Fibular tibialization is an effective, low-complexity technique for managing complex tibial non-union, especially in cases with compromised bone stock, providing a viable limb salvage option with minimal implant use and promising functional outcomes.
Dr. Sajal Maingi, Department of Orthopaedics, Dayanand Medical College and Hospital, Ludhiana, Punjab, India. E-mail: ssmaingi@gmail.com
Introduction: Non-union of long bone fractures, particularly of the tibia, presents considerable challenges due to poor vascularity, minimal soft-tissue coverage, and complications such as implant failure or infection from previous surgeries. Tibialization of the fibula remains a viable, though underreported, technique for addressing such complex cases.
Case Report: We report a case of a 26-year-old male with a history of poliomyelitis who presented with non-union of the left tibia following implant failure. Clinical evaluation revealed 4 cm limb shortening and varus deformity. Radiographs showed a broken 4.5 mm limited contact dynamic compression plate and multiple loosened screws. Given the intact fibula and adequate vascular and soft-tissue status, the Huntington method for tibialization was selected. The surgical approach included implant removal, debridement of non-union margins, and medial transfer of the fibula using anterolateral and lateral approaches. Postoperatively, the patient experienced transient vascular compromise, which resolved without intervention. At 6 months, radiographs confirmed proximal tibiofibular union, and the patient had regained functional mobility.
Conclusion: Fibular tibialization using the Huntington procedure offers a low-complexity, implant-sparing solution for managing tibial non-union, especially in patients with compromised bone and soft-tissue conditions. This case demonstrates favorable outcomes with minimal complications.
Keywords: Tibial non-union, fibular tibialization, Huntington procedure, implant failure, poliomyelitis, limb reconstruction.
Tibialization of the fibula is a time-tested procedure for managing tibial non-union, first popularized by Huntington [1] in 1904. This technique uses the fibula as a weight-bearing bone between the proximal and distal tibial segments. The weight-bearing axis transfers forces from the proximal tibia through the fibula, maintaining its vascular pedicle derived from the peroneal artery, and into the distal tibia, leading to tibiofibular synostosis. Despite its sound mechanical and biological principles, this technique requires expertise, particularly in vascularized graft harvesting, often involving a steep learning curve and complex plastic surgical interventions.
Dr. Tuli [2] introduced a modified “trap door” technique, wherein the proximal non-union edge of the tibia is freshened, and a trapdoor-like entry is created at the proximal tibial segment. The fibula is then transected and medialized into the proximal tibia’s medullary canal. A second-stage procedure, performed after 3–6 weeks, involves creating a similar trapdoor in the distal tibia for fibular fixation. This technique is contingent upon the presence of an intact fibula, vascularity, sensation in the sole, and supple soft tissues.
Catagni et al. [3] further advanced the approach by employing Ilizarov fixation and gradual medial translation of the fibula using olive wires. This technique involves predetermined osteotomies of the fibula’s proximal and distal ends, enabling medialization through controlled distraction. Indications include extensive bone loss unsuitable for bone transport or cases with inadequate bone regeneration due to poor quality. The method also supports bone regeneration and addresses compromised soft-tissue integrity or vascularity over the fibula.
Kassab et al. [4] described the use of Huntington’s classical technique in 11 cases of ipsilateral fibular transposition. The procedure was applied to patients aged 16–61 with segmental tibial bone loss ranging from 4 to 22 cm due to trauma, tumor resection, or osteomyelitis. The posterolateral approach was employed in most cases; however, an anterolateral approach was used when the anterior tibial artery (ATA) was compromised. Following decortication of the tibial ends, the fibula was mediatized and fixed using screws.
Clinical background
A 26-year-old male painter presented to the outpatient department of Safdarjung Hospital, New Delhi, with complaints of difficulty walking and shortening of the left lower limb for 2 years. The patient sustained a tibial fracture from a fall and underwent open reduction and internal fixation with plating at another facility. Post-surgery, he was unable to bear weight without a walking aid. The patient also reported a history of poliomyelitis in childhood.
Examination findings
On examination, the left thigh and calf muscles were atrophied. A non-adherent longitudinal surgical scar was present over the anterolateral aspect of the tibial shin. There was a 4 cm shortening of the limb and varus deformity. The fibula was intact along its entire length, with prominent proximal and distal ends extending beyond the joint line. Both the ATA and posterior tibial artery pulses were palpable, and the sole’s sensation was intact. Ankle and toe movements were normal.
Radiological findings
X-rays revealed thin femur and tibial diameters on the affected side compared to the contralateral limb (Fig. 1).

Figure 1: X-ray of bilateral hip with pelvis with femur to compare femoral width between poliotic (L) and non-poliotic limb (R).
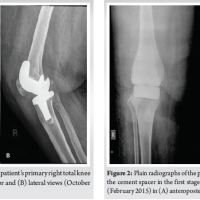
A non-union of the tibia with bone loss was observed, accompanied by a broken 4.5 mm narrow limited contact dynamic compression plate and multiple screw loosening (Fig. 2).
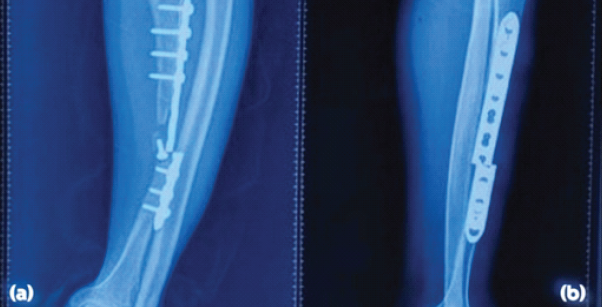
Figure 2: X-rays of left polio deformed tibia non-union with broken implant in situ, anteroposterior (a) and lateral (b) views.
Given the relatively larger fibular diameter, intact vascular and soft-tissue status, and absence of infection, the patient was planned for implant removal, freshening of non-union margins, and fibular tibialization using the Huntington method through anterolateral and lateral approaches.
Detailed surgical procedure
The patient was positioned supine on the operating table under pneumatic tourniquet control.
Step 1: Removal and tibial preparation: The prior anterolateral surgical incision (2 cm from the tibial crest) was utilized. Implants were removed, and the non-union margins of the proximal and distal tibial segments were freshened.
Step 2: Fibular dissection: A lateral incision was made, and the peroneal fascia was incised (Fig. 3).

Figure 3: Lateral incision for fibular graft harvest.
The superficial peroneal nerve was identified, mobilized, and protected. The lateral fibular surface was sharply dissected, retracting the peroneal muscles anteriorly while preserving a thin periosteal cuff.
The anterolateral intramuscular septum was freed from the compartment muscles and retracted. The fibula was osteotomized at the planned levels under C-arm guidance. A temporary K-wire was placed in the fibula as a joystick for maneuvering.
Step 3: Release of the interosseous membrane (IOM): The IOM was identified and incised longitudinally. Blunt dissection was performed between the IOM and tibialis posterior (TP) muscle layer, preserving the fibular attachments of the flexor hallucis longus (FHL) and TP muscles, along with the peroneal artery and venous pedicle. The tibial attachments of the IOM were similarly incised (Fig. 4).
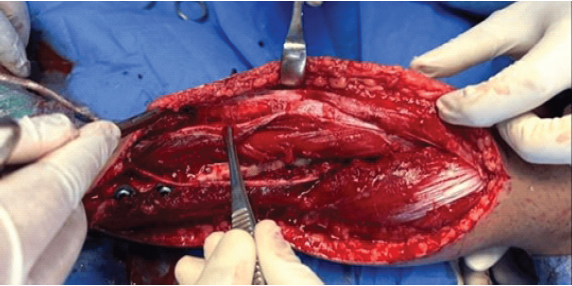
Figure 4: Superficial peroneal nerve identified and antero-lateral intermuscular septum incised, keeping the peronei in the posterior and A-L compartment anterior.
Step 4: Fibular medialization: With the IOM attachments released, the fibula was gently mediatized and aligned with the freshened tibial ends. The fibula was fixed to the proximal and distal tibial segments using multiple cortical screws with washers and K-wires (Fig. 5).
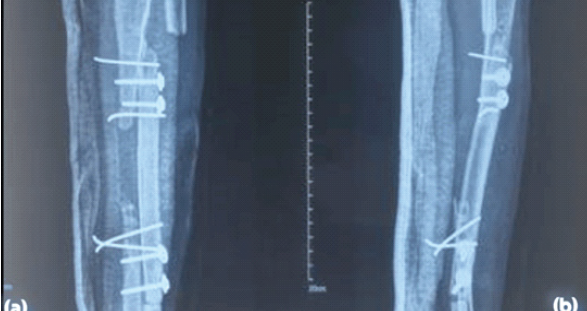
Figure 5: Immediate post-operative X-rays, anteroposterior (a) and lateral (b) views.
Follow-up X-rays were taken at 6 months (Fig. 6).
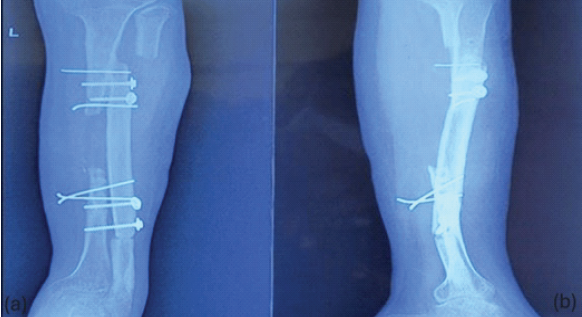
Figure 6: X-ray anteroposterior (a) and lateral (b) views after 6 months showing proximal tibio-fibular union (synostosis).
Non-union of tibial fractures [5,6,7] poses significant challenges, particularly in patients with complex anatomical and physiological considerations. Fibular vascular grafting, as described by Hertel et al. [8], provides a promising approach for such cases. However, the method described in this case modifies the original technique to address specific concerns related to soft-tissue damage, neurovascular compromise, and surgical efficiency.
The primary modification involved retracting the peronei muscles anteriorly and thoroughly dissecting the lateral surface of the fibula while preserving only the periosteum. This adjustment aimed to reduce soft-tissue tethering and avoid forceful retraction, thereby minimizing the risk of soft-tissue damage. Unlike the original method, which isolates the peroneal artery, our approach preserved the artery within the muscle pedicle (FHL and TP). This ensured adequate vascularity while avoiding the intricate dissection of the peroneal artery [9,10].
Protection of neurovascular structures was prioritized during the procedure. The anterior neurovascular bundle was cushioned by the IOM, and the posterior neurovascular bundle was protected by the TP muscle belly. These measures significantly reduced the risk of vascular injury and eliminated the need for delicate dissection. In addition, the high level of fibular osteotomy ensured minimal interference with the superficial and common peroneal nerves. The approach proved efficient, with the entire surgery completed within 2 h under tourniquet time.
Despite these precautions, a vascular complication was noted postoperatively. Computed tomography angiography revealed a segmental loss of opacification in the tibial artery below the proximal tibiofibular fixation point. However, the absence of clinical signs of ischemia, such as a warm limb with normal toe and ankle movements, indicated sufficient collateral circulation. Close observation over 72 h confirmed the resolution of vascular concerns without requiring further intervention. This underscores the importance of comprehensive monitoring and multidisciplinary collaboration, as exemplified by the consultation with the plastic surgery team.
The functional outcomes achieved in this case further validate the efficacy of the modified technique. Radiological evidence of proximal tibiofibular union was observed within 3 months, and the patient demonstrated a painless range of motion in the knee (0–130°) and ankle dorsiflexion (15°) with normal plantar flexion (30°). Functional outcome scores could not be applied as the affected limb had pre-existing poliomyelitis. Due to limited resources, magnetic resonance angiography could not be done to objectively assess the graft viability and vascular continuity. The cosmetic outcome, marked by a healed surgical scar, was also satisfactory.
While the modifications introduced in this case appear advantageous, they necessitate further investigation. Long-term outcomes, comparisons with the original technique, and applications in a larger cohort are needed to establish the generalizability of these findings. As both surgical and outcome assessments were performed by the same team, there may be an element of unintentional bias in evaluating results.
Nonetheless, this case highlights the potential of customized surgical approaches to address specific anatomical and clinical challenges, thereby improving patient outcomes.
This case highlights the utility of fibular vascular grafting with a modified surgical approach in managing complex tibial non-union, particularly in challenging scenarios such as a poliotic tibia with an implant in situ. The minimal reliance on implants makes it a valuable option for orthopedic surgeons. Despite encountering a temporary vascular complication, the overall outcome was successful, with evidence of union, restored function, and satisfactory cosmesis.
Future improvements in pre-operative planning, including detailed vascular imaging and multidisciplinary collaboration, could help mitigate such complications. This case underscores the importance of tailoring surgical techniques to individual patient anatomy and clinical conditions, demonstrating that even in complex cases, innovative approaches can lead to favorable outcomes. Further studies are encouraged to validate the effectiveness of this technique and refine its application.
This case report demonstrates the effectiveness of a modified fibular vascular grafting technique in managing complex tibial non-union, especially in previously infected poliotic limbs with retained implants. By minimizing soft-tissue trauma and preserving neurovascular integrity, this tailored approach offers a practical, low-implant alternative and may broaden treatment options for challenging orthopedic scenarios.
References
- 1. Huntington TW. VI. Case of bone transference: Use of a segment of fibula to supply a defect in the tibia. Ann Surg 1905;41:249-51. [Google Scholar] [PubMed]
- 2. Tuli SM. Tibialization of the fibula: A viable option to salvage limbs with extensive scarring and gap nonunions of the tibia. Clin Orthop Relat Res 2005;431:80-4. [Google Scholar] [PubMed]
- 3. Catagni MA, Camagni M, Combi A, Ottaviani G. Medial fibula transport with the Ilizarov frame to treat massive tibial bone loss. Clin Orthop Relat Res 2006;448:208-16. [Google Scholar] [PubMed]
- 4. Kassab M, Samaha C, Saillant G. Ipsilateral fibular transposition in tibial nonunion using huntington procedure: A 12-year follow-up study. Injury 2003;34:770-5. [Google Scholar] [PubMed]
- 5. Panteli M, Pountos I, Jones E, Giannoudis PV. Biological and molecular profile of fracture non-union tissue: Current insights. J Cell Mol Med 2015;19:685-713. [Google Scholar] [PubMed]
- 6. Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A, SCARE Group. The SCARE 2020 guideline: Updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg 2020;84:226-30. [Google Scholar] [PubMed]
- 7. Chaudhary MM. Infected nonunion of tibia. Indian J Orthop 2017;51:256-68. [Google Scholar] [PubMed]
- 8. Hertel R, Pisan M, Jakob RP. Use of the ipsilateral vascularised fibula for tibial reconstruction. J Bone Joint Surg Br 1995;77:914-9. [Google Scholar] [PubMed]
- 9. Gupta SP, Garg G. The Huntington procedure: Still a reasonable option for large tibial defects in paediatric patients. J Child Orthop 2014;8:413-21. [Google Scholar] [PubMed]
- 10. Parmaksızoğlu F, Cansü E, Ünal MB, Yener Ince A. Acute emergency tibialization of the fibula: Reconstruction of a massive tibial defect in a type IIIC open fracture. Strateg Trauma Limb Reconstr 2013;8:127-31. [Google Scholar] [PubMed]