Giant cell tumor of carpal bones is a rare, aggressive condition that carries a high risk of recurrence, and en bloc excision with extended curettage and structural autografting can provide effective local control while preserving wrist function.
Dr. Ramesh Govindharaaju, Department of Orthopaedics, Government Medical College, Kozhikode, Kerala, India. E-mail: doctor.rameshg@gmail.com
Introduction: Giant cell tumor of bone (GCTB) is a benign but locally aggressive lesion, rarely affecting the carpus (<2% of hand GCTs), and is associated with recurrence rates up to 87%. Management of carpal GCT is challenging due to the limited bone volume, risk of damage to articular cartilage, and the need to preserve wrist function.
Case Report: A 38-year-old male presented with recurrent GCT of his left wrist 1 year after curettage and bone grafting. He had painful swelling, restricted motion, and an expansile lesion involving the distal carpal row and bases of the 2nd–4th metacarpals. He underwent en bloc excision with extended curettage and reconstruction using iliac crest autograft stabilized by Kirschner wires. Post-operatively, he had good pain relief and maintained good wrist motion. At 12 months, positron emission tomography - computed tomography showed no recurrence or metastasis; Mayo Wrist Score was 85 (Good) and the disabilities of the arm, shoulder and hand score was 8.3.
Conclusion: Recurrent carpal GCTB can be managed with en bloc excision, extended curettage, autografting, and temporary fixation, achieving adequate disease control and preservation of wrist motion. Long-term surveillance remains essential as recurrence is high in lesions of the carpal bones.
Keywords: Giant cell tumor, carpal bones, en bloc resection, iliac crest autograft, Kirschner wire fixation.
Giant cell tumor of bone (GCTB) is a benign but locally aggressive neoplasm accounting for 4–5% of primary bone tumors, most frequently affecting the epi-metaphyseal regions of long bones in young adults. Involvement of the hand is rare (~2%), with carpal bone lesions representing an even smaller subset [1,2]. Among these, the capitate is most frequently reported, though multifocal carpal involvement has also been described. Carpal GCTB is particularly challenging due to limited bone stock, proximity to vital joint surfaces, and historically high recurrence rates, reported as 60–87% in hand lesions [1].
Management strategies range from intralesional curettage with grafting to wide excision and reconstruction. While curettage offers bone preservation, recurrence is common, particularly in recurrent or multicentric disease, where aggressive resection may be warranted. Various adjuncts, such as phenol, cryotherapy, and hydrogen peroxide have been employed to reduce recurrence risk [3]. In recent years, denosumab has emerged as a therapeutic option; however, concerns regarding residual stromal cell proliferation, increased recurrence after curettage, and rare malignant transformation have limited its use [4,5]. We present a rare case of multicentric recurrent GCTB involving the distal carpal row and metacarpal bases in an adult male, managed successfully with en bloc excision, extended curettage, autografting, and Kirschner-wire fixation, with good early functional recovery.
History and clinical examination
A 38-year-old right-hand–dominant male from Northern Kerala presented to us with progressive pain and swelling of his left wrist for a duration of 4 years. He had initially undergone evaluation for the same complaints 4 years ago, when the swelling was smaller, and X-ray and magnetic resonance imaging (MRI) at that stage were suggestive of a simple bone cyst or enchondroma, and the condition was managed non-operatively. One year before presentation, his symptoms increased and a fresh MRI was suggestive of GCT of the carpal bones. At this stage, he underwent intralesional curettage with cancellous bone grafting at an outside center and biopsy confirmed it to be GCT of the carpal bones. 8 months later, he presented to us with recurrent pain, swelling, and decreased wrist motion (Fig. 1).

Figure 1: Clinical images (top left) depicting the pre-operative range of motion at the left wrist; pre-operative antero-posterior radiograph showing relative lucencies in the carpals and proximal ends of the metacarpals and reduced inter-carpal clear spaces (top right); sagittal, coronal, and axial T1 and T2/short tau inversion recovery magnetic resonance imaging sequences of the left wrist showing a lobulated expansile lesion (bottom row).
The patient’s family history was negative for similar conditions. He claimed to be a non-smoker and non-alcoholic. He did not have any comorbidities. On examination, the patient had a firm, tender, non-mobile swelling of size 7 × 6 cm over the dorsum of the wrist extending to the hand. Visual analogue score (VAS) was 6/10. Ranges of motion (affected/healthy side) were 40◦/80◦ of dorsiflexion, 40°/80° of palmar flexion, 90/90° of pronation, and 90/90° of supination. No limitations to the range of motion (ROM) were seen for any of the fingers.
Diagnostic investigations
Plain radiographs revealed lucencies in the distal carpal row and bases of 2–4 metacarpals with reduction in the clear spaces between individual bones (Fig. 1). Contrast-enhanced MRI demonstrated a relatively well-defined lobulated expansile lesion involving the distal row of the carpal bones with contiguous spread to the bases of the 2nd and 3rd metacarpals, measuring ~51 × 37 × 41 mm (Fig. 1). The mass abutted the volar flexor tendons at the capitate level and extended dorsally between the 3rd and 4th extensor compartments into subcutaneous tissue. It was bounded laterally by the abductor pollicis longus and medially by the extensor carpi ulnaris. There was mild erosive change at the 4th metacarpal base and scaphoid with marrow edema in the lunate and triquetrum. Signal characteristics were t1-intermediate and T2/short tau inversion recovery hyperintense with internal septations showing Gradient Recalled Echo blooming; enhancement was heterogeneous with non-enhancing areas – overall features suggestive of a locally aggressive GCT recurrence. Routine blood investigations and infection panel were negative. Serum Parathyroid hormone was within normal limits, ruling out Brown tumor. The chest radiograph was clear.
Differential diagnosis
GCT of the tendon sheath, GCT with secondary Aneurysmal bone cyst.
Surgical technique
Under tourniquet, through a dorsal midline approach, en bloc resection of the lobulated mass followed by extended curettage of surrounding tumor tissue was performed (Fig. 2), including removal of soft-tissue components between dorsal extensor compartments and careful protection of the flexor sheath and Median nerve volarly.
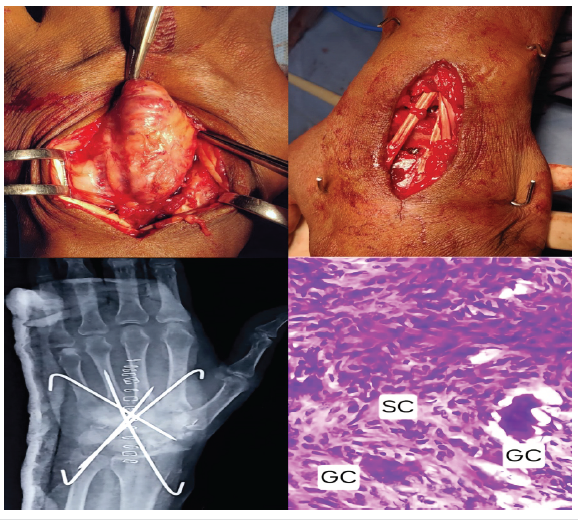
Figure 2: Intra-operative clinical image depicting the main lobulated mass being excised (top left); intra-operative clinical image after en bloc excision, iliac crest bone grafting, and stabilization with four K-wires. (top right); immediate post-operative antero-posterior radiograph of the wrist (bottom left); histopathological photomicrograph depicting the pathological spindle-shaped stromal cells and multi-nucleated giant cells (bottom right).
Residual cavity margins were curetted to punctate bleeding and burred, followed by application of 2 × 1-min cycles of hydrogen peroxide, while protecting surrounding soft tissues with moist gauze. A structural tricortical iliac crest autograft was fashioned to restore the distal carpal row and achieve normal carpal height, and a morselized cancellous bone graft was packed after debriding the distal cartilaginous surfaces of the proximal carpal bones to permit graft integration. Stable fixation was achieved with two smooth K-wires from the radius and ulna in a criss-cross fashion across the reconstructed column and attaining strong cortical purchase in the metacarpal shafts, one K-wire in retrograde direction from the 2nd metacarpal to the ulna, and one K-wire in retrograde direction from the 4th metacarpal base across the graft to the scaphoid (Fig. 2).
Histopathology
Resected tissues were sent for histopathological examination and Immuno-histochemistry. H&E sections showed a circumscribed neoplasm composed of sheets of spindly/oval cells admixed with many osteoclastic giant cells. Reactive new bone spicules were seen toward the periphery and in between. (Fig. 2) without malignant transformation was seen. The tumor cells were H3.3G 34W negative, Cytokeratin negative-ruling out carcinoma, SATB2 negative-ruling out osteoblastic malignancies, such as osteosarcoma. H3F3A G34W immunohistochemistry (IHC) is a highly sensitive and specific marker for GCTB. Gong et al. reported that 95% of 180 GCTBs harbored H3F3A mutations, most commonly G34W, with a minority showing alternative substitutions, highlighting that a small fraction may be IHC-negative [6]. Amary et al. similarly demonstrated high overall sensitivity (85–95%) for G34W IHC, though lower in small bone lesions, emphasizing that negative staining does not exclude GCTB [7].
Follow-up and outcomes
The patient’s wrist was immobilized in a below-elbow plaster slab for 4 weeks and then transitioned to a splint/brace. Early finger motion was encouraged from day 1. Gentle wrist mobilization was started at 7 weeks after removal of the K-wires, followed by progressive ROM and grip strengthening thereafter. The patient resumed his job as a driver at 3 months post-operatively. At 12 months after the surgery, the patient reported minimal discomfort with activities of daily living, no night pain, and no sensory complaints. He was able to bear weight on his wrist and perform his job as a driver without limitations. The surgical wound was well healed and there was no mass or localized warmth. Final ranges of motion were good (Fig. 3), with 50° dorsiflexion, 40° palmar flexion, 90° pronation, and 90° supination.

Figure 3: Post-operative clinical images with wrist range of motion (left); antero-posterior wrist radiograph taken at 12 months post-operatively (right).
Grip strength as a percentage of that of the healthy side was 80–85%, Mayo Wrist Score was 85 (Good), and disabilities of the arm, shoulder, and hand score was 8.3. VAS score was 1–2/10, but only during exertion. Surveillance imaging at 12 months follow-up showed maintained carpal alignment and good graft incorporation, with some relatively lucent areas in the middle of the iliac crest graft (Fig. 3). A Fluorodeoxyglucose positron emission tomography-computed tomography was done at this stage to rule out local recurrence, and it turned out to be negative for the same and also for distant metastasis.
GCT of bone is a benign but locally aggressive neoplasm, constituting 4–5% of primary bone tumors and most commonly affecting the epi-metaphysis of long bones, such as the distal femur, proximal tibia, and distal radius [1]. Occurrence in the carpal bones is exceedingly rare, accounting for <2% of all GCTs [2]. Treatment strategies vary between intralesional curettage and wide or en bloc excision. While curettage preserves bone, recurrence rates are high – up to 60–87% in hand lesions. McDonald and Schajowicz documented one of the first cases in 1992, treated with complete excision and yielding excellent long-term function without recurrence [2]. Subsequent reports have highlighted the challenges of diagnosis and treatment. Schmidt (2016) described a 51-year-old woman with capitate GCT who underwent multiple procedures and ultimately required total wrist arthroplasty [1]. Similarly, cases of multifocal carpal involvement, such as capitate with hamate or trapezium, have been reported, often necessitating en bloc excision and limited wrist fusion with iliac crest grafting to preserve hand function [8,9]. Adjunctive measures, such as phenol ablation and cryotherapy have also been employed to reduce recurrence [10]. Cases with less extensive involvement, especially those with only bony involvement sparing the soft tissue, have been managed adequately with either intralesional excision or en bloc resection and limited fusion with PolyMethylMethAcrylate cement augmentation as described by Ahlquist et al. (2024) and Gómez Mier et al. (2024) [11,12] In recent years, denosumab, a monoclonal antibody against Receptor Activator of Nuclear Factor Kappa-B ligand, has emerged as an adjuvant or neoadjuvant therapy for GCTB. Systematic reviews suggest it provides radiological and clinical improvement with reduced surgical morbidity, though its effect on recurrence and metastasis remains inconsistent [5]. Although neo-adjuvant Denosumab therapy has been known to reduce the tumor size, emerging evidence highlights the adverse effects of denosumab in GCTB. Denosumab selectively suppresses osteoclasts, but its effect on neoplastic stromal cells is minimal, allowing their persistence and proliferation after discontinuation of therapy. Denosumab-induced bone formation may entrap tumor cells, obscuring margins during curettage and thereby increasing recurrence risk. Rare but alarming is malignant transformation, with poor prognosis in an otherwise benign tumor affecting young patients [4]. In light of these concerns and uncertainties regarding optimal use, the use of denosumab was deferred in this patient.
Locally recurrent GCTB of the carpus can be managed with aggressive en bloc resection and extended curettage, structural iliac crest autografting, and stable K-wire fixation, offering pain relief and functional recovery while maintaining options for future salvage. An all-K-wire construct has two distinct advantages. The K-wires are removed at 6–8 weeks and post-removal this permits easier identification of recurrence, should it occur. New lesions would be more easily identifiable on both plain radiographs and on MRI without any metal artefacts confounding the image. Vigilant, long-term follow-up is essential in GCT of the carpus due to its high risk of recurrence and morbidity in recurrent cases.
Management of Giant cell tumor of the carpus can range from intralesional curettage with grafting or cemented fixation to en bloc resection and reconstruction with structural autograft. Kirschner-wire fixation, if done adequately, provides the advantage of leaving no metallic implants inside that can make radiological detection of possible recurrence easier.
References
- 1. Schmidt I. An unusual and complicated course of a giant cell tumor of the capitate bone. Case Rep Orthop 2016;2016:3705808. [Google Scholar] [PubMed]
- 2. McDonald DJ, Schajowicz F. Giant cell tumor of the capitate. A case report. Clin Orthop Relat Res 1992;279:264-8. [Google Scholar] [PubMed]
- 3. Chalidis BE, Dimitriou CG, Givissis PK. Tricortical bone grafting with limited midcarpal and carpometacarpal fusion for the treatment of giant cell tumor of the capitate. J Wrist Surg 2021;10:347-9. [Google Scholar] [PubMed]
- 4. Li H, Gao J, Gao Y, Lin N, Zheng M, Ye Z. Denosumab in giant cell tumor of bone: Current status and pitfalls. Front Oncol 2020;10:580605. [Google Scholar] [PubMed]
- 5. Luengo-Alonso G, Mellado-Romero M, Shemesh S, Ramos-Pascua L, Pretell-Mazzini J. Denosumab treatment for giant-cell tumor of bone: A systematic review of the literature. Arch Orthop Trauma Surg 2019;139:1339-49. [Google Scholar] [PubMed]
- 6. Gong LH, Zhang W, Sun XQ, Zhang M, Ding Y. DNA sequencing of H3F3A mutations in H3.3 immunohistochemistry-negative giant cell tumors of bone. Zhonghua Bing Li Xue Za Zhi 2021;50:190-3. [Google Scholar] [PubMed]
- 7. Amary F, Berisha F, Ye H, Gupta M, Gutteridge A, Baumhoer D, et al. H3F3A (histone 3.3) G34W immunohistochemistry: A reliable marker defining benign and malignant giant cell tumor of bone. Am J Surg Pathol 2017;41:1059-68. [Google Scholar] [PubMed]
- 8. Abdusamad V, Singh V, Jain R, Singh D. Giant cell tumor of the capitate and hamate: Case report and of literature review. J Wrist Surg 2020;9:425-30. [Google Scholar] [PubMed]
- 9. Tarng YW, Yang SW, Hsu CJ. Surgical treatment of multifocal giant cell tumor of carpal bones with preservation of wrist function: Case report. J Hand Surg Am 2009;34:262-5. [Google Scholar] [PubMed]
- 10. Mohaidat ZM, Al-Jamal HZ, Bany-Khalaf AM, Radaideh AM, Audat ZA. Giant cell tumor of bone: Unusual features of a rare tumor. Rare Tumors 2019;11:2036361319878894. [Google Scholar] [PubMed]
- 11. Ahlquist S, Gross JS, Nelson SD, Bernthal NM, Wessel LE. Treatment of a carpal giant cell tumor of bone with curettage and cemented capitohamate fusion. J Hand Surg Glob Online 2024;6:583-9. [Google Scholar] [PubMed]
- 12. Gómez Mier LC, Soto Montoya C, Franco Betancur A, Chaustre JF, Ramírez AF, Arroyave Rivera SA. Multifocal giant cell tumor of the carpus: Unusual presentation. Case report and review of the literature. Int J Surg Case Rep 2024;114:109127. [Google Scholar] [PubMed]










