Isolated lateral patellotibial ligament enthesopathy, though rare, should be considered in athletes presenting with unexplained lateral knee pain, and MRI plays a key role in its diagnosis.
Dr. Namdev Seth, Department of Radiodiagnosis, All India Institute of Medical Sciences, Gorakhpur - 273008, Uttar Pradesh, India. Email: namdevseth@gmail.com
Introduction: Patellofemoral stability is maintained by a complex interplay of osseous, muscular, and ligamentous structures, with the retinacular system playing a central role. While the medial patellofemoral and patellotibial ligaments are well characterized, the lateral patellotibial ligament (LPTL) has been less frequently described, and isolated pathology involving this structure is rarely reported in the literature.
Case Report: We report the case of a 23-year-old athletic male presenting with a 2-week history of activity-related lateral knee pain without preceding trauma. Clinical examination revealed focal tenderness at the tibial attachment of the LPTL without effusion, instability, or meniscal signs. Magnetic resonance imaging (MRI) demonstrated linear thickening of the lateral patellar retinaculum extending from the inferolateral patella to the anterolateral proximal tibia, consistent with the LPTL, which appeared thickened compared to the medial counterpart. Associated bone marrow edema at the tibial attachment near Gerdy’s tubercle suggested enthesopathy. Other intra-articular structures were normal. The patient was treated conservatively with physiotherapy, activity modification, and non-steroidal anti-inflammatory drugs, resulting in significant symptomatic improvement.
Conclusions: This case highlights isolated LPTL enthesopathy as a rare but important cause of lateral knee pain in athletes. Recognition of this entity on MRI is essential to prevent misdiagnosis and to facilitate appropriate conservative management.
Keywords: Patellofemoral stability, lateral patellotibial ligament, enthesopathy, overuse injury, knee magnetic resonance imaging.
Patellofemoral stability is maintained through a balance of osseous anatomy, ligamentous constraints, and dynamic muscular control. Among soft tissue stabilizers, the retinacular structures are essential in guiding patellar motion and preventing pathological tilt or translation [1]. The lateral patellar retinaculum consists of superficial fibers from the iliotibial band and vastus lateralis fascia, and a deeper layer comprising the lateral patellofemoral ligament (LPFL), lateral patellotibial ligament (LPTL), and patellomeniscal fibers [2].
While the medial patellofemoral ligament (MPFL) and medial patellotibial ligament (MPTL) have been extensively studied due to their role in recurrent patellar instability, their lateral counterparts remain less well described. The LPTL, a focal thickening of the deep lateral retinaculum, attaches from the inferolateral patella to the anterolateral tibia near Gerdy’s tubercle [3]. It contributes as a secondary stabilizer against excessive medial patellar translation.
Reports of isolated LPTL pathology are exceedingly rare. Most available literature discusses lateral retinacular involvement in maltracking syndromes or iatrogenic instability following lateral release [3]. Here, we describe a case of isolated thickening and enthesopathy of the LPTL in an athletic patient, emphasizing the importance of recognizing this structure on magnetic resonance imaging (MRI) and correlating it with clinical symptoms.
A 23-year-old athletic male presented with a history of localized pain in the left knee, predominantly over the lateral aspect for 2 weeks. The pain was mild to moderate in intensity, dull aching in character, aggravated by activities of daily living such as running, squatting, and climbing stairs. The symptoms were partially relieved with rest and on taking medications. There was no significant history of trauma or twisting injuries on the affected side. There was no history of similar complaints in any other joint.
On examination, there was point tenderness over the lateral aspect of the knee near the tibial attachment of the LPTL. There was no visible swelling, joint effusion, or deformity. Range of motion was full and pain-free till about 120° of flexion. In the last 10–20° of flexion, patient experienced mild discomfort. Clinical tests for ligamentous instability (including varus/valgus stress and Lachman’s test) were negative. There were no signs of meniscal injury on the McMurray’s test.
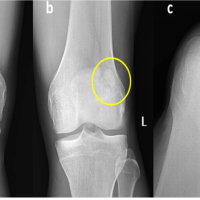
There was no significant finding on plain X-ray of the left knee in orthogonal views. MRI of the left knee demonstrated linear thickening of the lateral patellar retinaculum extending from the inferolateral patellar border to the lateral aspect of the proximal tibia (near tibial tubercle), corresponding to the LPTL. The LPTL appeared thickened in comparison to its medial counterpart. Associated bone marrow edema was noted at the anterolateral tibial cortex adjacent to Gerdy’s tubercle, precisely at the site of ligamentous attachment. On MRI, the marrow edema was seen as a hyperintense signal on T2-weighted (Fig. 1) and proton density fat-suppressed (PDFS) sequences (Fig. 2), with corresponding hypointensity on T1-weighted images. The signal alteration was limited to the subcortical marrow without evidence of cortical breach, fracture line, or intraosseous cyst formation. These findings are consistent with enthesopathic stress-related changes at the tibial insertion of the LPTL and correlated well with the patient’s localized pain and tenderness. The cruciate ligaments, collateral ligaments, menisci, and articular cartilage were all intact, and no joint effusion was observed.
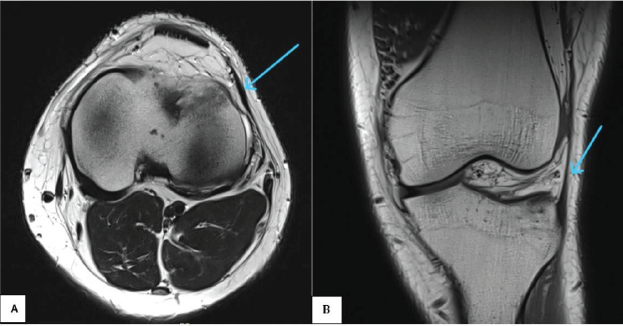
Figure 1: Axial (a) and coronal (b) T2-weighted magnetic resonance imaging images of the left knee joint show focal thickening of lateral patellar retinaculum (sky-blue arrow), which is classically described as the lateral patellotibial ligament.
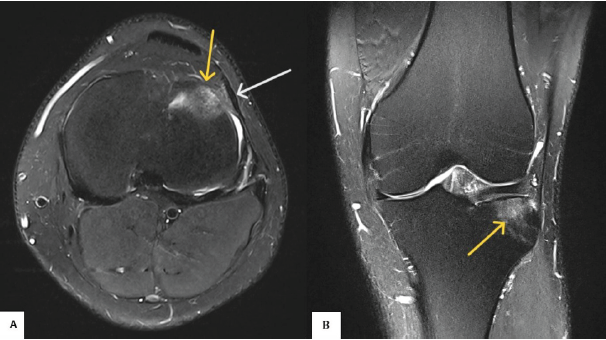
Figure 2: Axial (a) and coronal (b) proton density fat-suppressed images of the left knee joint show marrow edema (yellow arrow) at the anterolateral aspect of the tibial plateau (Gerdy’s tubercle) near tibial insertion site of lateral patellar tibial ligament (white arrow).
The patient was treated conservatively with rest, activity modification, a short course of non-steroidal anti-inflammatory drugs (NSAIDs), and focused physiotherapy. Rehabilitation included early pain-free range-of-motion exercises, quadriceps and VMO activation, and stretching of the ITB. A graded return to running and functional training was introduced once pain-free. At the 8-week follow-up, the patient reported complete resolution of pain and normal functional activity. Repeat MRI was not performed, as clinical improvement was satisfactory, and further imaging was reserved only for persistent or worsening symptoms.
The lateral retinacular complex provides both static and dynamic contributions to patellofemoral stability. Anatomical studies describe the superficial oblique fibers (from the ITB and vastus lateralis) and the deeper transverse fibers, including the LPFL and LPTL [2]. The LPTL is a discrete structure within the deep retinaculum, spanning from the inferolateral patellar border to the proximal tibia. Biomechanical work has highlighted its role as a restraint to abnormal patellar motion, although secondary to the MPFL [2,3].
Isolated LPTL injuries are uncommon and often under-recognized because gross instability or effusion is usually absent. In runners, repetitive microtrauma from knee flexion, sudden directional changes, and overuse can strain the ligament. Clinically, patients may present with lateral knee pain localized near the tibial insertion, mild tenderness, and discomfort during running, squatting, or stair climbing [3].
Radiologically, the LPTL is identified on MRI as a thin, low-signal band on axial and coronal sequences. In healthy knees, it is less conspicuous compared to the MPTL [4]. Pathological thickening, as seen in our patient, can be associated with focal enthesopathy, presenting as bone marrow edema at the tibial insertion site. Such marrow changes reflect traction-related microinjury and are consistent with the concept of enthesis organ pathology described in repetitive overuse syndromes [5].
Enthesopathies have been extensively documented in other sites such as the Achilles tendon and plantar fascia, where repetitive loading results in soft tissue thickening and adjacent marrow edema [5]. In our case, the absence of trauma and the history of athletic activity strongly support an overuse etiology of the LPTL enthesopathy.
Clinically, while MPFL and patellotibial ligament lesions are well reported in recurrent instability, there is a paucity of literature addressing isolated lateral retinacular or LPTL pathology [6]. LPTL reconstruction has been described only in the context of iatrogenic medial patellar instability following lateral release, where augmentation with graft tissue is considered [6]. This underscores the rarity of primary LPTL lesions such as the one we observed.
MRI is the imaging modality of choice for evaluating LPTL injuries [4,7]. In this case, the ligament demonstrated mild thickening with hyperintense signal on PDFS sequences, along with bone marrow edema at the anterolateral tibial insertion near Gerdy’s tubercle, correlating with the patient’s symptoms.
This case highlights the importance of correlating localized lateral knee pain with MRI evidence of LPTL thickening and tibial enthesopathy. Recognition of this entity prevents misdiagnosis. Management of LPTL enthesopathy is typically non-operative. Treatment centers on reducing mechanical stress through temporary activity restriction, short-term NSAID use, and structured physiotherapy. Rehabilitation emphasizes restoring normal patellofemoral mechanics by initiating gentle mobility work and targeted quadriceps activation, followed by progressive strengthening of the hip and knee musculature to reduce lateral pull on the patella. Gradual reintroduction of running and functional activities is undertaken once pain diminishes. Most patients recover well with this approach, and further imaging is rarely required unless symptoms fail to improve [8,9].
Surgical intervention is rarely required, considered only for persistent symptoms or associated instability. Awareness of LPTL anatomy and imaging features is essential for accurate diagnosis and prevention of chronic lateral knee pain in athletes [10].
Isolated LPTL pathology is an uncommon but clinically relevant cause of lateral knee pain, especially in athletic individuals. MRI plays a critical role in identifying ligamentous thickening and associated enthesopathy, which may otherwise be overlooked.
Awareness of this structure and its imaging appearance helps guide accurate diagnosis and appropriate conservative management.
Isolated LPTL enthesopathy, though rare, should be considered in athletes presenting with unexplained lateral knee pain, and MRI plays a key role in its diagnosis.
References
- 1. Merican AM, Sanghavi S, Iranpour F, Amis AA. The structural properties of the lateral retinaculum and capsular complex of the knee. J Biomech 2009;42:2323-9. [Google Scholar] [PubMed]
- 2. Garcia-Mansilla I, Zicaro JP, Martinez EF, Astoul J, Yacuzzi C, Costa-Paz M. Overview of the anterolateral complex of the knee. World J Clin Cases 2022;10:8474-81. [Google Scholar] [PubMed]
- 3. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc 2012;20:331-6. [Google Scholar] [PubMed]
- 4. Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: Injury patterns and assessment of risk factors. Radiographics 2010;30:961-81. [Google Scholar] [PubMed]
- 5. Benjamin M, McGonagle D. The enthesis organ concept and its relevance to the spondyloarthropathies. Adv Exp Med Biol 2009;649:57-70. [Google Scholar] [PubMed]
- 6. Marberry K, Boehm K, Korpi F, Johnson J, Kondrashov P. Anatomical and radiographic characterization of the lateral patellofemoral ligament of the knee. Mo Med 2020;117:469-74. [Google Scholar] [PubMed]
- 7. Dainer RD, Barrack RL, Buckley SL, Alexander AH. Arthroscopic treatment of acute patellar dislocations. Arthroscopy 1988;4:267-71. [Google Scholar] [PubMed]
- 8. Feller JA, Feagin JA Jr., Garrett WE Jr. The medial patellofemoral ligament revisited: An anatomical study. Knee Surg Sports Traumatol Arthrosc 1993;1:184-6. [Google Scholar] [PubMed]
- 9. LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000-10. [Google Scholar] [PubMed]
- 10. Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy: A double-blind, randomized controlled trial. Am J Sports Med 2014;42:610-8. [Google Scholar] [PubMed]