Safe surgical dislocation offers superior joint visualization and facilitates complete removal of loose bodies in hip primary synovial chondromatosis, making it a valuable alternative to arthroscopy—especially in cases with extensive intra-articular involvement.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai - 600077, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Introduction: Primary synovial chondromatosis (PSC) is a rare benign disorder characterized by cartilaginous nodule formation within synovial tissue. Hip joint involvement is uncommon, and optimal surgical management remains debated.
Case Report: We report a 27-year-old woman with a 2-year history of progressive right hip pain and functional limitation. Radiographic evaluation revealed multiple calcified loose bodies with mild joint space narrowing. The patient underwent safe surgical dislocation with complete loose body removal and partial synovectomy. Histopathological examination confirmed PSC. At 24 months, there is no evidence of early complications related to surgical dislocation, such as avascular necrosis, trochanteric osteotomy nonunion, and infection. We acknowledge that longer-term follow-up is necessary to exclude delayed recurrence or late complications such as heterotopic ossification which remains a limitation of our report.
Conclusion: Safe surgical dislocation provides excellent visualization and complete loose body removal in hip PSC while minimizing the risk of avascular necrosis. This technique represents a viable alternative to arthroscopic management, particularly for cases with large or numerous loose bodies.
Keywords: Primary synovial chondromatosis, hip joint, safe surgical dislocation, loose bodies, synovectomy
Primary synovial chondromatosis (PSC) is a rare benign metaplastic disorder characterized by the formation of cartilaginous and osteocartilaginous nodules within synovial tissue [1,2]. First described by Reichel in 1900, this condition is believed to result from metaplasia of pluripotential mesenchymal cells within the synovial membrane [2]. The disorder typically affects large joints, with the knee being most commonly involved, while hip involvement occurs in only 5–10% of cases [1,2]. The pathogenesis involves three distinct phases: an active intrasynovial phase without loose body formation, a transitional phase with both synovial lesions and loose bodies, and a quiescent phase characterized by free loose bodies without active synovial disease [2]. Clinical presentation is often nonspecific, leading to delayed diagnosis and potential complications including secondary osteoarthritis, joint contracture, and rarely, malignant transformation to chondrosarcoma [3]. Treatment typically involves surgical removal of loose bodies combined with synovectomy to prevent recurrence [3]. However, the optimal surgical approach for hip PSC remains controversial, with options including arthroscopic debridement, open arthrotomy, and safe surgical dislocation [4]. We present a case of hip PSC successfully treated using safe surgical dislocation and discuss the advantages of this approach.
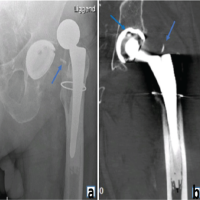
A 27-year-old previously healthy woman presented with a 2-year history of progressive right hip pain. The pain was described as deep, aching, and exacerbated by activity, with no history of antecedent trauma. Physical examination revealed a right coxalgic gait pattern with visible atrophy of the right thigh musculature. The range of motion assessment demonstrated preserved but painful movement in all planes, with particular limitation at terminal ranges. The patient reported functional impairment affecting daily activities and work performance. Plain radiographs of the right hip revealed multiple radiopaque loose bodies distributed throughout the hip joint space, with mild medial joint space narrowing and early osteophyte formation consistent with secondary degenerative changes (Fig. 1).

Figure 1: Multiple loose bodies in the right hip joint with narrowing of medial joint space.
Based on clinical presentation and imaging findings consistent with synovial chondromatosis, surgical intervention was undertaken using the Ganz safe surgical dislocation technique. This approach was selected to provide optimal visualization of the entire joint space while minimizing the risk of avascular necrosis of the femoral head. The procedure was performed through a posterior approach with trochanteric osteotomy, allowing controlled dislocation of the femoral head while preserving the medial femoral circumflex artery and its contributions to femoral head vascularity (Fig. 2a and b).
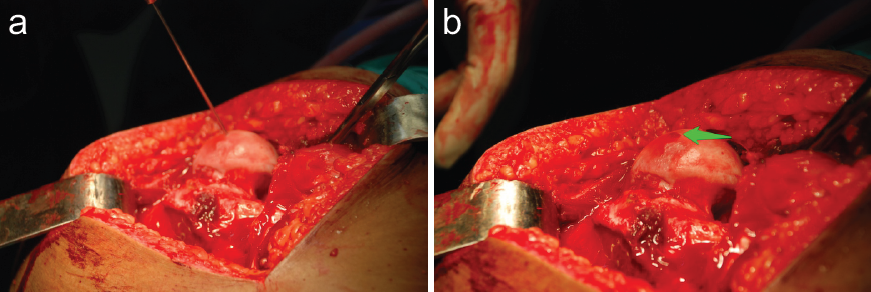
Figure 2: (a) Dislocated femoral head drilled with K-wire. (b) Vascularity of the femoral head confirmed through bleeding.
Ganz osteotomy preserves the external rotators (specifically obturator externus), which act as a protective sling around the medial circumflex femoral artery branch. Dislocation of the femoral head was done in a controlled, anterior direction (after posterior approach entry), so the posterior retinacular vessels remain untensioned and intact. The capsule was opened in Z-shaped fashion, avoiding transection of the retinacular vessels. Intraoperatively, 14 osteocartilaginous loose bodies ranging from 5.0 to 25 mm in diameter were identified and completely removed from the joint space (Fig. 3).

Figure 3: Osteocartilaginous loose bodies.
Following loose body removal, a partial synovectomy was performed, targeting areas of hypertrophic synovium while preserving healthy synovial tissue. Before reduction, femoral head vascularity was confirmed through drilling with a Kirschner wire, which demonstrated adequate bleeding, confirming preservation of vascular supply. Histopathological examination revealed nodular architecture typical of synovial chondromatosis (Fig. 4).
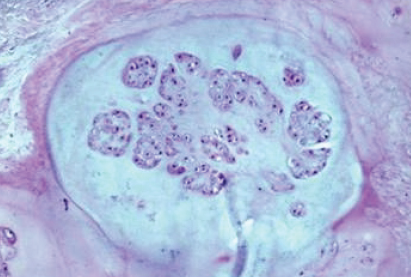
Figure 4: Histological picture with hematoxylin and eosin staining.
Each nodule consisted of hyaline cartilage with increased cellularity, clustered chondrocytes, and predominantly pyknotic nuclei. No mitotic figures were identified, confirming the benign nature of the lesion. The immediate posto-perative course was uncomplicated. The patient was mobilized with protected weight-bearing for 6 weeks, followed by progressive rehabilitation. At 3 months postoperatively, the patient had returned to full activities of daily living without pain or functional limitation. At 24-month follow-up, radiographic evaluation showed no evidence of femoral head avascular necrosis, disease recurrence, or progression of degenerative changes (Fig. 5). Clinical examination demonstrated full range of motion in all planes without pain or functional restriction (Fig. 6).
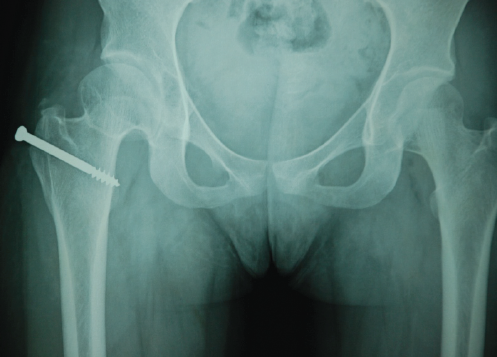
Figure 5: 24 months follow-up radiograph.

Figure 6: 24-month follow-up – knees cross-legged and squatting.
PSC of the hip represents a challenging clinical entity due to its rarity, nonspecific presentation, and potential for significant morbidity if left untreated [5]. This case demonstrates the effectiveness of safe surgical dislocation as a treatment modality for hip PSC with multiple large loose bodies. The pathogenesis of PSC involves metaplasia of synovial mesenchymal cells into chondroblasts, leading to the formation of cartilaginous nodules that may subsequently ossify and detach as loose bodies [2]. Recent molecular studies have identified the role of transforming growth factor-beta and fibroblast growth factor pathways in this process [6]. The presence of proliferating cell nuclear antigen-positive chondrocytes in primary PSC distinguishes it from secondary synovial chondromatosis associated with degenerative joint disease [7]. Hip involvement in PSC occurs in approximately 5–10% of cases, with a slight male predominance and peak incidence in the third to fifth decades [8]. The deep location of the hip joint often leads to delayed diagnosis, as early-stage disease may not be radiographically apparent until calcification or ossification occurs. The management of hip PSC requires complete removal of loose bodies and addressing the underlying synovial pathology to prevent recurrence. Recurrence rates of 0–15% have been reported in the literature, with incomplete synovectomy being a significant risk factor [9]. Arthroscopic management has gained popularity for hip PSC due to its minimally invasive nature and reduced morbidity [10]. However, hip arthroscopy has limitations including technical difficulty, restricted visualization of certain joint areas, and challenges in removing large loose bodies [10,11]. In addition, the learning curve for hip arthroscopy is steep, and complications such as neurovascular injury and cartilage damage have been reported [11]. The Ganz safe surgical dislocation technique offers several advantages for complex hip pathology, including PSC with multiple or large loose bodies [4,12,13]. This approach provides:
- Complete joint visualization: 360° access to all joint compartments
- Preservation of femoral head vascularity: Protection of the medial femoral circumflex artery
- Technical accessibility: Familiar surgical approach for most orthopedic surgeons
- Complete loose body removal: Ability to address all joint areas comprehensively
- Concurrent procedures: Opportunity for additional interventions if needed
The technique’s safety profile has been well-established, with avascular necrosis rates of <2% when performed by experienced surgeons [14,15]. While safe surgical dislocation offers excellent exposure and complete disease treatment, it is more invasive than arthroscopic approaches and requires trochanteric osteotomy with associated healing time and potential complications [16]. The decision between surgical approaches should consider factors including surgeon experience, loose body size and number, joint accessibility, and patient factors. Long-term follow-up is essential in PSC cases due to potential recurrence and rare malignant transformation risk (approximately 5%) [17]. Clinical deterioration, radiographic changes, or recurrent symptoms should prompt immediate evaluation and consideration of malignant transformation.
Safe surgical dislocation is a reliable treatment for PSC of the hip, especially in cases with multiple or large loose bodies. It offers comprehensive joint visualization, facilitates complete loose body removal, and enables partial synovectomy with minimal morbidity when performed by skilled surgeons. Compared to arthroscopy, this technique provides superior access to all joint compartments while preserving femoral head vascularity. Surgical approach selection should be tailored to individual patient factors and surgeon expertise. Given its safety and effectiveness, safe surgical dislocation merits consideration as a key option in the management strategy for hip synovial chondromatosis.
• Safe surgical dislocation enables complete visualization of the hip joint, facilitating thorough removal of loose bodies and targeted synovectomy in PSC.
• Preservation of femoral head vascularity through controlled dislocation techniques minimizes the risk of avascular necrosis, ensuring favorable post-operative outcomes.
• Early surgical intervention in hip PSC can prevent secondary degenerative changes, restore full function, and reduce recurrence risk when combined with partial synovectomy.
References
- 1. Iyengar KP, Mishra A, Vaish A, Kurisunkal V, Vaishya R, Botchu R. Primary synovial chondromatosis of the hip joint (PrSC of the hip): A retrospective cohort analysis and review of the literature. J Clin Orthop Trauma 2022;35:102068. [Google Scholar] [PubMed]
- 2. Habusta SF, Mabrouk A, Tuck JA. Synovial chondromatosis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. [Google Scholar] [PubMed]
- 3. Philip MC, Usman S: Synovial chondromatosis: A rare differential diagnosis of hip pain in a child. J Orthop Case Rep 2017;7:37-9. [Google Scholar] [PubMed]
- 4. Fang S, Li H, Wang Y, Xu P, Sun H, Li S, et al. Surgical hip dislocation for treatment of synovial chondromatosis of the hip. Int Orthop 2021;45:2819-24. [Google Scholar] [PubMed]
- 5. Marques-Gomes C, Fernandes BM, Diz-Lopes M, Bernardes M. Synovial chondromatosis, a cause of hip pain: A case report. J Med Case Rep 2024;18:594. [Google Scholar] [PubMed]
- 6. Li Y, El Mozen LA, Cai H, Fang W, Meng Q, Li L Transforming growth factor beta 3 involved in the pathogenesis of synovial chondromatosis of temporomandibular joint. Sci Rep 2015;5:8843. [Google Scholar] [PubMed]
- 7. Robinson D, Hasharoni A, Evron Z, Segal M, Nevo Z. Synovial chondromatosis: The possible role of FGF 9 and FGF receptor 3 in its pathology. Int J Exp Pathol 2000;81:183-9. [Google Scholar] [PubMed]
- 8. Adiga CP, Balaji GA, Prabhu V, Mahesh D. Primary synovial osteochondromatosis of hip joint in a teenager. Indian J Musculoskelet Radiol 2022;4:119-23. [Google Scholar] [PubMed]
- 9. Shamsunder C, Khalid SA, Sujit Kumar VR. Synovial chondromatosis of the hip – Management with synovectomy and partial removal of loose bodies: Case study. Muller J Med Sci Res 2014;5:64. [Google Scholar] [PubMed]
- 10. Lin CW, Wu CD. Primary synovial osteochondromatosis of the hip joint treated with arthroscopic-assisted mini-open surgery-two case reports. J Orthop Case Rep 2018;8:38-41. [Google Scholar] [PubMed]
- 11. You JS, Flores SE, Friedman JM, Lansdown DA, Zhang AL. The Learning curve for hip arthroscopic surgery: A prospective evaluation with 2-year outcomes in patients with femoroacetabular impingement. Orthop J Sports Med 2020;8:2325967120959140. [Google Scholar] [PubMed]
- 12. Habibi A, Konopka J, Arsoy D. EP6.33 surgical hip dislocation for synovial chondromatosis. J Hip Preserv Surg 2025;12:i100. [Google Scholar] [PubMed]
- 13. Parikh S, Hunter M, Heidemann E, Forro S, Davis T, Corces A. Surgical dislocation of the hip through lateral approach for the treatment of synovial chondromatosis. J Orthop Case Rep 2022;12:104-8. [Google Scholar] [PubMed]
- 14. Massè A, Aprato A, Alluto C, Favuto M, Ganz R. Surgical hip dislocation is a reliable approach for treatment of femoral head fractures. Clin Orthop 2015;473:3744-51. [Google Scholar] [PubMed]
- 15. Khalifa AA, Haridy MA, Fergany A. Safety and efficacy of surgical hip dislocation in managing femoral head fractures: A systematic review and meta-analysis. World J Orthop 2021;12:604-19. [Google Scholar] [PubMed]
- 16. Liu Y, Li J, Ma N, An M, Gao F, Hu B, et al. Arthroscopic treatment of synovial chondromatosis of hip joint. J Orthop Surg 2020;15:405. [Google Scholar] [PubMed]
- 17. Ng VY, Louie P, Punt S, Conrad EU. Malignant transformation of synovial chondromatosis: A systematic review. Open Orthop J 2017;11:517-24. [Google Scholar] [PubMed]