Management of delayed, self-inflicted metallic foreign body injuries demands surgical adaptability, infection control, staged reconstruction, and integrated psychiatric support for optimal recovery.
Dr. Department of Orthopedics, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Self-inflicted injuries in psychiatric patients are quite common; however, deep impaction of foreign bodies such as bolts is exceedingly rare. Foreign body impaction injuries in fingers pose a significant risk of skin and deep tissue damage, leading to infection and bone exposure if left unattended.
Case Report: A 20-year-old psychiatric male patient presented with severe pain, swelling, and restricted movement of index and ring fingers of his right hand following self-insertion of bolts into the fingers. Clinical examination and radiographic imaging revealed deeply embedded metallic bolts within the soft tissues of the affected fingers. Management involved careful removal of the impacted bolts through cutting, thorough debridement and subsequent reconstruction by local skin flaps to restore finger functionality and appearance.
Conclusion: This case emphasizes the importance of prompt diagnosis and management of foreign body injuries to prevent morbidity associated with deep tissue damage and bone erosion. It emphasizes the effectiveness of a combined approach of bolt excision, aggressive debridement, and skin flap reconstruction in treating such severe injuries. It offers broader clinical insights into managing severe foreign body injuries and enhances our understanding of the potential complications associated with delayed intervention in such cases.
Keywords: Self-inflicted injury, bolt impaction, flap reconstruction.
Self-inflicted trauma among psychiatric patients tends to present late. Such injuries are unusual in presentation and require innovative management. Insertion of metal bolts into the fingers is a very rare occurrence, having the potential for catastrophic vascular and soft-tissue damage if left treated on time [1]. In comparison to the management of accidental foreign body injury, intentional embedding is more challenging due to the delay in presentation, deep impaction contamination, and the psychological dimensions of the injury that affect management as well as recovery. Standard instrumentation frequently proves inadequate for the extrication of deeply embedded metal objects, requiring surgeons to improvise and use unconventional tools to avoid additional damage [2,3,4]. No less crucial is the stepwise sequence of reconstruction – the establishment of infection control and optimum tissues before definitive repair. The present case demonstrates not just the technical difficulties of bolt extrication by means of a commercially available cutlery blade but emphasizes the necessity for individualized reconstructive planning for salvaging hand anatomy and function. The case of a rare impaction of a bolt into the fingers of a young psychiatric patient was reported successfully being treated with emergency bolt division by a commercial-grade cutting blade followed by delayed flap reconstruction. The need for responsive operative methods and integrated multi-disciplinary management was thus brought about by this complex injury.
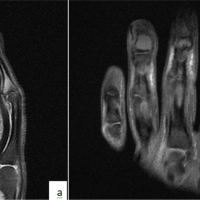
A 20-year-old male with a known psychiatric disorder was brought to the emergency department after self-inserting metallic bolts into his left hand’s index finger (IF) and ring finger (RF). The patient had reportedly absconded from home 8 days prior (Fig. 1a and b).

Figure 1: (a and b) Clinical photograph at presentation showing deep impaction of metallic bolts encircling the index and ring fingers, with evident soft-tissue necrosis, edema, and early signs of infection without gangrenous changes.
On examination, the bolts were deeply impacted in the fingers, with surrounding edema, erythema, soft-tissue involvement, and signs of early localized infection. The patient was febrile but hemodynamically stable. Radiographs confirmed a deeply embedded metallic bolt traversing the soft tissues without obvious bony involvement (Fig. 2).

Figure 2: Plain radiographs of the left hand (anteroposterior, oblique, and lateral views) showing metallic bolt-like foreign bodies tightly encircling proximal phalanges of index and ring fingers.
Given the chronicity and severity of the injury, emergency surgery was scheduled. Standard instruments were inadequate for bolt removal due to the hardness and position of the bolts. A heavy metal cutter brought from the engineering department (Fig. 3) was used carefully to section the bolts, avoiding further soft-tissue injury.

Figure 3: Intraoperative image showing use of commercial-grade metal cutter to divide deeply impacted bolt in patient’s fingers.
The debridement was done thoroughly along with lavage. Both fingers were viable with delayed bleeding on the IF, and due to contamination and local tissue inflammation, the closure was postponed (Fig. 4).
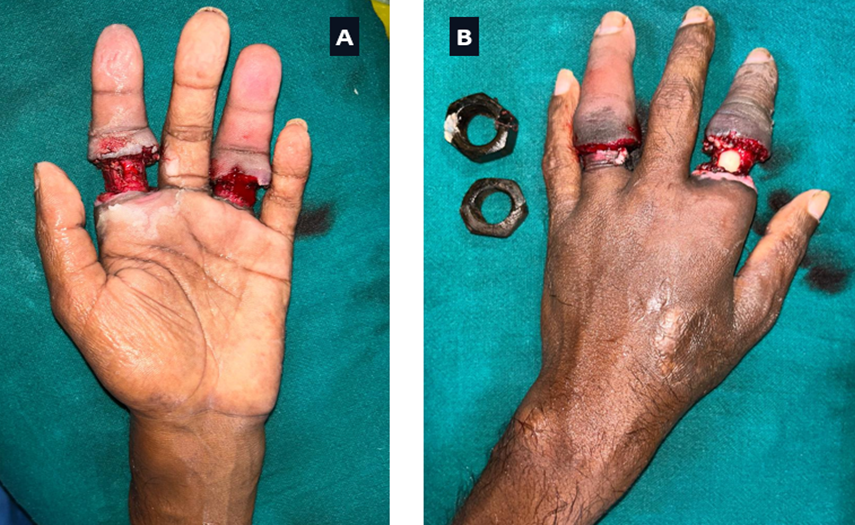
Figure 4: (a and b) Intraoperative image showing the patient’s hand immediately after removal of deeply impacted bolts from second and index fingers, revealing extensive soft-tissue damage, bone exposure, and early ischemic changes.
The wound was dressed and treated empirically with antibiotics. The patient had a history of self-insertion of rings over fingers and the penis in the past, which was removed at home. A psychiatric consultation was taken. Following admission, the patient was closely monitored in the ward to ensure his safety and to prevent any attempts to self-harm or leave the hospital premises. After ensuring infection control and optimizing the wound, delayed reconstruction was undertaken 2 weeks later on confirmation of both fingers’ viability (Fig. 5).

Figure 5: Wound status post bolt removal day 3.
The exposed bone over the dorsum of IF was covered with a reverse dorsal metacarpal artery flap, and the volar aspect was resurfaced with a cross-finger flap from the dorsum of the middle finger. Circumferential soft-tissue defect over RF was covered with 2 mm acellular dermal matrix and skin graft (Fig. 6).
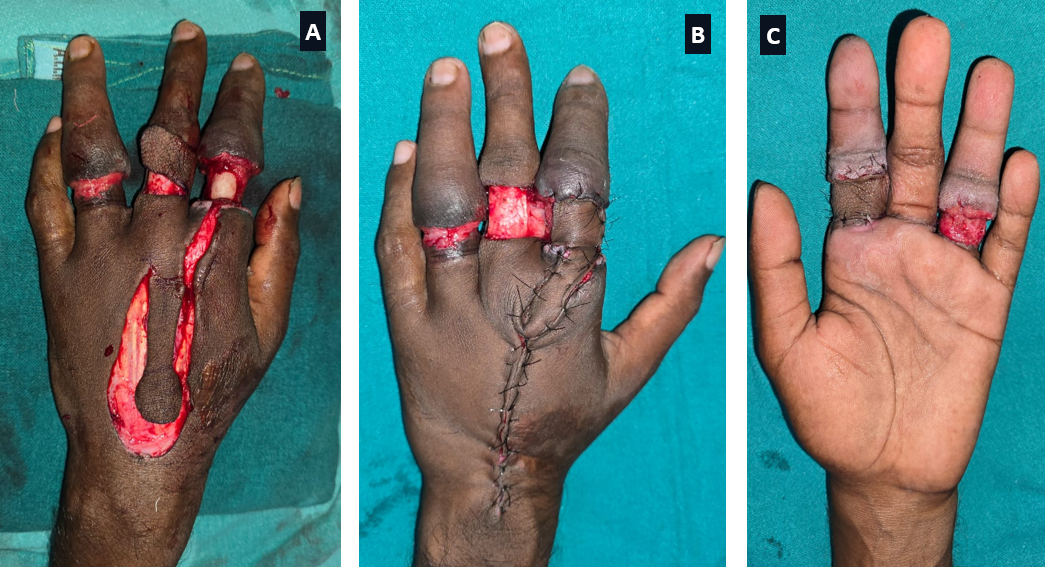
Figure 6: (a, b, c) Intraoperative image showing delayed flap reconstruction over the exposed second and 4th digits.
Recovery was uncomplicated after the operation, with good viability of the flap and uptake of skin graft. The cross-finger flap was divided after 2 weeks, and physiotherapy started. Tendon reconstruction was planned for both fingers after the joints were supple. Psychiatric follow-up was advised, but the patient was lost to subsequent follow-up despite repeated calls. The patient again absconded from home and was brought in by family members after 5 months. At presentation, the flap and skin graft were well settled over IF and RF (Fig. 7a, b, c, d).
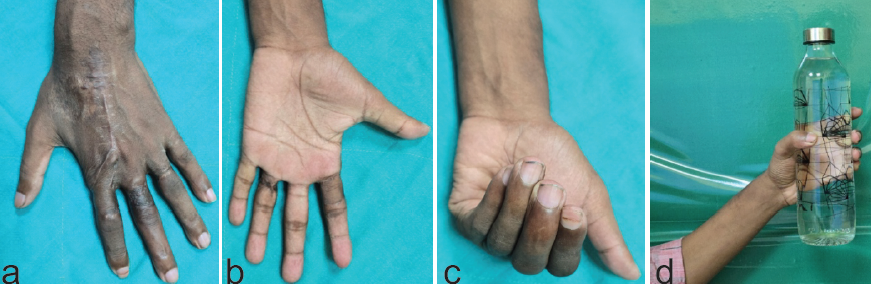
Figure 7: (a, b, c, d) At 5 months follow-up. Well-settled flap and skin graft. Stiffness of the interphalangeal joints of all four fingers, sparing the thumb. He can perform basic activities of daily living.
There was stiffness of the interphalangeal joints of IF, middle, RF, and little fingers, sparing the thumb. He can do basic activities of daily living. Parents were keeping him locked in the home to prevent wandering. Parents were advised regarding the need for physiotherapy for further procedures. The patient has not reported since then.
Self-inflicted injuries involving foreign bodies are relatively rare occurrences, and even more uncommon when involving industrial bolts in fingers. Psychiatric disorders predispose individuals to unusual patterns of self-harm, often resulting in complex and delayed presentation. Although various foreign body injuries of the hand have been documented, the impaction of bolts specifically has been scarcely reported [1,2]. Psychiatric illnesses such as bipolar disorder, schizophrenia, and major depressive disorder are strong predictors of self-mutilating acts [3]. In the index case, bolts were deeply embedded in the fingers for a long time resulting in soft-tissue necrosis and exposure of the bone. Prolonged retention of foreign bodies significantly increases the risk of secondary infection, chronic osteomyelitis, neurovascular compromise, and functional loss [ 5]. Ramesh and Satish Kumar reported a case of distal gangrene of finger in a crushed hand due to the “tourniquet effect” by the retained “engagement ring” [1]. Diagnosis in such settings is often delayed due to poor mental condition of the patient and ignorance of the relatives highlighting the indispensable role of early presentation. Surgical intervention in such cases requires cautious and decisive approach. Removal of the foreign body under strict control is imperative to prevent damage to the overlying structures. Echem et al., employed a traction technique for the removal of entrapped rings. The finger is adequately lubricated with petroleum jelly, and traction is consistently exerted toward the distal end of the finger using looped electric cables, while the cables are maneuvered laterally around the finger. The looped cables apply pressure to the soft tissues, causing the entrapped ring to roll off the cables and out of the finger [2]. Several additional non-destructive techniques, such as winding, compression, caterpillar, twin threads, and glove techniques, are documented in the literature [3,4,6]. When there is extensive loss of soft tissue, reconstruction by flap covering becomes mandatory to cover the exposed joints, tendons, and bones. In instances where significant soft-tissue loss is present, reconstruction with flap coverage becomes necessary to protect exposed tendons, joints, and bones. Several reconstructive options are described in the literature, including cross-finger flaps, thenar flaps, and reverse-flow digital artery flaps, each chosen based on defect location, size, and patient factors [7,8]. Flap reconstruction not only provides vital coverage but also optimizes functional and esthetic outcomes. A multi-disciplinary treatment plan combining psychiatric evaluation and treatment is required for complete management. Treatment of the underlying psychiatric disease minimizes the recurrence of self-mutilation and facilitates patients’ compliance with follow-up rehabilitation [9]. Early psychiatric intervention is a key factor of the overall prognosis of these patients. The outcome of cases of deep foreign body impaction depends mainly on the timely intervention, adequate soft-tissue reconstruction, and rigorous infection control. Early surgery supplemented by specific reconstructive measures greatly enhances the recovery of function and minimizes long-term morbidity [10]. The present case demonstrates a rare type of self-imposed injury and underscores the necessity of early surgery and psychiatric counseling. It adds to the scarce literature on injuries due to bolts as a foreign body and underlines the importance of a comprehensive treatment plan.
Impacted bolts of psychiatric patient fingers are a rare and severe type of self-mutilating injury that tends to be complicated by delay of presentation and deep tissue injury. Early removal and surgical debridement with subsequent staged reconstruction will achieve the best functional and esthetic results.
Deep impaction of metal foreign bodies within the hand is a particularly challenging problem surgically and functionally and particularly for psychiatric patients. The delay in presentation makes these cases more likely for infection, tissue necrosis, and osseous involvement. Prompt surgery and early diagnosis are essential to prevent long-term morbidity as well as maintain hand function. Ideal treatment involves a team effort including careful removal, precise surgery, and timely reconstruction. The coordinated care improves the function significantly and reduces the complications.
References
- 1. Ramesh BA, Satish Kumar J. Ring finger necrosis due to a ring. Indian J Surg 2017;79:367-8. [Google Scholar] [PubMed]
- 2. Echem RC, Eyimina PD, Adiela VV. Removal of entrapped rings from swollen fingers by a nondestructive technique. Int J Res Med Sci 2019;7:3162-7. [Google Scholar] [PubMed]
- 3. Kalkan A, Kose O, Tas M, Meric G. Review of techniques for the removal of trapped rings on fingers with a proposed new algorithm. Am J Emerg Med 2013;31:1605-11. [Google Scholar] [PubMed]
- 4. Thilagarajah M. An improved method of ring removal. J Hand Surg Br. 1999 Feb;24(1):118-9. [Google Scholar] [PubMed]
- 5. Moellhoff N, Throner V, Frank K, Benne A, Coenen M, Giunta RE, et al. Epidemiology of hand injuries that presented to a tertiary care facility in Germany: A study including 435 patients. Arch Orthop Trauma Surg 2023;143:1715-24. [Google Scholar] [PubMed]
- 6. Kingston D, Bopf D, Dhanjee U, McLean A. Evaluation of a two rubber band technique for finger ring removal. Ann R Coll Surg Engl. 2016 May;98(5):300-2. [Google Scholar] [PubMed]
- 7. Krishnamoorthy R, Karthikeyan G. Degloving injuries of the hand. Indian J Plast Surg 2011;44:227-36. [Google Scholar] [PubMed]
- 8. Alawi SA, Werner D, Könneker S, Vogt PM, Jokuszies A. Quality of life and reconstructive surgery efforts in severe hand injuries. Innov Surg Sci 2018;3:147-56. [Google Scholar] [PubMed]
- 9. Haw C, Hawton K, Houston K, Townsend E. Psychiatric and personality disorders in deliberate self-harm patients. Br J Psychiatry 2001;178:48-54. [Google Scholar] [PubMed]
- 10. Singisetti K, Kokkinakis M, Shankar N. Penetrating injury of the hand with a door handle: A case report. J Med Case Rep 2008;2:377. [Google Scholar] [PubMed]