CT imaging demonstrates superior accuracy in fracture characterization and pre-operative planning compared to conventional radiography, thereby contributing to improved surgical precision and functional outcomes in tibial fractures.
Dr. Rahul Vithal Ravariya, Department of Orthopaedics, Maharashtra Institute of Medical Education and Research Medical College, Pune, Maharashtra, India. E-mail: rahulravariya5@gmail.com
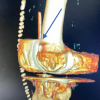
Introduction: Tibial plateau fractures are complex intra-articular injuries that require precise classification for optimal management. The widely used Schatzker classification, based on X-rays, provides a two-dimensional assessment, while the computed tomography (CT)-based three-column theory offers a more detailed three-dimensional analysis. This study aimed to compare the functional outcomes of complex tibial plateau fractures classified using these two systems and treated with locking compression plates (LCP).
Materials and Methods: A prospective, observational study was conducted involving 44 patients with closed Schatzker type V and VI tibial plateau fractures. Patients were allocated into two groups: Group A (n = 22) based on CT-based three-column classification and Group B (n = 22) based on X-ray-based Schatzker classification. All patients underwent open reduction and internal fixation using anatomical LCPs. Functional outcomes were assessed using the Rasmussen clinical score at regular follow-ups. Intraoperative variables and post-operative complications were also analyzed.
Results: Group A showed significantly better Rasmussen scores at 6, 12, 24, and 36 weeks (P < 0.05), along with shorter operative time, reduced blood loss, lower radiation exposure, and fewer complications compared to Group B. Joint stiffness and post-traumatic arthritis were notably higher in the Schatzker group.
Conclusion: CT-based three-column classification enables more accurate surgical planning and leads to superior functional and perioperative outcomes in complex tibial plateau fractures compared to the Schatzker classification.
Keywords: Classification, computed tomography, locking plate, Schatzker, tibial plateau fracture.
The tibial plateau, which constitutes the superior articular surface of the tibia, serves as a critical load-bearing region of the knee joint [1]. Patients with osteopenic bone have a higher component of compression with a less obvious split fragment, while young patients with good bone quality tend to have split fractures with less depression [2]. They account for 1.2% of all fractures in the body [3]. Tibial plateau fractures represent the fractures involving the articular surface of the proximal part of the tibia bone, i.e., the lateral or medial condyle or both, with a varying degree of articular depression and displacement [4]. They are prevalent in two age groups, and they manifest as higher-energy fractures in young patients and lower-energy fractures in elderly patients. Osteopenia is the main cause in the elderly. In younger individuals, tibial plateau fractures are more frequently linked to complications such as nonunion, infection, restricted joint mobility, and the development of post-traumatic arthritis [5]. These fractures typically result from axial loading combined with significant valgus or varus stresses [6]. The complexity of these injuries is further heightened by the intricate biomechanics of weight transmission across the knee joint, along with the critical role of ligamentous support and articular congruity in maintaining joint stability [7,8]. The majority of tibial plateau fractures result from falls from heights and road traffic accidents (RTAs) involving fast-moving vehicles. The fracture pattern, location, and degree of fracture displacement are determined by the direction, amplitude, and location of the force in addition to the position of the knee at impact [9]. The Schatzker classification is fundamental and essential to the term of tibia plateau fractures. It provides a description of fracture pathoanatomy in anterior–posterior radiographs and suggests treatment modalities. The Schatzker classification system for tibial plateau fractures, which divides fractures into six types, is widely recognized by orthopedic surgeons to assess initial injury, plan management, and predict a prognosis. Schatzker type IV, V, and VI fractures typically result from high-energy trauma and are frequently associated with both local and systemic injuries [10]. High-energy trauma resulting in extensive articular and metaphyseal injury patterns, are characteristic of severe tibial plateau injuries [11]. Among these, types V and VI are considered particularly complex due to extensive articular and metaphyseal involvement. The use of locking plates for managing such complex tibial plateau fractures offers several biomechanical advantages. Locking plate fixation has significantly advanced the management of tibial plateau fractures by offering biomechanical benefits such as improved stability in osteoporotic bone, secure unicortical screw fixation in the periarticular region, and the capacity to span extensively comminuted metaphyseal-diaphyseal zones effectively [13,14]. For Schatzker type V and VI fractures, both unicondylar and bicondylar plating techniques – often combined with or without cannulated cancellous (CC) screws – are commonly employed to achieve stable fixation. Multiple fixed-angle locking mechanisms created by these plates improve the stability of proximal tibia fractures and support the articular surface. Minimally invasive medial plating, preserving soft tissues and periosteal blood supply, provides stable fixation [12]. This helps with early knee range of motion and few post-operative problems. The primary goal of this study will be to examine the functional results following the use of locking plates to treat these fractures after classifying them on the two different classification systems, in addition to the consequences, if any [15,16]. The biomechanical principle of proximal tibial locking compression plate (LCP) is based on external fixators and internal fixators because the angle-stable interface between the screws and the plate allows placement of the plate without any contact with the bone, which gives the advantage of preserving the periosteal blood supply along with bone perfusion. These treatment methods, depending on how the fracture pattern is classified in the literature, are all acceptable treatment modalities but have their own merits and demerits. Similarly, they all vary in the ultimate result and are often compared to each other, as the knowledge of the best possible treatment still remains debatable. The management of tibial plateau fracture has been controversial, and the main objectives of it are a stable, pain-free knee joint with a good functional range of motion, along with good radiological restoration of the tibial articular surface [19]. When it comes to the comparisons between the existing methodologies for treatment, there is a lacuna in literature. Meanwhile, in the existing medical literature, there is no solid consensus about the best approach to treat tibial plateau fractures, and there is limited evidence to prove its the ultimate and gold standard treatment modality. Many studies have been conducted around the globe, but very few provide satisfactory comparative evidence for its substantial treatment. While recent radiological advancements offer improved bony injury assessments, they come with cost constraints and limited accessibility in underdeveloped and developing countries. In contrast, simpler and cost-effective primary imaging modalities only provide an initial idea of the type of bony injury and lack detailed information. The computed tomography (CT)-based three-column classification system provides a comprehensive three-dimensional insight into fracture patterns, offering a much deeper understanding of the injury’s pattern. In contrast, the Schatzker classification is based on standard X-ray imaging and offers a simplified, two-dimensional interpretation of the fracture. Each classification system possesses unique advantages and limitations. Treatment given to the patients of complex tibial plateau fractures using the two classification systems will have different functional outcomes [18]. Therefore, a comparative evaluation of the two classification systems is warranted to determine their relative clinical effectiveness.
This prospective, single-center, observational comparative study was conducted in the department of orthopedics at a tertiary care teaching hospital, following approval from the institutional ethics committee. A total of 44 adult patients presenting with closed, complex tibial plateau fractures were included in this study. Patients were assigned into 2 groups of 22 each: Group A included those whose fractures were classified using CT-based three-column theory, while Group B included those classified by the conventional X-ray-based Schatzker classification. Inclusion criteria comprised patients aged 18 years and older with Schatzker Type V/VI or multi-column fractures treated with open reduction and internal fixation using anatomical LCPs within 2 weeks of injury. Exclusion criteria included patients above 65 years, those with open fractures (Gustilo-Anderson Type III and above), associated avulsion injuries or joint dislocations, isolated single-column fractures on CT, or those medically unfit for surgery. All eligible patients presenting during the study were enrolled consecutively and subsequently assigned to two groups. All surgeries were performed by a single senior orthopedic surgeon, assisted by the same team, following a predefined standardized operative protocol, with consistent perioperative management and post-operative rehabilitation, ensuring uniformity in surgical technique, minimizing surgeon-related variability, and standardizing care within this single-center study. All surgeries were performed under spinal or epidural anesthesia in the supine position with tourniquet control, using standard anterolateral, posteromedial, or dual incision approaches as dictated by the fracture pattern. Fixation was performed with anatomical LCPs and CC screws as necessary. Postoperatively, patients were immobilized with an above-knee slab for 3 weeks, followed by suture removal around post-operative day 14. Post-operative evaluation included X-rays and CT scans for all patients to assess reduction, alignment, and fixation adequacy. Rehabilitation included early quadriceps exercises, knee mobilization after 3 weeks, and progressive weight-bearing beginning after 6 weeks. Functional outcomes were assessed using the Rasmussen clinical score at 6, 12, 24, and 36 weeks postoperatively by a single trained evaluator to minimize subjectivity and ensure consistency. Additional parameters, including duration of surgery, estimated blood loss, fluoroscopy exposure time, incision size, and post-operative complications, were systematically documented. Statistical analysis was performed using the Statistical Package for the Social Sciences version 26.0. Continuous data were presented as mean ± standard deviation and compared using Student’s t-test, while categorical variables were analyzed using Chi-square or Fisher’s exact test, with a P < 0.05 considered statistically significant.
This prospective observational study included 44 patients diagnosed with complex tibial plateau fractures, categorized into two equal groups. Group A (n = 22) comprised patients classified using the CT-based three-column theory, whereas Group B (n = 22) included patients categorized based on the Schatzker classification using X-ray imaging.
There was no statistically significant difference in baseline demographics between the two groups. The mean age in Group A was 42.5 ± 10.2 years, and in Group B, it was 44.2 ± 9.7 years (P = 0.47). Both groups showed male predominance, and the majority of injuries were due to RTAs. The side distribution of fractures was also comparable (Table 1).

Table 1: Patient demographics and baseline characteristics
Notable variations in critical intraoperative parameters were identified between the two groups. Group A demonstrated shorter surgical duration, reduced intraoperative blood loss, less fluoroscopy time, and smaller incision lengths. These differences were statistically significant (P < 0.05) and reflect improved surgical efficiency when utilizing CT-based fracture mapping (Table 2).

Table 2: Intraoperative and surgical parameters
Functional outcomes assessed using the Rasmussen clinical score showed statistically superior results in Group A across all follow-up intervals. At the final follow-up (36 weeks), the mean score in the CT-based group was 27.1 ± 1.4, compared to 25.0 ± 2.0 in the Schatzker group (P = 0.001). Early functional gains were evident, likely reflecting superior joint alignment and more precise surgical planning enabled by CT-based assessment (Table 3).

Table 3: Functional outcome (Rasmussen’s score)
Post-operative complications were more prevalent in the X-ray-based group. Notably, joint stiffness and post-traumatic arthritis were more frequently observed in Group B. The CT-based group had only one case of wound infection (4.5%), while the Schatzker group had three cases (13.6%). These findings support the use of CT imaging for more precise fracture characterization, reducing intraoperative errors and complications (Table 4).

Table 4: Post-operative complications
The management of complex tibial plateau fractures remains a challenging endeavor for orthopedic surgeons due to the intricacy of the joint anatomy, variability of fracture patterns, and potential for long-term functional impairment. Accurate fracture classification plays a pivotal role in surgical planning and prognostication. This study aimed to compare the functional outcomes and complication profiles of fractures classified using CT-based three-column theory versus the conventional X-ray-based Schatzker classification, both treated operatively with LCPs.
Our findings demonstrate that patients in the CT-based three-column group (Group A) had significantly better functional outcomes at all follow-up intervals, as measured by the Rasmussen functional score. At 36 weeks, the mean score in Group A was 27.1 compared to 25.0 in Group B (P = 0.001). This improvement is likely attributable to more precise pre-operative understanding of fracture morphology using CT imaging, which enhances the surgeon’s ability to address posterior and central column involvement that may be underappreciated on plain radiographs [10,21].
Similar trends were observed by Zhu et al., who introduced the three-column theory and highlighted its enhanced reproducibility and accuracy in assessing complex fracture patterns [9]. Their CT-based approach allowed surgeons to tailor fixation techniques to individual fracture morphologies, especially when posterior fragments were involved, an area often missed with traditional Schatzker classification.
Intraoperative parameters in our study also favored the CT-based group, with significantly shorter surgical times, reduced intraoperative blood loss, and decreased fluoroscopy time. This aligns with the observations of Egol et al. and Higgins et al., who highlighted that utilizing CT-based fracture mapping enhances surgical efficiency and minimizes intraoperative complications [13,14]. Moreover, smaller incision lengths in Group A may correlate with a less invasive approach made possible by better spatial orientation during surgical planning.
Group A demonstrated a reduced incidence of post-operative complications. In particular, joint stiffness and post-traumatic arthritis were more prevalent in the Schatzker group. Aurich et al. similarly reported that residual articular incongruity, more common in conventional fixation approaches, predisposes patients to post-traumatic osteoarthritis and functional limitations [4]. These findings are further supported by Vadadoriya et al., who reported improved functional outcomes and reduced complication rates in patients treated with anatomically contoured LCPs for tibial plateau fractures [20]. The enhanced restoration of joint congruity in the CT-based group may have played a key role in the decreased complication rates noted in our study.
While our study affirms the clinical value of CT-based classification, it also highlights a practical limitation. Advanced imaging may not be universally available, particularly in resource-limited settings, where cost and accessibility can hinder its routine use. Nonetheless, the findings support its utility, especially for high-energy fractures (Schatzker Types V and VI), where treatment planning complexity justifies the additional imaging burden.
The Schatzker classification, though widely used and easy to apply, primarily offers a two-dimensional view of a three-dimensional problem. Several authors, including Musahl et al., have argued that such systems oversimplify the injury and fail to capture posterior and multiplanar involvement, which are critical for optimal fixation and functional restoration [17].
The exclusion criteria were applied because these injuries often require different surgical strategies and post-operative protocols, which may limit the generalizability of our findings to the broader trauma population.
It should be noted that confounding factors such as patient comorbidities, rehabilitation compliance, nutritional status, and socioeconomic background may also influence outcomes. This pilot study was specifically designed to evaluate the feasibility and potential benefits of CT-based versus X-ray classification in a resource-limited setting. While providing preliminary evidence of improved outcomes with CT, these results should be interpreted in the context of potential confounders.
Further large-scale, multicenter, randomized studies with long-term follow-up are needed to confirm these findings and comprehensively assess functional outcomes, complications, and cost-effectiveness more comprehensively.
Limitations
This study has a few limitations. The study was single-centered. The sample size was relatively small, though adequate for detecting significant differences. Long-term functional and radiological outcomes beyond 36 weeks were not evaluated, which may not capture long-term functional or radiological outcomes.
This prospective study demonstrates that the CT-based three-column classification offers superior guidance in the operative management of complex tibial plateau fractures compared to the conventional X-ray-based Schatzker classification. By providing a more comprehensive and three-dimensional understanding of fracture morphology – including posterior and multiplanar components – the three-column approach enables more accurate pre-operative planning, tailored fixation strategies, and improved intraoperative execution.
Patients classified and treated using the CT-based system experienced significantly better functional outcomes, shorter surgical durations, lower intraoperative blood loss, and fewer post-operative complications. These findings are particularly relevant for high-energy articular injuries such as Schatzker Type V and VI fractures.
Given these advantages, the three-column theory should be considered a valuable adjunct in modern orthopedic trauma practice, especially in centers with access to advanced imaging. Its integration into routine clinical protocols may contribute to more effective surgical care and improved long-term recovery for patients with complex tibial plateau fractures.
Routine use of CT imaging in complex tibial fractures enhances diagnostic accuracy and guides optimal surgical planning, ultimately improving patient functional recovery and clinical outcomes.
References
- 1. Roberts JM. Fractures of the condyles of the tibia. An anatomical and clinical end-result study of one hundred cases. J Bone Joint Surg 1968;50:1505-21. [Google Scholar] [PubMed]
- 2. Unnikrishnan J, Jacob PJ, Francis J. Functional outcome of tibial condyle fractures treated with open reduction and internal fixation with plate and screws. Kerala J Orthop 2013;26(2):98-106. [Google Scholar] [PubMed]
- 3. Cole P, Levy B, Schatzker J, Watson JT. Tibial plateau fractures. In: Browner B, Levine A, Jupiter J, Trafton P, Krettek C, editors. Skeletal Trauma: Basic Science, Management, and Reconstruction. Philadelphia, PA: Saunders Elsevier; 2009. p. 2201-87. [Google Scholar] [PubMed]
- 4. Aurich M, Koenig V, Hofmann G. Comminuted intraarticular fractures of the tibial plateau lead to posttraumatic osteoarthritis of the knee: Current treatment review. Asian J Surg 2018;41:99-105. [Google Scholar] [PubMed]
- 5. Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury 2006;37:475-84. [Google Scholar] [PubMed]
- 6. Agnew SG. Tibial plateau fractures. Oper Tech Orthop 1999;9:197-205. [Google Scholar] [PubMed]
- 7. Schatzker J. The Rationale of Operative Fracture Care. Vol. 3. New York: Springer; 2005. p. 447-69. [Google Scholar] [PubMed]
- 8. Marsh JL. Tibial plateau fractures. In: Rockwood and Green’s Fractures in Adults. Philadelphia, PA: Wolters Kluwer; 2015. p. 2303-67. [Google Scholar] [PubMed]
- 9. Zhu Y, Yang G, Luo CF, Smith WR, Hu CF, Gao H, et al. Computed tomography-based three-column classification in tibial plateau fractures: Introduction of its utility and assessment of its reproducibility. J Trauma Acute Care Surg 2012;73:731-7. [Google Scholar] [PubMed]
- 10. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: The toronto experience 1968-1975. Clin Orthop Relat Res 1979;138:94-104. [Google Scholar] [PubMed]
- 11. Watson JT. High-energy fractures of the tibial plateau. Orthop Clin North Am 1994;25:728-52. [Google Scholar] [PubMed]
- 12. Krettek C, Gerich T, Miclau T. A minimally invasive medial approach for proximal tibial fractures. Injury 2001;32 Suppl 1:SA4-13. [Google Scholar] [PubMed]
- 13. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma 2004;18:488-93. [Google Scholar] [PubMed]
- 14. Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: How does lateral locking plate fixation compare to dual plate fixation. J Orthop Trauma 2007;21:301-6. [Google Scholar] [PubMed]
- 15. Ricci WM, Rudzki JR, Borrelli J Jr. Treatment of complex proximal tibia fractures with the less invasive skeletal stabilization system. J Orthop Trauma 2004;18:521-7. [Google Scholar] [PubMed]
- 16. Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res 2005;439:207-14. [Google Scholar] [PubMed]
- 17. Musahl V, Tarkin I, Kobbe P, Tzioupis C, Siska PA, Pape HC. New trends and techniques in open reduction and internal fixation of fractures of the tibial plateau. J Bone Joint Surg Br 2009;91:426-33. [Google Scholar] [PubMed]
- 18. Arun KN, Madhuchandra P, Raju KP, Pawan Kumar KM, Nandish. Functional outcome of tibial plateau fractures treated with locking compression plates. Int J Orthop Rheumatol. 2018;4:14–17. [Google Scholar] [PubMed]
- 19. Liu YK, Zhou ZY, Liu F. New developments in treatments of tibial plateau fractures. Chin Med J (Engl) 2017;130:2635-8. [Google Scholar] [PubMed]
- 20. Vadadoriya K, Chatterjee R, Sarkar T, Mukherjee S, Sengupta A, Hashib G, et al. Study of functional outcome of tibial plateau fractures treated with anatomical contoured locking compression plate. Indian J Orthop Surg 2021;7:280-90. [Google Scholar] [PubMed]
- 21. Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium–2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 2007;21 10 Suppl:S1-133. [Google Scholar] [PubMed]