Volar locking plate fixation allows stable anatomical restoration of distal radius fractures, facilitating early wrist mobilization and excellent functional recovery with minimal complications. Precise reduction of palmar tilt and restoration of articular congruity are critical technical factors that directly influence postoperative outcomes.
Dr. Thivagar Murugesan, Department of Trauma and Orthopaedics, Royal Shrewsbury Hospital, Shrewsbury, United Kingdom. E-mail: thivagarthedon@gmail.com
Introduction: Most frequent injuries of the Upper limb are a distal radius fracture (DRF). If they aren’t handled well, they might cause problems for a long time. There are several techniques to treat this issue, but volar locking plate fixation has become increasingly prevalent since it may restore anatomical alignment, provide stable fixation, and allow for early movement. This study aimed to evaluate the functional and radiological results of distal end radius fractures treated with volar locking plate fixation.
Materials and Methods: In this prospective analytical investigation, 60 patients with DRFs, ranging in age from 18 to 80 years, were enrolled. Patients were treated with open reduction and internal fixation using volar locking devices. Functional results are evaluated using the Gartland and Werley Demerit Point System and goniometry. Radial length, radial inclination, palmar tilt, and articular step-off were employed to quantify radiological outcomes. Follow-up evaluations were conducted at 2, 4, and 6 weeks, in addition to 6 months. We used the Statistical Package for the Social Sciences version 20 to analyze the data and discovered that P < 0.05 was significant.
Results: Patients exhibited substantial improvement in wrist function across all planes of motion, with plantar flexion rising from 31.6° at 2 weeks to 67.8° at 6 months, and dorsiflexion from 31.7° to 66.4°. Supination and pronation also became a lot better, becoming close to normal levels after 6 months. The radiographic restoration was good, with a mean radial length of 8.8 mm, an inclination of 17.6°, and a palmar tilt of 8.9°. There were very few complications (6.7% arthritis, 6.7% malunion).
Discussion: Our results support previous research showing volar plating offers robust fixation, restores anatomical alignment, and facilitates early mobility. Correlation study revealed that palmar tilt and articular congruity substantially impacted functional recovery, emphasizing the need of meticulous surgical reduction.
Conclusion: Volar locking plate fixation is an effective treatment for DRFs, characterized by low complication rates and excellent functional and radiological outcomes.
Keywords: Distal radius fracture, volar locking plate, functional outcomes, radiological outcomes, Gartland and Werley score.
Distal radius fractures (DRF) are among the most prevalent bone injuries in orthopedic treatment, constituting a considerable percentage of fractures in both younger persons after high-energy trauma and older adults with osteoporosis [1]. The rising frequency of these fractures, together with their capacity to induce enduring impairment, makes them a focal point of significant clinical and scientific interest. In the past, therapeutic options for DRFs have included both conservative care with casting and surgical procedures that include external fixation, Kirschner wires, and dorsal plating [2,3]. However, the problems that come with these methods, such malunion, limited wrist function, and tendon problems, have led to the creation and use of better fixation methods [4].
Volar locking plate fixation has been a favored surgical choice due to its capacity to provide secure fixation, preserve anatomical reduction, and promote early mobility, all of which are essential for good functional recovery [5]. The biomechanical benefit of locking plate designs, especially in osteoporotic bone, guarantees sufficient stability even in cases of comminuted or intra-articular fractures. Numerous studies have shown positive results with this method, but there is still a lot of variation in the results that have been recorded. This is due to the kind of fracture, the patient’s age, the timing of the surgery, and the rehabilitation that follows [6,7].
It is hard to figure exactly how well someone is doing after repairing a DRF. It covers not just range of motion (ROM) and grip-strength, but also patient-reported measurements and radiographic parameters such “radial length, inclination, palmar tilt, and articular congruity” [8,9]. Linking functional recovery to radiological results offers further information on how well the surgery worked and how it will affect the wrist’s long-term performance [10]. Despite a substantial body of research, there are still gaps in comprehending the correlation between radiographic restoration and functional recovery, especially across heterogeneous patient groups with varying injury mechanisms and socioeconomic statuses [11,12].
This prospective research was conducted to assess both functional and radiological results in patients with distal-radius-fractures treated with volar locking plate fixation. The research seeks to provide an exhaustive comprehension of the efficacy of volar plating in reinstating wrist function and anatomical alignment by methodical analysis of ROM, radiographic characteristics, and standardized grading systems. The research also looks at the links between radiological measures and functional results, providing useful information to help doctors make decisions and improve patient care.
The Department of Orthopaedics at General Hospital in Jayanagar, Bengaluru, Karnataka, conducted analytical study from September 2019 to August 2021, after getting permission from the Institutional Ethics Committee. All patients supplied their written approval before being enrolled in the experiment. During the research, “privacy and secrecy were strictly maintained. Individuals aged 18–80 years with DRFs, including intra-articular or extra-articular, closed simple or comminuted fractures, and with or without concurrent ulnar styloid fractures, were included. Pathological fractures, intricate injuries, fractures affecting both the radius and ulna (except the ulnar styloid), patients lost to follow-up, pregnant women, or those declining participation were omitted. We used prevalence data from the past 5 years to figure out that we required at least 30 individuals. However, to make the study stronger, we ended up enrolling 60 patients.
At the time of admittance, a detailed medical history and physical exam were done to find out how the event occurred, how healthy the individual was generally, and if they had any other problems that may be linked to it. The local examination focused on deformity, edema, pain, and functional impairment. We looked for compartment syndrome by checking the radial artery pulsations, capillary refill, and changes in sensation. At initially, a plaster slab below the elbow was employed to hold the individual immobile, and oral medications and non-steroidal anti-inflammatory drugs were given to help with the pain. Radiographic assessment included anteroposterior and lateral projections of both the injured and intact sides. Fractures were classified according to the Frykman and AO systems, evaluating radial length, inclination, palmar tilt, and articular step-off. Patients had a pre-anesthetic evaluation and then received open reduction and internal fixation with an anatomical volar locking plate, performed under regional or general anaesthesia. The duration between the injury and the operation was 3–12 days.
After surgery, patients were immobilized below the elbow for 2 weeks, had their limb elevated, moved their fingers, shoulder, and elbow actively, and then went to structured physiotherapy. Functional assessment occurred at 2, 4, 6 weeks, and 6 months, using goniometric measurements of wrist ROM and grip strength evaluation by a dynamometer. After 6 months, the Gartland and Werley Demerit Point System was employed to look at the findings. This approach takes into consideration complications, residual deformity, subjective symptoms, and objective assessments. The information was loaded into Microsoft Excel and then looked at using the Statistical Package for the Social Sciences version 20.” The descriptive statistics included means, percentages, and standard deviations. We used repeated measures analysis of variance for group comparisons, considering a P ≤ 0.05 as statistically significant.
The current research examined the functional and radiological results subsequent to volar locking plate fixation for DRFs in a prospective cohort of 60 patients. Table 1 shows that most of the patients were between the ages of 20 and 30 (30%), followed by similar numbers in the 41–50 and 51–60 age groups (20% each).
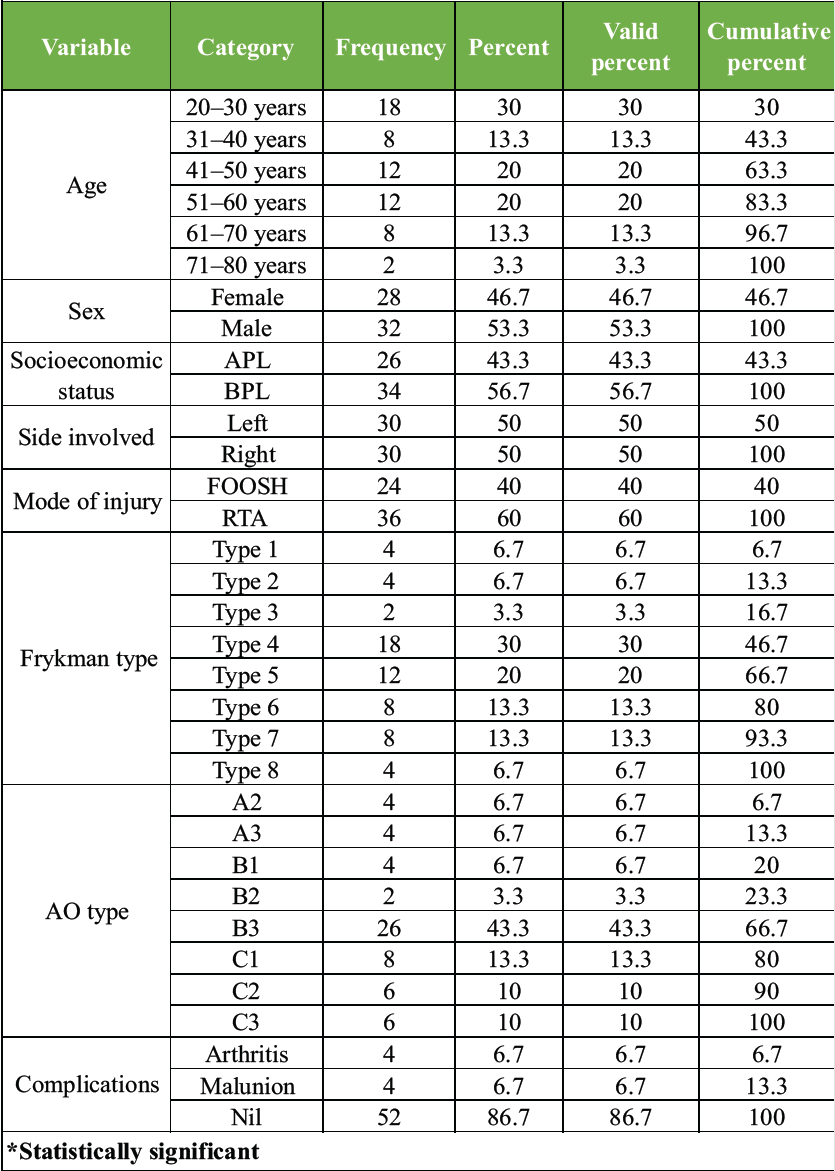
Table 1: Demographic and clinical characteristics of study population (n=60)
A minor number of patients were above 70 years old. There was a little difference between the sexes, with 53.3% being men and 46.7% being girls. Moreover, half of the patients (56.7%) were from families that lived below the poverty level. There was an equal distribution of involvement, with 50% of cases affecting the left and right wrists. Most of the injuries (60%) were caused by car accidents, while 40% were caused by falls on extended hands. In terms of fracture categorization, Frykman Type 4 (30%) was the most common, followed by Type 5 (20%). The AO categorization also showed that B3 fractures were the most common form (43.3%), followed by C1 (13.3%), and C2 and C3 were equal in number (10% each). Only 6.7% of people had arthritis, and 6.7% had malunion, which means that most (86.7%) did not have any problems.
Table 2 shows that functional outcomes measured by wrist ROM became better over time in all groups. The mean plantar flexion values went raised from 31.6° at 2 weeks to 67.8° at 6 months. There were statistically significant differences between the result groups (P < 0.05). Dorsiflexion exhibited a same pattern, enhancing from 31.7° at 2 weeks to 66.4° at 6 months, with significant intergroup differences (P < 0.05). Radial deviation improved from a mean of 8.7° at 2 weeks to 12.3° at 6 months, while ulnar deviation increased from 16.5° to 28.4° during the same time, both exhibiting considerable recovery. These data reveal that therapy continuously increased wrist mobility, and individuals in the good group consistently had wider ranges of motion.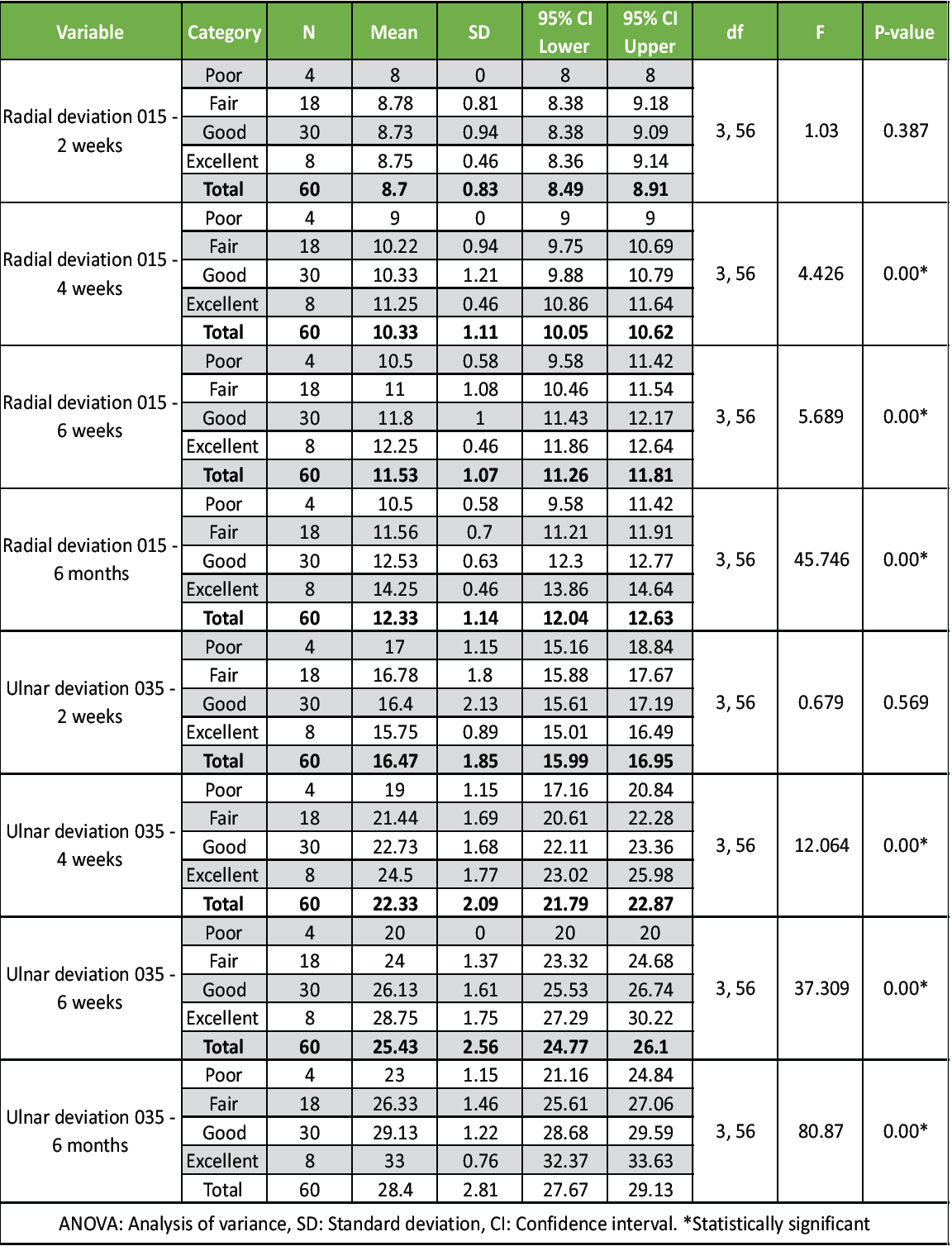
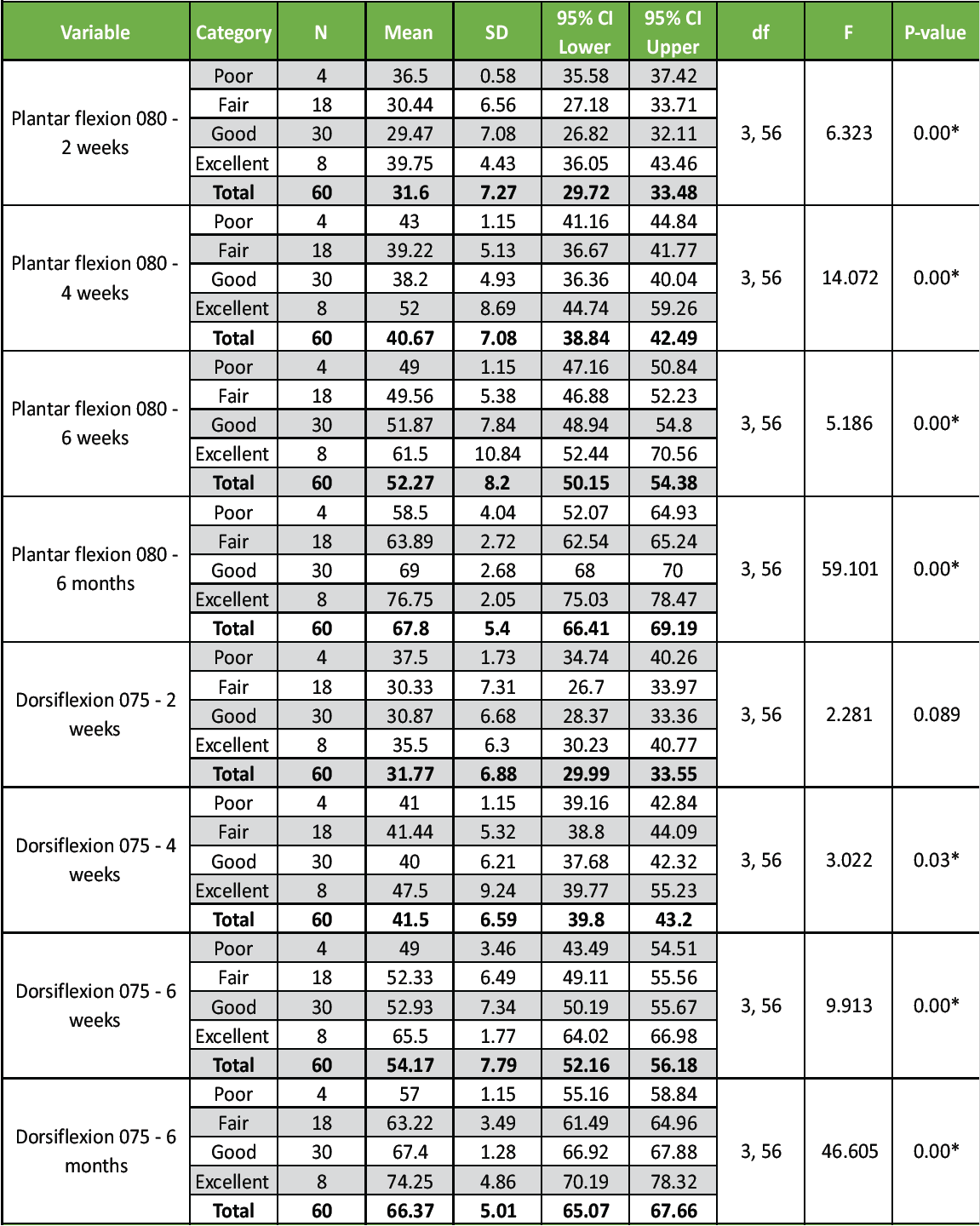
Table 2: Range of motion outcomes at different time intervals: Plantar flexion, dorsiflexion, and radial deviation measurements with ANOVA results
Table 3 shows more clearly what happened when the forearm was rotated. Supination rose considerably from 32.3° at 2 weeks to 72.1° at 6 months, and patients with favorable outcomes had almost full mobility (81°). Pronation increased from 47° at 2 weeks to 66.2° at 6 months, with significant P-values between groups once again. These results show that rotational recovery is similar to flexion–extension and deviation recovery, with significant gains seen 6 months after surgery.
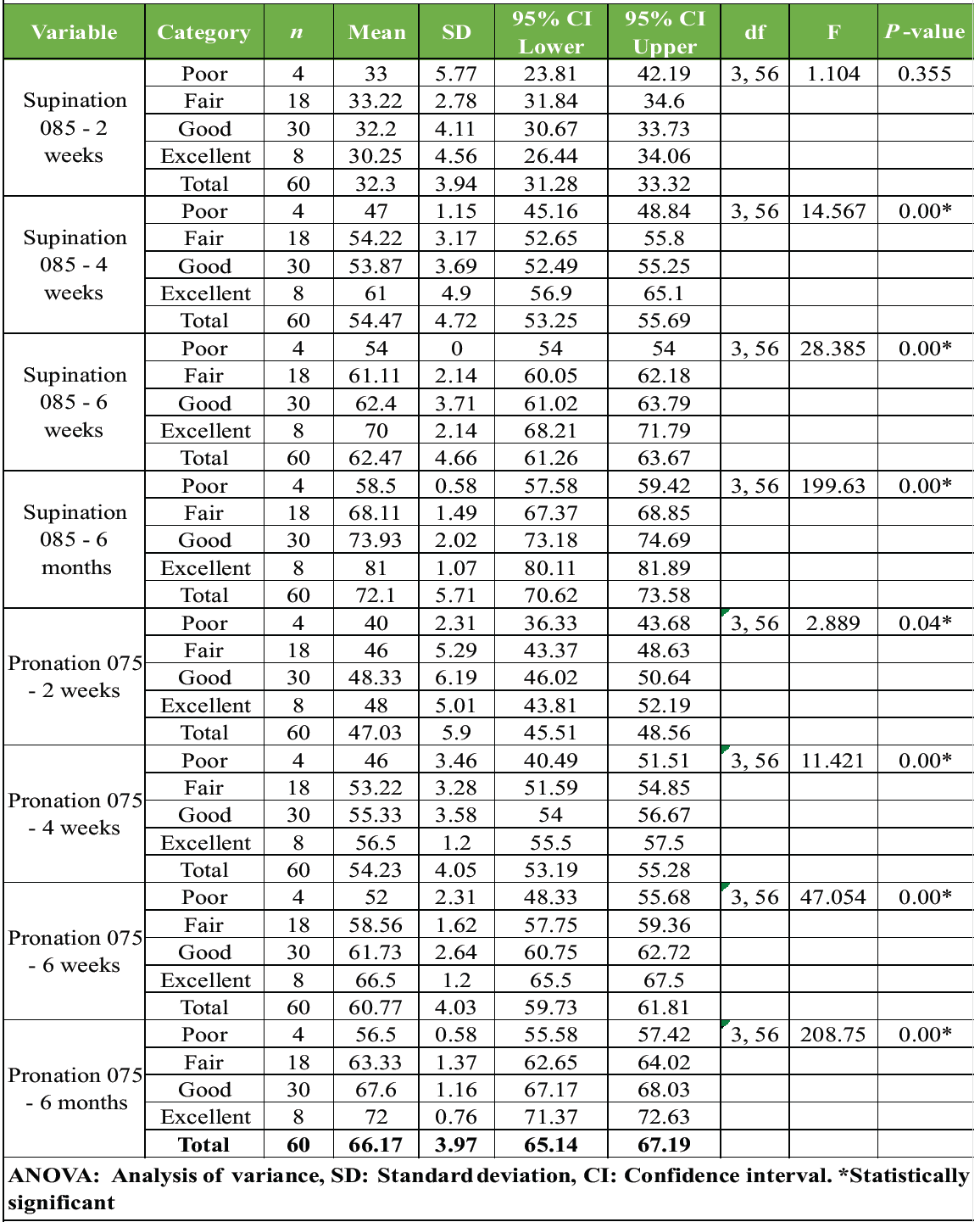
Table 3: Supination and pronation range of motion outcomes: descriptive statistics and ANOVA between-group comparisons
The alignment of the wrist was successfully restored, as evidenced by the radiological results in Table 4. “The average duration of time between injury and surgery was 4.2 days. Patients who demonstrated exceptional outcomes underwent surgery slightly sooner. The Gartland and Werley scores, which quantify functional recovery, exhibited a significant gradient. The average score of patients with exceptional outcomes was 1.5 points, while those with poor outcomes scored an average of 21.5 points. This discrepancy is statistically significant (P < 0.001). The groups all exhibited comparable radiographic characteristics, including radial length (mean 8.8 mm), radial inclination (17.6°), and palmar tilt (8.9°). Articular step-off exhibited some variation, with patients attaining exceptional outcomes averaging 1.5 mm, in contrast to lesser values in other groups. This difference was statistically significant (P = 0.008).
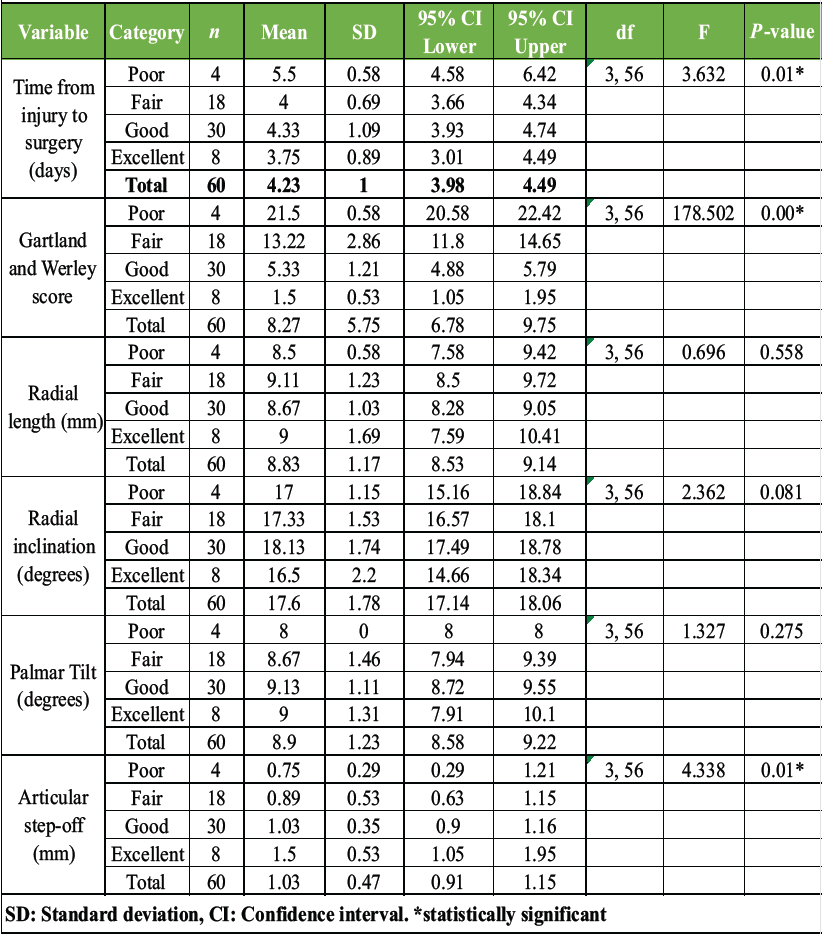
Table 4: Surgical parameters and radiological outcomes: time to surgery, functional scores, and radiographic measurements
Finally, Table 5 illustrates the investigation of the correlation between functional and radiological results. The Gartland and Werley scores exhibited a robust negative correlation with articular step-off (r = −0.368, P < 0.01) and palmar tilt (r = −0.283, P < 0.05). This implies that the functional recuperation was rendered worse by a decrease in tilt and an increase in step-off. Radial inclination and palmar tilt exhibited a positive correlation (r = 0.260, P < 0.05), while articular step-off and palmar tilt exhibited a negative correlation (r = −0.318, P < 0.05). To optimize functional outcomes, these findings emphasize the importance of achieving the appropriate anatomical reduction.”
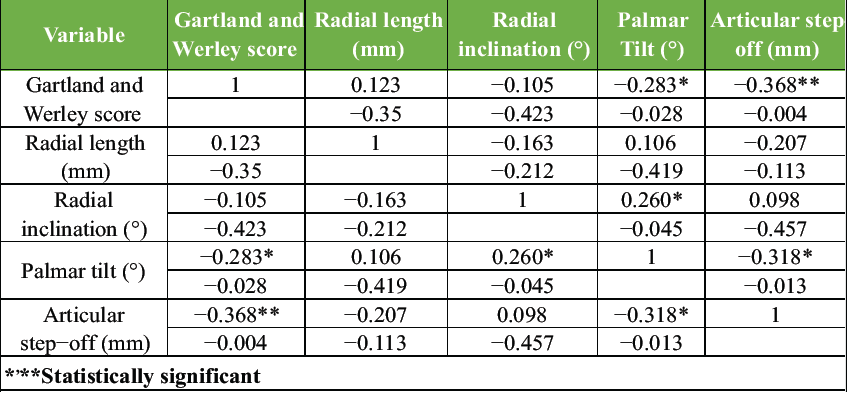
Table 5: Correlations between Gartland-Werley scores and radiological parameters
In general, the results indicate that volar-locking-plate fixation is a successful therapy for DRFs, as it results in a significant functional recovery, a progressive improvement in wrist and forearm mobility, and a stable radiological restoration with minimal complications.
The current prospective investigation contributes to the expanding data about the significance of volar locking plate fixation in the treatment of DRFs, including both functional and radiological perspectives. Our research showed that “wrist ROM, including flexion, extension, radial and ulnar deviation, pronation, and supination, improved steadily and significantly over time.” By 6 months, most patients had almost normal function again. Radiological results were similarly good, with the restoration of radial length, inclination, and palmar tilt. Only a small number of people had problems such as arthritis or malunion. These results are consistent with several published research, however, there are distinctions regarding long-term outcomes, complication rates, and the relationships between radiological alignment and functional recovery.
In contrast, Lawson et al. “performed a meta-analysis of randomized controlled trials and found no clinically significant differences in patient-reported outcomes between volar locking plates and conservative therapy at 12 months, despite volar plates demonstrating superior radiographic alignment. Our findings indicated that the restoration of parameters such as palmar tilt and articular step-off was significantly associated with enhanced functional scores, thereby underscoring the importance of precise anatomical reduction – an aspect that Lawson et al. recognized but did not observe as resulting in substantial variations in patient-reported pain or disability after 1 year. This difference may be attributed to the comparatively younger demographic in our research, where the restoration of normal architecture likely results in enhanced functional improvements compared to older patients” [13].
Likewise, Pace et al., “in their assessment of corrective osteotomy using volar locking plates for malunited DRFs, exhibited significant improvements in ROM, pain alleviation, and disabilities of the arm, shoulder, and hand (DASH) ratings. Their outcomes are similar to ours when it comes to functional recovery, although they were more focused on revision surgery for malunions than on acute fixation. Both investigations show that volar plates may efficiently restore biomechanics, which leads to better long-term wrist function” [14].
Huang et al. “emphasized difficulties associated with implants, namely flexor tendon discomfort resulting from plate prominence over the watershed line. In our research, complications were minor, with just 6.7% experiencing arthritis and malunion each. This indicates that precise plate location and attentive surgical technique are essential for reducing hardware-related issues. Their research emphasizes the significance of implant design and positioning, aligning with our finding that attaining appropriate anatomical reduction is a critical factor for optimal results” [15].
Lüdi et al. “documented favorable to exceptional results with the amalgamation of dorsal and volar plating in intricate intra-articular fractures, with patients recovering more than 90% of their contralateral wrist mobility and grip strength. Our investigation used just volar plates, although the recovery trajectories in ROM and function were comparable, indicating that for less intricate fractures, volar plating alone may be enough. Their results also stress that plating techniques need to be tailored to each fracture’s level of intricacy, with combination treatments only being used for very comminuted patterns” [16].
Gou et al. “conducted a comprehensive evaluation comparing volar locking plates with external fixation. They discovered that volar plates yielded lower DASH and visual analog scale ratings at follow-up and exhibited a reduced complication rate, whereas external fixation demonstrated superior early grip strength. Our investigation corroborates previous findings, demonstrating that volar plates facilitated stable fixation, prompt mobility, and superior functional recovery with few problems” [17].
When you look at all of these comparisons together, they show that our research supports the increasing agreement that volar locking plate fixation gives accurate radiological restoration and good functional recovery with minimal complication rates. Some research says that patient-reported outcomes might not always show big differences between conservative or external fixation methods. However, our results support the idea that accurate anatomical reduction with volar plates directly leads to better functional outcomes, especially in younger and more active groups. This establishes volar locking plate fixation as a reliable and efficacious method for the treatment of DRFs in well-chosen individuals.
The current prospective research revealed that volar-locking-plate fixation for DRFs guarantees exceptional functional recovery, continuous enhancement of wrist and forearm mobility, and dependable radiological restoration with low sequelae. Restoring anatomical features, especially palmar tilt and articular congruity, had a big effect on functional results, which shows how important it is to do a precise surgical reduction. Our results corroborate the effectiveness and safety of volar plating as a preferred treatment approach, providing stable fixation, early mobilization, and sustained recovery across various patient populations, in comparison to data from other research.
Volar locking plate fixation ensures stable anatomical reduction in distal radius fractures, allowing early mobilization and excellent functional recovery with minimal complications.
References
- 1. Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius frac-tures. Hand Clin 2021;28:113-25. [Google Scholar] [PubMed]
- 2. Diaz-Garcia RJ, Chung KC. The evolution of distal radius fracture management: A historical treatise. Hand Clin 2012;28:105-11. [Google Scholar] [PubMed]
- 3. Mathews AL, Chung KC. Management of complications of distal radius frac-tures. Hand Clin 2015;31:205-15. [Google Scholar] [PubMed]
- 4. Evans BT, Jupiter JB. Best approaches in distal radius fracture malunions. Curr Rev Musculoskelet Med 2019;12:198-203. [Google Scholar] [PubMed]
- 5. Ali Fazal M, Denis Mitchell C, Ashwood N. Volar locking plate: Age related outcomes and complications. J Clin Orthop Trauma 2020;11:642-5. [Google Scholar] [PubMed]
- 6. Parmaksizoglu F, Kilic S, Cetin O. A novel model of locking plate and locking spongious screw: A biomechanical in vitro comparison study with classical lock-ing plate. J Orthop Surg Res 2024;19:237. [Google Scholar] [PubMed]
- 7. Hollensteiner M, Sandriesser S, Bliven E, von Rüden C, Augat P. Biomechanics of osteoporotic fracture fixation. Curr Osteoporos Rep 2019;17:363-74. [Google Scholar] [PubMed]
- 8. Schmidt V, Gordon M, Petterson A, Buttazzoni C, Seimersson A, Sayed-Noor A, et al. Functional outcomes are restored a decade after a distal radius fracture: A prospective long-term follow-up study. J Hand Surg Eur Vol 2024;49:322-8. [Google Scholar] [PubMed]
- 9. Walter J, Prakrit Chhetri, D. Nandagopal. Radiological parameters and function-al outcomes in distal radius fractures: A narrative review. Natl J Clin Anat 2025;14:174-9. [Google Scholar] [PubMed]
- 10. Vinay V, Rastogi A, Mohta A, Mishra A. Correlation between functional and ra-diological assessment after treated distal radius fractures. J Orthop Rep 2025;15: 100752. [Google Scholar] [PubMed]
- 11. Ludvigsen T, Matre K, Vetti N, Kristoffersen PM, Toppe MK, Gudmundsdottir R, et al. Is there a correlation between functional results and radiographic find-ings in patients with distal radius fracture A0 type A3 treated with volar locking plate or external fixator? OTA Int 2021;4:e142. [Google Scholar] [PubMed]
- 12. Kumar BV, Rastogi A, Mohta A, Mishra A. Correlation between functional and radiological assessment after treated distal radius fractures. J Orthop Rep 2025;12: 100752. [Google Scholar] [PubMed]
- 13. Lawson A, Na M, Naylor JM, Lewin AM, Harris IA. Volar locking plate fixation versus closed reduction for distal radial fractures in adults: A systematic review and meta-analysis. JBJS Rev 2021;9: e20.00022. [Google Scholar] [PubMed]
- 14. Pace V, Sessa P, Guzzini M, Spoliti M, Carcangiu A, Criseo N, et al. Clinical, functional and radiological outcomes of the use of fixed angle volar locking plates in corrective distal radius osteotomy for fracture. Acta Biomed 2021;92:e2021180. [Google Scholar] [PubMed]
- 15. Huang YM, Chen CY, Lin KC, Tarng YW, Liao CY, Chang WN. Functional out-comes following fixation of a marginal distal radius fracture with two commonly used volar locking plates: A retrospective cohort study. BMC Musculoskelet Disord 2022;23:18. [Google Scholar] [PubMed]
- 16. Lüdi S, Kurz C, Deforth M, Ghafoor H, Haefeli M, Honigmann P. Radiological, clinical, and functional outcomes of combined dorsal and volar locking plate os-teosynthesis for complex distal radius fractures. J Hand Surg 2023;48:377-87. [Google Scholar] [PubMed]
- 17. Gou Q, Xiong X, Cao D, He Y, Li X. Volar locking plate versus external fixation for unstable distal radius fractures: A systematic review and meta-analysis based on randomized controlled trials. BMC Musculoskelet Disord 2021;22:433. [Google Scholar] [PubMed]