This case highlights that elastic stable intramedullary nailing can serve as a simple, minimally invasive, and effective alternative for selected humeral shaft fractures in adults.
Dr. Ghadeer A Alsager, Department of Orthopedic Surgery, King Saud Medical City, Riyadh, Saudi Arabia. E-mail: ghadeer.alsagr@gmail.com
Introduction: Humerus fractures can be caused by significant force, minor incidents, or pre-existing bone conditions. They have been historically managed with either conservative or surgical management. Recently, a shift toward surgical management can be seen due to the need for quicker functional recovery. A recent method has emerged back to the surface, and its outcomes are being reported more and more, which is the method of closed reduction and fixation using bundling techniques.
Case Report: We present a 68-year-old female who presented with an isolated closed left spiral humerus fracture at the junction of the proximal ⅔ and distal ⅓ following a fall. She was managed with three elastic nails of size 3 mm filling the medullary canal. She was followed closely postoperatively and healed without issues in range of motion, stiffness, or pain.
Conclusion: This case study examines the management of a humeral fracture in a geriatric patient using three free-floating elastic intramedullary nails. The successful outcome of this approach suggests that this treatment option offers adequate stability for humeral shaft fractures in older adults and can be easily implemented in similar fracture patterns.
Keywords: Humerus fractures, elastic nails, midshaft humerus fractures, closed reduction of humerus fractures, closed reduction.
Humerus fractures can be caused by significant force, minor incidents, or pre-existing bone conditions [1]. Approximately 60% of humeral shaft fractures (HSFs) are diagnosed in individuals older than 50 years [2]. HSFs can be managed conservatively or surgically with open reduction and plate osteosynthesis, minimally invasive plate osteosynthesis, or with intramedullary nails (IMN) [3]. Historically, non-surgical treatment has been favored for humerus fractures due to the bone’s natural healing ability, the less strict requirements for perfect bone alignment, and the avoidance of surgical risks [4]. Despite the traditional preference for non-surgical treatment, there is a recent shift toward surgical intervention for humerus shaft fractures. This change is driven by the desire for early mobilization, quicker functional recovery, and the development of new surgical techniques and implants. Plate and nail fixation are the most common surgical techniques used to achieve high healing rates, accurate bone alignment, and optimal upper limb function [5]. Intramedullary nailing is an alternative surgical technique for fixing humerus shaft fractures. Compared to open reduction and internal fixation with a plate, intramedullary nailing has a lower risk of infection and post-operative radial nerve injury. However, it carries a higher risk of shoulder impingement, pain, and limited shoulder motion, and may require subsequent surgery to remove the implant [6]. Originally intended for treating long bone fractures in children, Elastic stable IMN (ESINs) offer superior stability against axial, rotational, and bending forces in the diaphysis of long bones. Their lightweight design, coupled with the thicker periosteum and rapid bone healing in children, contributes to their effectiveness. However, despite these benefits, ESINs are rarely used in adult patients [7]. This case study examines the management of a humeral fracture in a geriatric patient using three free-floating ESINs. The successful outcome of this approach suggests that ESINs may offer adequate stability for HSFs in older adults. This case report details the use of a retrograde ESIN for a spiral humerus shaft fracture.
A 68-year-old right-hand dominant female presented after a fall with an isolated closed left spiral humerus fracture at the junction of the proximal ⅔ and distal ⅓ (Fig. 1).
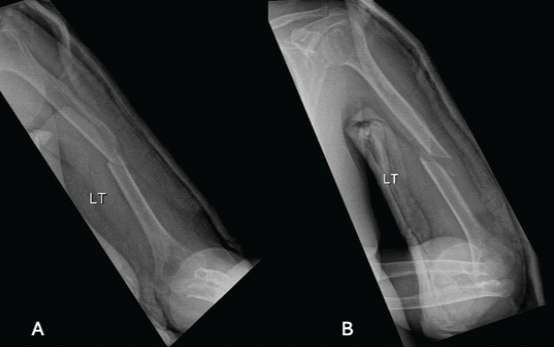
Figure 1: Humerus fracture upon presentation after coaptation splint application, (a) showing anterior-posterior view, (b) showing lateral view.
The patient had no other injuries and was neurovascularly intact on presentation. She was an independent ambulator. The patient was treated with a coaptation splint in the emergency room, with plans for operative fixation the next day. Following a pre-operative assessment, the patient was scheduled for closed reduction with internal fixation under general anesthesia. In the supine position, with a radiolucent arm table, without a tourniquet. Landmarks were identified, and a 3–5 cm incision was taken from the lateral epicondyle. The lateral cortex was perforated with an awl, and entry was established and confirmed under fluoroscopy in both anteroposterior (AP) and lateral views. An adequate nail was then fixed in a universal chuck with a T-handle and advanced with oscillating hand movements until it reached the fracture site. The nail was introduced into the proximal fragment by indirect manipulation of the fragment under fluoroscopy. Subsequent manual advancement of the nail was carefully done, passing the fracture site until finally resting at the humeral head. Same steps were taken to reach a total of 3 elastic nails of size 3 mm filling the medullary canal. Following closure, the patient was placed in a functional brace with a non-weight-bearing (NWB) status of the left upper extremity (Fig. 2).
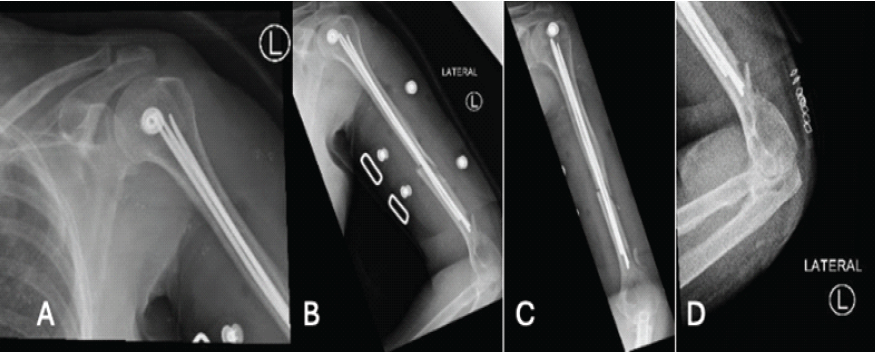
Figure 2: Humerus fracture post-fixation. (a) Anterior-posterior (AP) X-ray of the shoulder post-fixation, (b) lateral X-ray of the humerus post-fixation, (c) AP X-ray of the humerus post-fixation. (d) Lateral X-ray of the distal humerus post-fixation.
The patient had an uneventful post-operative course and was discharged on day 1 postoperatively after controlling pain and ensuring an intact neurovascular function with immediate range of motion exercises. The patient was in a splint for 2 weeks and then was seen in the office. The incision was well healed, and the patient remained neurovascularly intact. She was NWB for 6 weeks after surgery and advanced to progressive weight bearing as tolerated (Fig. 3).
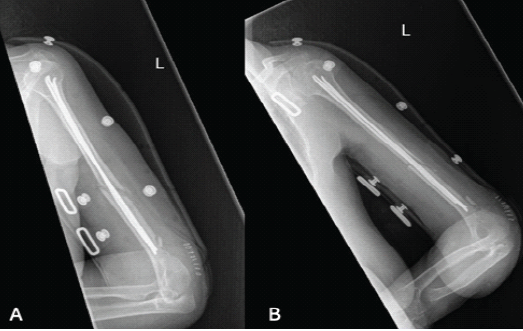
Figure 3: (a) Anterior-posterior X-ray of the humerus 2 weeks postoperatively, (b) Lateral X-ray of the humerus 2 weeks postoperatively.
The patient was then seen in the office at 3-months postoperatively and reported significant improvement in pain, her elbow range of motion was 0–135° (Fig. 4).
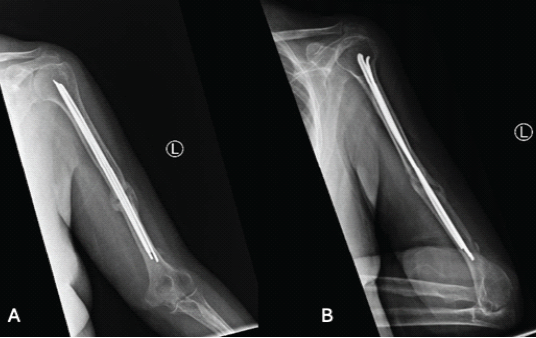
Figure 4: (a) Anterior-posterior AP X-ray of the humerus 3 months postoperatively, (b) Lateral X-ray of the humerus 3 months postoperatively.
At 6-months post-operative follow-up, the patient was pain free with full range of motion, and radiographs demonstrated appropriate callus formation (Fig. 5).
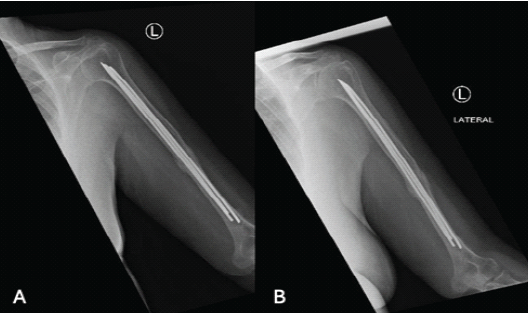
Figure 5: (a and b) show anterior-posterior X-ray of the humerus 6 months postoperatively.
The standard of care for humeral shaft fracture remains open reduction and fixation with plate osteosynthesis ORIF or closed reduction and fixation with rigid IMNs [8]. However, a recent method has emerged back to the surface, and its outcomes are being reported more and more, which is the method of closed reduction and fixation using bundling techniques [8,9]. This bundling technique is performed percutaneously with either elastic nails or long Kirschner wires (K-wires), aiming to stabilize the fracture by filling the canal [10]. The biomechanics behind Hackethal’s method of elastic nailing are dependent on two elastic nails that symmetrically brace within the metaphysis, where they produce three-point fixation on the inner bone, providing rotational, axial, and translational stability that is vital for the best results [11]. It is important to understand the correct technique for this method, as most of the complications reported are due to inadequate surgical technique. Proximally, the construct used whether the nail or K-wire should be diverged to increase its stability [10]. Distally, they should pass through both the pillars of the lower humerus to achieve three-point fixations, and they should be locked to prevent migration [10].
Concerns about potential fat embolism, harm to medullary circulation, and a widespread poor understanding of the biomechanical principles of intramedullary nailing have all contributed to the debate surrounding this therapeutic approach, which led to its abandonment [9]. A recent study re-investigating the biomechanics of this elastic nailing had shown that the optimal nail diameter for this method, which is recommended to be used, is between 2 and 3 mm, as they exhibited that torsional stiffness is highly dependent on nail diameter. This method has continued usefulness in treating simple shaft fractures; however, understanding of biomechanical principles is crucial [12].
The proposed indications for using this method from the literature are: Simple AO A and B diaphyseal fractures, adequate surgical technique (complete filling of the medullary cavity with the implants) [13], Narrow intramedullary canal (< 7 mm), long spiral or oblique fracture over the metadiaphyseal junction, obesity [7], Middle third of humerus shaft fracture [14], Nonetheless some authors have advised against the use of this method with oblique and spiral fracture as they tend to not unite [11].
On the other hand, this method should be avoided when the fracture is multifragmentary, not amenable to closed reduction, intra-articular, the bone is osteoporotic, the medullary canal is obstructed, there is radial nerve palsy, or an active infection at the surgical site [15].
Advantage of this method over ORIF is the fact that it is a closed method, thus will require minimal soft-tissue dissection, low chance of hematoma distribution and periosteal stripping, and less risk of nerve injury, and is superior to rigid IMN by sparing the rotator cuff [11,16]. It also has the advantage of having low cost, requiring no specific instrumentation, and being fast to carry out [10]. Outcomes reported in patients treated with this method were 0% fractures at the insertion point, normal shoulder and elbow function in 87% and 63% respectively, and Union was achieved in a 2-month period [10].
The downside of this method is the fact that it is a non-rigid construct, hence requires the addition of a cast or arm-to-chest bandage until union begins, non-union when applied to an incorrect fracture pattern or an incorrect surgical technique is implemented, which was reported to be 5–24%, migration of the K-wires (6–29%) [10].
Sidiropoulos et al. [15] published a case report reviewing the literature till the end of 2019, using the keywords “adult humerus fracture, elastic nails.” In patients 18 years or older with a humerus diaphyseal fracture. They reviewed the complication rate among seven studies (128 patients) included. Non-union was (7.1–23.3%), infections (10.0–30%), Nail impingement and elbow stiffness 6 months postoperatively (3.9%). The overall functional result was at least good in 83%(16).
Moreover, more recent studies published after 2019, investigating this method, Tarng et al. [7] 2021, analyzed 16 patients with a mean age of 54.4 years and a mean follow-up of 14 ± 2.5 months. They reported an average time to union to be 16 ± 4.3 weeks with 0% of wound infections, loss of reduction, non-union, implant failure, or skin irritation. The only complication reported was a nail back-out in an osteoporotic patient. Another study by Abdalla et al. [17]. In 2024 a 29 patients with a mean age of 32. Their result showed union in 19 fractures within 13–21 weeks. Evaluation using the Stewart and Hundley Scoring technique showed excellent outcomes for 60% of patients, good outcomes for 30%, fair outcomes for 5%, and poor outcomes for 5%.
Although ORIF and IMN are still considered the standard of care, we should keep our minds open to other techniques, such as the described method in this study. Given that the humerus has the advantage of being a non-weight-bearing bone, it has a wider range of acceptable alignment, and less invasive methods of fixation, such as the one mentioned, can be utilized effectively.
ESINs are a valid treatment option, particularly in elderly patients with simple fracture patterns and narrow medullary canals. By filling the canal with multiple flexible nails, adequate axial and rotational stability can be achieved while avoiding extensive soft tissue dissection, radial nerve injury, and shoulder impingement associated with plating or rigid nailing. Successful outcomes depend on proper patient selection, correct surgical technique ensuring three-point fixation, and careful post-operative monitoring. This case supports reconsidering ESIN as a viable fixation option for humeral shaft fractures, especially where biological preservation and early mobilization are priorities.
References
- 1. Lander ST, Mahmood B, Maceroli MA, Byrd J, Elfar JC, Ketz JP, et al. Mortality rates of humerus fractures in the elderly: Does surgical treatment matter? J Orthop Trauma 2019;33:361-5. [Google Scholar] [PubMed]
- 2. Bounds EJ, Frane N, Jajou L, Weishuhn LJ, Kok SJ. Humeral Shaft Fractures. Orthopedic Trauma Call for the Attending Surgeon; 2023. p. 121-30. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448074 [Last Accessed on 2025 May 09]. [Google Scholar] [PubMed]
- 3. Qiu H, Liu Y, Chen Y, Weng Z, Liu D, Dong J, et al. Treatment of humeral shaft fractures with different treatment methods: A network meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 2023;24:583. [Google Scholar] [PubMed]
- 4. Van Bergen SH, Mahabier KC, Van Lieshout EM, Van Der Torre T, Notenboom CA, Jawahier PA, et al. Humeral shaft fracture: Systematic review of non-operative and operative treatment. Arch Orthop Trauma Surg 2023;143:5035-54. [Google Scholar] [PubMed]
- 5. Li Y, Luo Y, Peng J, Fan J, Long XT. Clinical effect of operative vs nonoperative treatment on humeral shaft fractures: Systematic review and meta-analysis of clinical trials. World J Orthop 2024;15:783-95. [Google Scholar] [PubMed]
- 6. Orapiriyakul W, Apivatthakakul V, Theppariyapol B, Apivatthakakul T. Humerus shaft fractures, approaches and management. J Clin Orthop Trauma 2023;43:102230. [Google Scholar] [PubMed]
- 7. Tarng YW, Lin KC, Chen CF, Yang MY, Chien Y. The elastic stable intramedullary nails as an alternative treatment for adult humeral shaft fractures. J Chin Med Assoc 2021;84:644-9. [Google Scholar] [PubMed]
- 8. Obruba P, Kopp L, Edelmann K. Treatment of humeral shaft fractures using Hackethal’s technique of intramedullary bundle nailing. Acta Chir Orthop Traumatol Cech 2012;79:341-6. [Google Scholar] [PubMed]
- 9. Upadhyay AS, Lil NA. Use of titanium elastic nails in the adult diaphyseal humerus fractures. Malays Orthop J 2017;11:53-9. [Google Scholar] [PubMed]
- 10. Pidhorz L. Acute and chronic humeral shaft fractures in adults. Orthop Traumatol Surg Res 2015;101 Suppl 1:S41-9. [Google Scholar] [PubMed]
- 11. Verma A, Kushwaha SS, Khan YA, Mohammed F, Shekhar S, Goyal A. Clinical outcome of treatment of diaphyseal fractures of humerus treated by titanium elastic nails in adult age group. J Clin Diagn Res 2017;11:RC01-4. [Google Scholar] [PubMed]
- 12. Obruba P, Capek L, Henys P, Kopp L. Computed modeling of humeral mid-shaft fracture treated by bundle nailing. Comput Methods Biomech Biomed Engin 2016;19:1371-7. [Google Scholar] [PubMed]
- 13. Obruba P, Rammelt S, Kopp L, Edelmann K, Avenarius J. Non-Unions after fixation of humeral fractures using Hackethal’s bundle nailing technique. Acta Ortop Bras 2016;24:270-4. [Google Scholar] [PubMed]
- 14. Baranowski D, Brug E. Current indications for intramedullary bundle nailing. Unfallchirurg 1989;92:486-94. [Google Scholar] [PubMed]
- 15. Sidiropoulos K, Athanaselis ED, Saridis A, Agapidis A, Saridis A. Elastic intramedullary nails in the treatment of multi-segmental humeral fracture in a polytrauma patient. Cureus 2021;13:e16161. [Google Scholar] [PubMed]
- 16. Zhao JG, Wang J, Huang WJ, Zhang P. Surgical interventions for treating humeral shaft fractures in adults. Cochrane Database Syst Rev 2019;2019:CD012174. [Google Scholar] [PubMed]
- 17. Abdalla M, Elsagheir M, Ashry A, Elbannan M, Ragab A, Mohamad A. Is elastic stable intramedullary nailing a viable treatment option for diaphyseal fractures of the humerus in adults? A 29-case series prospective study. Ortop Traumatol Rehabil 2024;26:357-62. [Google Scholar] [PubMed]





