Regular follow-up after closed reduction is essential to ensure maintenance of reduction, alignment, detect early dislocation, and guide timely modification of immobilization or rehabilitation.
Dr. Bhuvneshwar, Department of Orthopaedics, New Surgery Building, SN Medical College, Agra - 282002, Uttar Pradesh, India. E-mail: bhuvneshwar7013@gmail.com
Introduction: A rare but difficult condition to treat is neglected posterior dislocation of the hip. A delayed presentation results in soft-tissue contractures, poor bone stock, altered anatomy, and fibrous tissue formation in the acetabulum, all of which make reduction challenging. Despite the considerable risks and technical difficulties, total hip arthroplasty (THA) is frequently the recommended course of treatment in such chronic cases.
Case Report: We report the case of a 48-year-old man who had a 1.5-year-old posterior hip dislocation that had been neglected. After undergoing closed reduction and skin traction at a nearby hospital, the patient experienced a secondary displacement shortly after being released. He was treated conservatively at several local centers since he lacked access to definitive care. The patient had a 7 cm limb shortening with fixed flexion, adduction, and internal rotation deformity when they arrived at our facility. Imaging showed a deformed anterior wall, a fragmented posterior acetabular wall, and a femoral head with total loss of articular cartilage.
Surgical Procedure: A total hip replacement (THR) using cement was planned, and several backup plans, such as structural grafts, acetabular cages, dual mobility cups, and subtrochanteric osteotomy, were ready for any intraoperative difficulties. A posterior strategy was applied. Fibrous tissue and malformed bony walls covered the acetabulum; to medialize and stabilize the cup, careful dissection and gradual reaming were done. Osteotomy was performed on the femoral head. A medial calcar fracture was discovered during surgery, and cerclage wiring was used to treat it. The implant was a cemented stem with a highly porous acetabular cup.
Results: Recovery from surgery went smoothly. The patient’s limb length and function were restored along with a stable hip fixation.
Discussion: In developing nations, where delayed presentation is common due to limited orthopedic access and reliance on traditional bone setters, neglected posterior hip dislocations with acetabular fractures present significant reconstructive challenges. In these situations, THR necessitates careful pre-operative planning, cautious intraoperative technique to prevent neurovascular damage, and methods to deal with bone loss and soft-tissue contracture.
Conclusion: THA, which provides pain relief and functional recovery, is the recommended treatment for chronic posterior hip dislocation with acetabular involvement. However, because of its technical complexity, it requires careful planning and execution.
Keywords: Neglected posterior hip dislocation, total hip arthroplasty, acetabular fracture, limb shortening, bone loss management.
Hip dislocations that go unnoticed are uncommon. Neglected hip dislocations become more difficult to treat because closed reduction becomes impossible as the acetabulum fills with fibrous tissue [1,2]. The best course of action for treating neglected hip dislocations is still up for debate. Hemiarthroplasty, total hip replacement (THR), hip arthrodesis, the Girdlestone procedure, and subtrochanteric osteotomy are among the surgical techniques that have been documented [3,4]. Given the risks of iatrogenic femoral shaft fracture, unstable reduction from fibrous tissue overgrowth in the acetabulum, and avascular necrosis of the femur head, total hip arthroplasty (THA) is frequently advised for chronic posterior dislocation [1,5]. Nonetheless, an attempt at reducing neglected or unreduced hip dislocation may be made in younger patients with a preserved femoral head. Open reduction may lead to avascular necrosis and hip joint arthritis [3].
Over time, due to altered anatomy, the hip joint and surrounding areas undergo compensatory and adaptive changes. It is challenging to reduce the head in the acetabulum due to poor bone stock and a high-riding femoral head. Moreover, exposure is problematic due to capsular and muscular contractures. Fragments of the acetabular wall come together to form fibrous/bony unions [2,4]. In old cases and where avascular necrosis has set in, THA can be done, but its associated complications make it a challenging procedure [1,5].
In a posterior dislocation, the limb’s internal rotation attitude, classical flexion, and adduction may not be visible in neglected cases [3]. Technical difficulties arise when treating posterior, superior, and medial defects with uncontained acetabulum regions. Medialization, the development of a high hip center, or the application of a structural graft can all be used to cover the cup in THA. When delayed THR is used for post-acetabular fractures, cemented cups and reinforcement cages are more likely to loosen and fail [5].
Neglected posterior dislocation of the hip with acetabulum fracture is a rare case and is difficult to manage. Here, we describe a case of a 48-year-old patient who had posterior hip dislocation that was treated by a local practitioner initially, but later he came to our facility because of hip pain, inability to walk, and limitations in daily living activities. This study aimed to review the existing literature and describe the evaluation and surgical approach used in a complex case of neglected hip dislocation, utilizing the full range of therapeutic options available to the orthopedic surgeon.
A 48-year-old male presented to us with 1½-year-old posterior hip dislocation (Fig. 1) following a road traffic accident.
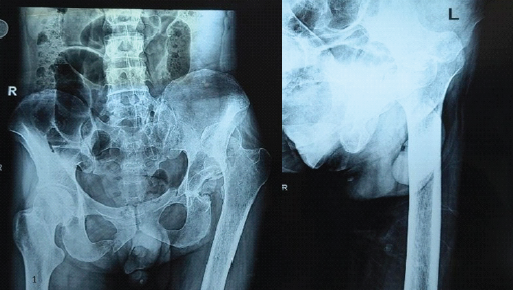
Figure 1: Preoperative plain radiograph showing posterior dislocation of the left hip.
He gave a history of subsequent treatment from the local hospital, where he was managed with closed reduction of the hip joint, and skin traction was applied. After this, the patient was discharged from the hospital and sustained a jerk while shifting in bed, and developed pain in his groin region. Patient went back to the hospital, but he could not find his treating doctor. Hence, after starting medication for pain relief, he came back to his home. The patient went to the hospital again after 1 month, where he was diagnosed with posterior hip dislocation. He was referred to a higher center and was advised of surgery.
The patient went to different local centers and was managed conservatively. After 1½ year, he presented to our center. The limb had shortening of 7 cm with fixed flexion, adduction, and internal rotation deformity (Fig. 2). He was initially managed with skeletal traction application for 1 month, but to no avail. Surgery was planned, and the patient was investigated for the same.

Figure 2: Clinical photograph showing 7 cm shortening with flexion, internal rotation.
Computed tomography scan and magnetic resonance imaging of the left hip were done to assess the viability of the head. The femoral head was rotated and slightly deformed with complete loss of articular cartilage without any evidence of avascular necrosis of the head of the femur. The posterior wall of the acetabulum appeared fragmented, and the anterior wall was also deformed (Fig. 3).
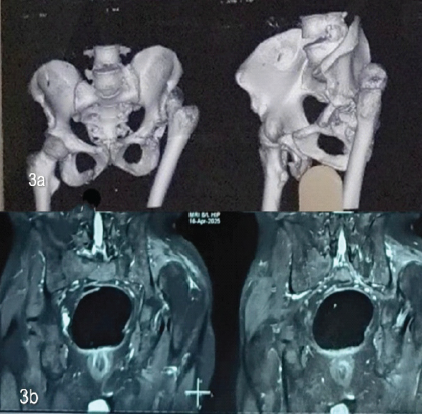
Figure 3: (a) Computed tomograph Images showing posterior superior dislocation of the left femoral head with the posterior column of left acetabulum appears fragmented; (b) Magnetic resonance imaging images showing complete loss of articular cartilage without any evidence of avascular changes in the femoral head.
Neglected posterior hip dislocation leads to secondary arthritis, femoral head necrosis, and severe functional limitation, making reconstruction difficult. Conventional methods often fail to restore function due to distorted anatomy. THR offers reliable pain relief, stability, and restoration of biomechanics in such complex neglected cases, justifying its use as the preferred treatment option.
Surgical procedure
Planning was done for THA keeping in mind all the options and complications that would arise during the case. Acetabular reconstruction plates, cables, and long locking compression plate for intraoperative femoral fractures and cannulated screws for femoral head graft, cemented and uncemented THA were kept as backup. Consent for limb shortening and subtrochanteric shortening osteotomy was also taken from the patient in case the femoral head could not be reduced. Furthermore, smaller cups were ordered in case a high hip center was required. Acetabular cages and a ring to combat bony defects were also ordered. A dual mobility implant was also kept as a backup in case there was instability.
Standard posterior approach in the lateral decubitus position was used (Fig. 4a). Since the trochanter was high riding, the anterior superior iliac spine and outline of the iliac crest were used as the essential landmarks, and the incision was extended more posteriory (Fig. 4b).
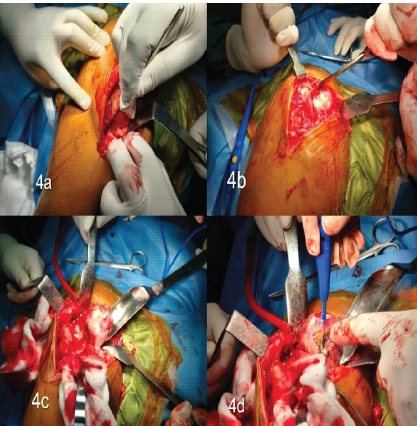
Figure 4: (a) Posterior(southern) approach used with incision given more posteriorly: (b) High riding greater trochanter and femoral head was identified (c) Intraoperative image showing chondrolysis of the femoral head, and thus total hip arthroplasty was planned intraoperatively; (d) Intraoperative image showing the release of the femoral head from surrounding soft tissue.
The limb was rotated, and the femoral head was palpated. The fascia was incised, and the gluteus maximus insertion was released from the femoral side. The gluteal maximus was split along the incision line to expose the femoral head. The femoral head had chondrolysis of the entire articular cartilage (Fig. 4c).
Short external rotators were identified and then detached from the trochanter close to their insertion. They were reflected posteriorly with stay sutures to help protect the sciatic nerve. The head was freed from surrounding soft tissues and was osteotomized (Fig. 4d).
Step 3: Visualization of the acetabulum and placement of the acetabular component
Gentle sustained traction was given to bring down the trochanter. The femoral shaft was retracted anteriorly with the help of a Czerny retractor, as the acetabulum could not be identified. The soft tissue was dissected to identify the acetabulum, but because of dense fibrosis, it was difficult. C-arm machine was then used to identify the acetabulum, and an artery forceps was put in the acetabular cavity to mark it. The posterior acetabular wall was absent, and the fractured anterior wall had inturned into the acetabular cavity and, with the associated fibrous tissue, had completely obscured the acetabulum. The anterior wall was repositioned, and the femur was retracted with a bone hook. The acetabulum was exposed, and fibrous tissue was removed with a cautery, keeping it inside the bony margins of the acetabulum. The floor of the acetabulum was identified, and initially a small reamer was used to medialize the cavity. Chondrolysis of the entire acetabular cartilage was also noted (Fig. 5a). The acetabular bone was very soft and osteoporotic. Hence, gradual reaming was done to prevent any fracture. The cup was gradually medialized and placed slightly superiorly to gain coverage of the remaining anterior and posterior walls (Fig. 5b). A highly porous small cup was placed and fixed with screws. The fixation was stable enough and did not require any additional bone graft. Furthermore, the posterior wall had so much fibrosis that releasing it posteriorly risked injury to the sciatic nerve. Hence, a decision to place a deeper cup and slightly superior to achieve stability was taken.
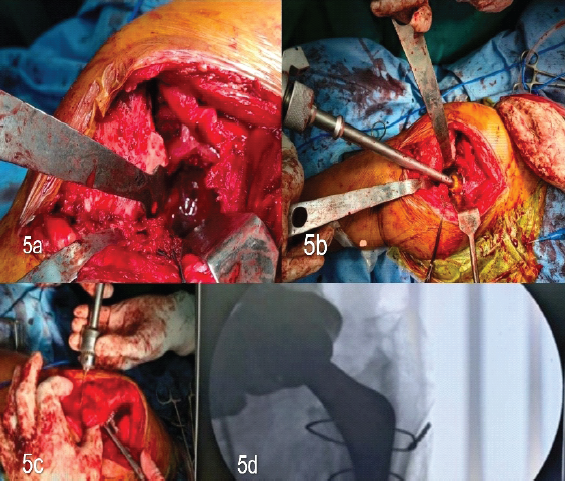
Figure 5: (a) Chondrolysis of the entire acetabular cartilage; (b) Intraoperative image showing use of small reamer to medialise the acetabular cavity and reduce the fractured inturned acetabular wall; (c) Intraoperative image showing managing interaoperative fracture with encerclage; (d) Fluoroscopic image showing placement of acetabular and femoral component with encerclage.
Step 4: Preparation for stem insertion
The femoral shaft was exposed for stem preparation. Initially, broaches for uncemented stems were used, but the femur was very osteoporotic, and the decision to put a cemented stem was taken. After broaching the canal, a trial was done after putting a small stem without a head to assess reducibility. Initially, even this was very difficult, and sustained traction was used to reduce the stem. Traction was continued for 10 min even after reduction, to gradually stretch the tissues. The knee joint was flexed to reduce sudden traction injury to the sciatic nerve. The trial stem and head were dislocated using a bone hook. Being a tight reduction, it was difficult to dislocate, and sustained traction with a bone hook was used to dislocate it. However, we encountered a medial calcar fracture on the anterior surface after removing the femoral stem. The fracture line extended nearly an inch below the calcar. Encerclage wires were used to prevent any further propagation of the fracture (Fig. 5c). The stem was then cemented using compression of the fracture with bone holding forceps. Extravasated cement was removed. No trial reduction was done to prevent any further fractures of the osteoporotic bone. Final reduction was done with a small-sized head, and the limb was put in flexion at the knee to prevent sciatic nerve injury, and then gradually straightened the leg (Fig. 5d).

Figure 6: (a) Post-operative plain radiograph; (b) Clinical photograph of patient: (c) Follow-up 1-month plain radiograph; (d) Follow-up 1-month clinical photograph of patient.
Fig. 6a and b shows the patient post-operative plain radiograph and clinical picture.
Fig. 6c and d shows the patient follow-up plain radiograph and clinical picture after 1 month.
Patient followed for 1st month and 3rd month, having pre-operative Harris Hip score of 14.04% which has improved to Harris Hip score of 48.55 and 62.20, respectively.
A hip dislocation raises the possibility of femoral head avascular necrosis. If reduction takes place within 6 h of the injury, the risk is <10%; if it takes longer, the risk is more than 50%. Furthermore, a possible long-term consequence after posterior hip dislocation is secondary osteoarthritis [6].
The occurrence of posterior hip dislocation is greater than that of anterior dislocation for the reason that the typical mechanism of injury is an axial load on a flexed and adducted hip. On the other hand, although anterior dislocations are infrequent, they frequently come along with fractures of the anterior column or femoral head, which might necessitate open reduction and fixation, sometimes employing a dual approach [7].
Since delayed presentation can result in complications such as limb shortening, abnormal gait, and difficulties with daily activities, treating neglected hip dislocation becomes more difficult over time. The limb may become fixed in flexion, adduction, and internal rotation as a result of soft-tissue contracture and fibrous tissue accumulation in the acetabulum.
Compared to Olasinde et al., [8] where initial heavy skeletal traction was applied for neglected posterior hip dislocation followed by bipolar hemiarthroplasty with good functional outcome, in our study, skeletal traction was given for 1 month but failed to achieve reduction. Hence, an alternative intraoperative strategy had to be planned to facilitate hip reduction. Our findings were consistent with those of Jain et al. [9], where skeletal traction failed in neglected posterior hip dislocations and open reduction was required, leading to good functional outcomes. It highlights the importance of timely surgical intervention when conservative measures prove ineffective. In contrast, transtibial skeletal traction was suggested by Selimi et al. [10] as a pre-operative treatment for patients who had hip dislocations older than a year. To enable a more successful reduction, this method aims to stretch the tense and contracted hip muscles.
According to research by Garret et al., [11] THR is the best course of action for chronic posterior dislocations with acetabular fractures. For dislocations that have been misaligned for more than 3 months, Garret advised THR, especially for those that are categorized as Type IV (acetabular rim and floor fractures) or Type V (femoral head fracture, with or without additional fractures). For neglected dislocations linked to Type II or higher acetabular fractures, Jain discovered that primary THA produced the best results.
A constrained THR was advocated by Chatterjee et al. [12] in a 2-year-old neglected dislocation to overcome instability. While our case report did not require constrained implants, the study underscores that implant selection should be individualized depending on the extent of soft-tissue laxity.
No previous study on management of neglected posterior hip dislocation with 7 cm of shortening has been reported, as was the case in our case. Compared to Mishra et al., [7] which recommended use of skeletal traction preoperatively in more than 1 year dislocation followed by THA even if head was not found soft intraoperatively, but in our study, old dislocation may not be beneficial with skeletal traction and preoperatively planning becomes challenging as back up of sub trochanteric shortening, intraoperative fracture management along with placement of deeper and vertical cup was crucial in this case.
A neglected posterior dislocation of the hip is difficult to treat. Care should be taken to screen polytrauma patients for hip dislocation. THA emerges as the preferred treatment in long-standing posterior hip dislocation with chondral damage. Long-term follow-up of these patients is required, as well as a larger number of cases need to be studied to ascertain the results of THA in such cases.
All polytrauma patients must be carefully screened for hip dislocation to prevent missed injuries, delayed diagnosis, and subsequent complications such as avascular necrosis, post-traumatic arthritis, and functional disability.
References
- 1. Arjun A, Harshvardhan M, Muthukumar T, Jetti A, Prakashappa TH, Jambu N. Technique and outcomes of total hip arthroplasty with or without sub-trochanteric shortening osteotomy for neglected post-traumatic hip fracture-dislocations: A case-series. J Clin Orthop Trauma 2020;11 Suppl 5:S767-72. [Google Scholar] [PubMed]
- 2. Li C, Hao J, Yu B, Wang F. External fixation-assisted reduction for the treatment of neglected hip dislocations with limb length discrepancy: A retrospective study of 13 cases. BMC Musculoskelet Disord 2019;20:408. [Google Scholar] [PubMed]
- 3. Aggarwal A, Singh AP, Maheshwari R, Pandey A, Arora A, Khan SA. Neglected traumatic hip dislocation in children: A retrospective series of 18 cases. J Pediatr Orthop B 2005;14:233-8. [Google Scholar] [PubMed]
- 4. Kumar S, Dahuja A, Narula MS, Garg S, Kaur R. Neglected hip dislocation: An unusual presentation, its management and review of the literature. Strategies Trauma Limb Reconstr 2017;12:189-92. [Google Scholar] [PubMed]
- 5. Sundaresh DC, Ramanath SK, Grover A, Gadi D. Uncemented total hip replacement after two years of neglected hip dislocation with fracture of posterior column and wall of the acetabulum. Trauma Mon 2016;21:e25301. [Google Scholar] [PubMed]
- 6. Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip—prognostic factors influencing the incidence of avascular necrosis of the femoral head. J Bone Joint Surg Br. 1986;68(4):508-11. [Google Scholar] [PubMed]
- 7. Mishra D, Jain M, Tripathy SK, Singh AK, Singh AK. Neglected Anterior dislocation of hip managed with total hip arthroplasty using dual approach: A case report and review of literature. J Orthop Case Rep 2024;14:141-7. [Google Scholar] [PubMed]
- 8. Olasinde AA, Olawoye OA, Alonge TO. Chronic posterior dislocation of the right hip treated with bipolar hemiarthroplasty in resource limited environment: A case report. Int J Surg Case Rep 2023;105:108152. [Google Scholar] [PubMed]
- 9. Jain M, Swaroop S, Kumar DS. Neglected posterior hip dislocation in adults presenting after one year managed successfully with single stage total hip arthroplasty: A case series. J Orthop Case Rep 2021;11:84-8. [Google Scholar] [PubMed]
- 10. Selimi V, Heang O, Kim Y, Woelber E, Gollogly J. Chronic hip dislocations: A rarity. How should we treat them? J Orthop 2016;13:431-6. [Google Scholar] [PubMed]
- 11. Garrett JC, Epstein HC, Harris WH, Harvey JP Jr., Nickel VL. Treatment of unreduced traumatic posterior dislocations of the hip. J Bone Joint Surg Am 1979;61:2-6. [Google Scholar] [PubMed]
- 12. Chatterjee D, Chakraborty PP, Goyal T, Ghosh S. Neglected hip dislocation: An unusual presentation, its management and review of the literature. Strategies Trauma Limb Reconstr 2017;12:195-9. [Google Scholar] [PubMed]









