Surgeons should ensure secure fixation of REGENETEN® implants, as detachment may lead to loose body formation.
Dr. Akinari Tokiyoshi, Department of Orthopaedic Surgery, Hotakubo Orthipaedic Hospital, 5-7-27 Higashi Ku Kumamoto City, Kumamoto, 862-0926, Japan, Department of Orthopaedic Surgery, Kugawa Hospital for Orthopaedic Surgery, 10-26 Shindencho, Kofu City, Yamanashi, 400-0066, Japan. E-mail: akinaritokiyoshi@gmail.com
Introduction: The REGENETEN® bioinductive collagen implant (Smith and Nephew, Andover, MA) has been increasingly used in rotator cuff repair as a biological scaffold to promote tendon regeneration. Clinical studies have shown favorable healing and reduced retear rates, with complications considered rare. We present a rare case of loose body formation within the subacromial bursa following rotator cuff repair with REGENETEN®.
Case Report: A 60-year-old man presented with the right shoulder pain. Magnetic resonance imaging (MRI) revealed a partial-thickness tear of the supraspinatus tendon, and conservative treatment was initiated. Due to persistent nocturnal pain, arthroscopic repair was performed 3 months later using a medium-sized REGENETEN® implant secured on the tendon surface. Postoperatively, passive range-of-motion exercises began at 2 weeks, and active exercises at 3 weeks. At 6 weeks, the patient developed recurrent shoulder pain and mechanical catching. Despite continued rehabilitation, symptoms worsened. At 6 months, MRI demonstrated a hypointense structure within the subacromial bursa. Diagnostic arthroscopy revealed a whitish, mobile loose body measuring 16 × 13 mm, containing a medial implant staple encapsulated by fibrous tissue, while the repair site remained intact. The loose body was excised arthroscopically. Histological examination demonstrated fibrin deposition, infarcted necrotic fibrous tissue, and fibrocollagenous proliferation, findings consistent with a foreign body reaction. The post-operative course was uneventful, symptoms resolved within 1 month, and the patient returned to full occupational activity within 2 months.
Conclusion: Although REGENETEN® has been proven safe and effective, rare complications such as implant detachment and foreign body reactions should be considered. Unlike rice body formation, which is associated with systemic inflammatory conditions and necessitates evaluation for underlying rheumatologic disease, the present case represents an implant-derived loose body that was definitively treated by surgical excision. To the best of our knowledge, this is a rare case of loose body formation within the subacromial bursa due to migration of a REGENETEN® implant staple. Awareness of this complication is clinically important in patients with persistent post-operative mechanical symptoms following rotator cuff repair with REGENETEN®.
Keywords: Rotator cuff injuries/surgery, tendon injuries/surgery, collagen/therapeutic use, foreign-body reaction, shoulder joint/surgery.
The REGENETEN® bioinductive collagen implant (Smith and Nephew, Andover, MA) has been increasingly utilized as a biological scaffold in rotator cuff repair, designed to stimulate tendon regeneration. Clinical studies have reported reduced retear rates and favorable healing, and complications are considered rare [1,2,3]. Here, we present a rare case of loose body formation within the subacromial bursa, associated with fibrin deposition following rotator cuff repair using the REGENETEN® implant.
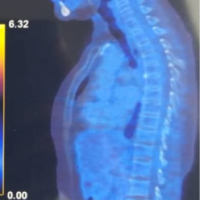
A 60-year-old man presented to our clinic with the right shoulder pain. On examination, his range of motion was 150° in forward flexion and 60° in external rotation, without mechanical catching. Magnetic resonance imaging (MRI) revealed a partial-thickness tear of the supraspinatus tendon (Fig. 1), and conservative management was initiated. However, as his nocturnal pain worsened, arthroscopy was performed 3 months later, confirming a partial tear. Arthroscopic rotator cuff repair was then carried out with augmentation using a medium-sized REGENETEN® implant, which was secured on the tendon surface (Fig. 2).
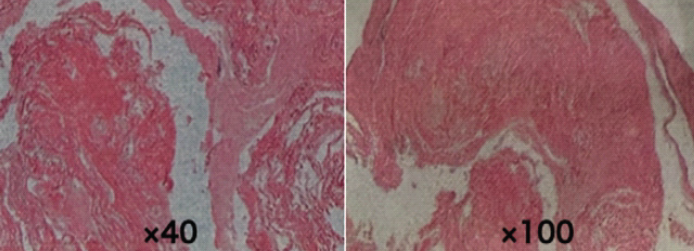
Figure 1: Pre-operative coronal T2-weighted magnetic resonance imaging (MRI) showing partial-thickness supraspinatus tear. Pre-operative coronal T2-weighted MRI of the right shoulder demonstrating a partial-thickness tear of the supraspinatus tendon (arrowhead). The image was obtained before any intervention.
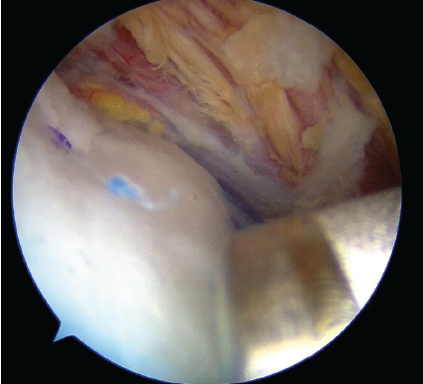
Figure 2: Arthroscopic view after rotator cuff repair with REGENETEN®. Intraoperative arthroscopic image of the right supraspinatus tendon after rotator cuff repair augmented with a medium-sized REGENETEN® bioinductive collagen implant.
Postoperatively, passive range-of-motion exercises were initiated at 2 weeks, followed by active exercises beginning at three weeks. At 6 weeks, the patient developed recurrent shoulder pain and mechanical catching. Despite continued rehabilitation, symptoms gradually worsened. At 6 months postoperatively, MRI demonstrated a hypointense structure within the subacromial bursa (Fig. 3). Suspecting this to be the cause of symptoms, repeat arthroscopy was performed.
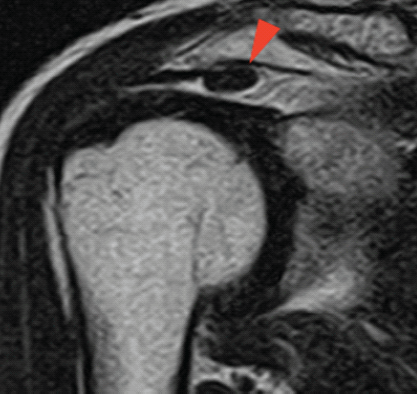
Figure 3: Post-operative coronal T2-weighted Magnetic resonance imaging (MRI) showing loose body within subacromial bursa. Coronal T2-weighted MRI of the right shoulder performed 6 months postoperatively, demonstrating a hypointense structure (arrowhead) within the subacromial bursa, consistent with a loose body formation. The previously torn rotator cuff appears to have been repaired.
Diagnostic arthroscopy identified a mobile, whitish loose body measuring approximately 16 × 13 mm. A medial staple from the REGENETEN® implant was identified at the center of the specimen, encapsulated by surrounding tissue, while the rotator cuff repair site itself remained intact (Figs. 4 and 5). The loose body was excised arthroscopically.
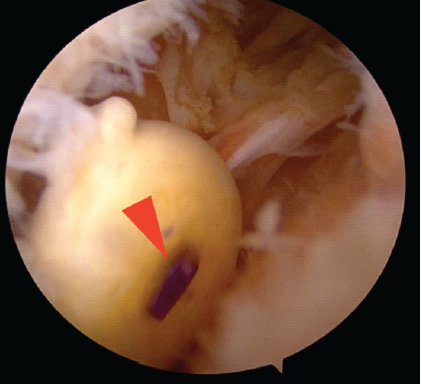
Figure 4: Arthroscopic removal of loose body containing medial staple. Arthroscopic image of the excised loose body measuring approximately 16 × 13 mm, with the medial staple (arrowhead) of the REGENETEN® implant embedded at its center, surrounded by fibrinous tissue.
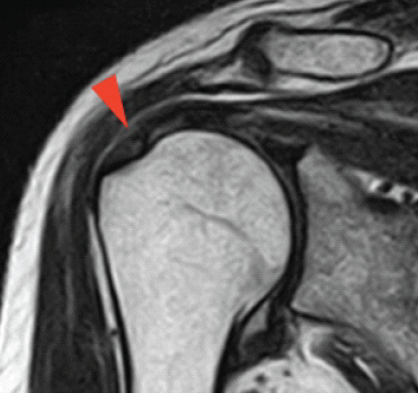
Figure 5: Post-excision arthroscopic view of healed rotator cuff. Arthroscopic image of the right supraspinatus tendon after removal of the loose body, showing complete tendon healing and intact repair site.
Histological examination demonstrated a fibrinous mass with infarction and necrotic fibrous tissue, surrounded by fibrocollagenous tissue (Fig. 6), findings consistent with a foreign body reaction. The post-operative course was uneventful, symptoms resolved within 1 month, and the patient returned fully to his construction work within 2 months.
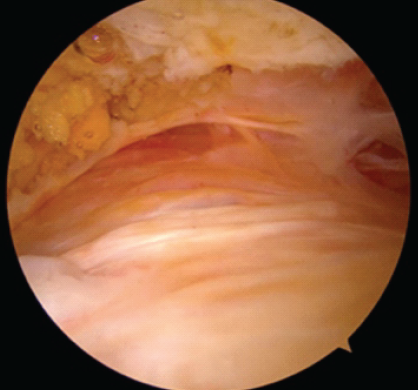
Figure 6: Histological examination of the excised loose body. Micrograph of the excised specimen demonstrating a fibrinous mass with infarction and necrotic fibrous tissue, surrounded by fibrocollagenous tissue, consistent with a foreign body reaction.
REGENETEN® does not require tendon-to-bone reattachment [4], thereby simplifying the surgical procedure, and has also been reported to be cost-effective [5]. Although its safety and efficacy have been well established, rare complications such as foreign body reactions and implant detachment have been described [2,3].
In contrast, poly-L-lactic acid anchors have been reported to elicit immune or systemic allergic reactions [6], leading to inflammatory bursitis and rice body formation [7]. Similar allergic reactions to poly-L-lactic acid screws have been documented in anterior cruciate ligament reconstruction [8]. Barad [9] suggested that degradation of polylactic acid implants could trigger exaggerated host responses. In such cases, joint swelling, pain, and rice body formation were observed, with symptoms improving after surgical removal.
In the present case, however, a discrete loose body within the subacromial bursa originated from a detached medial staple of the REGENETEN® implant. The implant itself is composed of bovine tendon collagen, polyether ether ketone staples on the lateral side, and both L- and D-isomers of polylactic acid staples on the medial side [7]. The excised specimen was surrounded by fibrin, but histology clearly distinguished it from rice bodies, as it contained implant-derived material rather than purely synovial products. Since L- and D-isomers of polylactic acid staples are bioabsorbable, they were not identifiable in this case, suggesting early detachment of the medial staple with subsequent foreign body reaction leading to loose body formation. The rotator cuff previously damaged and augmented with REGENETEN was found to be completely healed (Fig. 5), consistent with previous reports [10]. This finding suggests that REGENETEN may be highly effective in promoting rotator cuff repair.
To the best of our knowledge, this is the first documented case of loose body formation within the subacromial bursa caused by migration of a REGENETEN® bioinductive implant (medial staple). This distinction is clinically important, as rice body formation is typically associated with systemic inflammatory disease and requires evaluation for underlying rheumatologic conditions, whereas implant-derived loose bodies can be definitively treated by surgical excision. Awareness of this rare complication broadens the spectrum of potential adverse events related to bioinductive implants and should be considered in patients presenting with persistent post-operative mechanical symptoms following rotator cuff repair with REGENETEN®.
Surgeons should be aware that detached REGENETEN® implants may rarely lead to loose body formation in the subacromial bursa, and appropriate fixation during surgery is important to prevent this complication.
We report a rare case of loose body formation in the subacromial bursa caused by migration of a medial REGENETEN® staple. The rotator cuff repair itself was successful, demonstrating the efficacy of REGENETEN® in tendon healing. However, surgeons should be aware that detached implants may rarely cause loose body formation, and careful fixation during surgery is recommended to prevent this complication.
Surgeons should be aware of the rare risk of loose body formation from detached REGENETEN® implants and ensure secure fixation.
References
- 1. Bushnell BD, Connor PM, Harris HW, Ho CP, Trenhaile SW, Abrams JS. Retear rates and clinical outcomes at 1 year after repair of full-thickness rotator cuff tears augmented with a bioinductive collagen implant: A prospective multicenter study. JSES Int 2020;5:228-37. [Google Scholar] [PubMed]
- 2. Warren JR, Domingo-Johnson ER, Sorensen AA, Cheng AL, Latz KH, Cil A. Bioinductive patch as an augmentation for rotator cuff repair, a systematic review and meta-analysis. J Shoulder Elbow Surg 2024;33:2515-29. [Google Scholar] [PubMed]
- 3. Schlegel TF, Abrams JS, Angelo RL, Getelman MH, Ho CP, Bushnell BD. Isolated bioinductive repair of partial-thickness rotator cuff tears using a resorbable bovine collagen implant: Two-year radiologic and clinical outcomes from a prospective multicenter study. J Shoulder Elbow Surg 2021;30:1938-48. [Google Scholar] [PubMed]
- 4. Thangarajah T, Ling FK, Lo IK. Isolated bioinductive arthroscopic repair of partial-thickness rotator cuff tears using a resorbable collagen implant. JBJS Essent Surg Tech 2022;12:e21.00008. [Google Scholar] [PubMed]
- 5. Rognoni C, Nherera LM, Garofalo R, Guerra E, Longo UG, Taverna E, et al. Economic evaluation of a bioinductive implant for the repair of rotator cuff tears compared with standard surgery in Italy. Adv Ther 2023;40:5271-84. [Google Scholar] [PubMed]
- 6. Sivaloganathan S, Amr R, Shrivastava R, Relwani J. The Risotto sign – a severe inflammatory bursitis with rice body formation, complicating a rotator cuff repair with a bioabsorbable suture anchor. JRSM Open 2015;6:2054270414562986. [Google Scholar] [PubMed]
- 7. Root KT, Wright JO, Mandato N, Stewart BD, Moser MW. Subacromial-subdeltoid bursitis with rice bodies after rotator cuff repair with a collagen scaffold implant: A case report. JBJS Case Connect 2023;13:e22.00565. [Google Scholar] [PubMed]
- 8. Mastrokalos DS, Paessler HH. Allergic reaction to biodegradable interference Poly-L-lactic acid screws after anterior cruciate ligament reconstruction with bone–patellar tendon–bone graft. Arthroscopy 2008;24:732-3. [Google Scholar] [PubMed]
- 9. Barad SJ. Severe subacromial-subdeltoid inflammation with rice bodies associated with implantation of a bio-inductive collagen scaffold after rotator cuff repair. J Shoulder Elbow Surg 2019;28:e190-2. [Google Scholar] [PubMed]
- 10. Bokor DJ, Sonnabend D, Deady L, Cass B, Young A, Kampen CV, et al. Preliminary investigation of a biological augmentation of rotator cuff repairs using a collagen implant: A 2-year MRI follow-up. Muscles Ligaments Tendons J 2015;5:144-50. [Google Scholar] [PubMed]
The authors would like to thank Dr. Maiko Fujihara for providing valuable histological advice.