distress by PFDI-20 total score. J Patient Rep Outcomes 2022;6:51. [Google Scholar] [PubMed]
- 14. Johansson E, Danielsson L. Women’s experiences of physical therapy treatment for vulvodynia. Physiother Theory Pract 2024;40:2274-84. [Google Scholar] [PubMed]











