Multidisciplinary evaluation is essential for managing fractures in HSS, while documenting such rare trauma presentations expands the limited evidence available to guide future similar cases.
Dr Luis Mariano Rentería Ramírez, Instituto Mexicano del Seguro Social (IMSS), General Zone Hospital with Family Medicine No. 2, Saltillo, Coahuila, Mexico, Department of Traumatology and Orthopedics, Blvd. Venustiano Carranza 3458, El Kiosco, 25240 Saltillo, Coahuila. E-mail: luism12_06@hotmail.com
Introduction: Hallermann–Streiff syndrome (HSS) is a globally rare congenital condition of unknown etiology, with approximately 200 cases reported worldwide. Although its skeletal morphological abnormalities are well recognized, traumatic and periprosthetic fractures have not been documented. These anatomical variations pose significant challenges for determining the optimal therapeutic approach, particularly in acute trauma settings.
Case Report: We report the case of a 12-year-old male from Mexico who presented to the emergency department after a fall from standing height, sustaining direct trauma to the right hemibody. His medical history included a right femoral fracture 5 years earlier. Intraoperative findings revealed pronounced femoral shaft thinning, and open reduction and internal fixation (ORIF) with a low-profile plate was performed. The post-operative course was favorable, with satisfactory clinical and radiological progression at 6 months. This case illustrates the complex skeletal involvement associated with HSS and underscores the need for individualized surgical planning within a multidisciplinary framework.
Conclusion: This case contributes valuable evidence to the limited literature on HSS by documenting a traumatic fracture requiring surgical management in a patient with this rare syndrome. Recognition of skeletal abnormalities and coordinated multidisciplinary care are essential for improving diagnosis, treatment, and follow-up in similar future presentations.
Keywords: Hallermann–Streiff syndrome, traumatic fracture, periprosthetic fracture, rare congenital disorder.
Hallermann–Streiff syndrome (HSS) is an extremely rare condition, with approximately 200 cases reported globaly [1]. First described by Aubry in 1893, and later characterized by Hallermann and Streiff, it is primarily recognized for its craniofacial dysmorphisms, ocular anomalies, and dermatologic features [2,3] a recent estimates a prevalence of 1 in 10 million in Japan [4]. The syndrome includes features such as bird-like facies, mandibular hypoplasia, microphthalmia, congenital cataracts, blue sclerae, hypotrichosis, cutaneous atrophy, and dental anomalies [5,6]. Although the exact etiology remains unknown, some cases have been associated with mutations in the GJA1 gene, suggesting a possible dominant inheritance pattern, though this remains unconfirmed [7]. Skeletal abnormalities, including cortical thinning of long bones, poor ossification, and disproportionate stature, are reported. However, no prior documentation exists of traumatic or periprosthetic fractures in patients with HSS. This case highlights such an occurrence, emphasizing the need for awareness of underlying bone fragility and anatomical considerations in surgical planning.
A 12-year-old male with confirmed HSS presented to the emergency department following a fall from standing height during transfer to his wheelchair. He reported immediate right thigh pain, functional limitation, and localized edema without skin lesions. The patient had a prior history of right femoral shaft fracture treated with ORIF using a dynamic compression plate (DCP) in 2020. On physical examination, he exhibited multiple classical features of HSS, including craniofacial dysmorphia, hypotrichosis, nystagmus, strabismus, blue sclerae, mandibular hypoplasia, and syndactyly. Skeletal findings included scoliosis and previous fracture history.
Diagnostic assessment
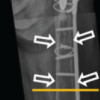
Plain radiographs of the right femur were obtained (Fig. 1), revealing a diaphyseal mid-third fracture with a simple fracture line located immediately distal to the previous osteosynthesis material, cortical thinning was noted without pathological lesions.
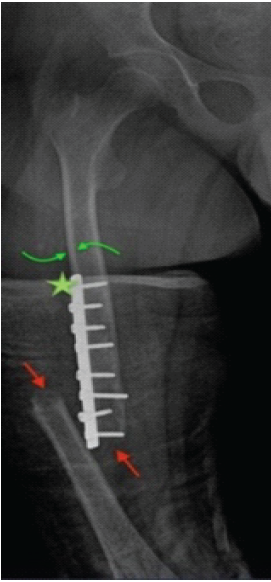
Figure 1: Anteroposterior (AP) X-ray of the right femur, February 26, 2025. AP radiograph of the right femur showing a displaced periprosthetic femoral fracture with varus angulation, displacement, and shortening (red arrows). Previous osteosynthesis material is visible without signs of fatigue or loosening (star). Adequate corticomedullary differentiation is observed in the diaphyseal region, along with cortical thinning (green arrows).
Therapeutic intervention
Surgical intervention involved the removal of the prior DCP and ORIF using a new 10-hole, 4.5 mm narrow DCP. Intraoperative findings included femoral shaft thinning and elongation with adequate cortical consistency and no gross pathological changes. Alignment was restored in axial and sagittal planes, verified by intraoperative imaging. Postoperatively, the patient was managed with restricted weight-bearing and allowed passive and active mobilization.
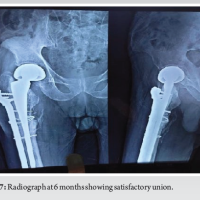
He was discharged on postoperative day 2 with close follow-up scheduled. At 3 weeks, the patient was asymptomatic, with proper wound healing and functional mobility. Radiographs confirmed maintained reduction and early consolidation (Fig. 2). At 6 months, he remained pain-free with good hip mobility and radiological evidence of Grade IV callus formation (Fig. 3).
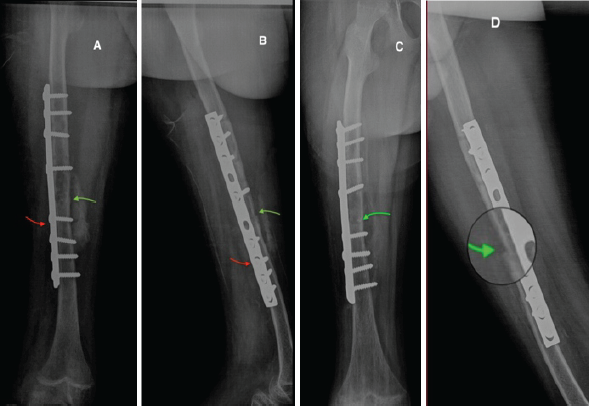
Figure 2: X-ray follow-up. Immediate post-operative anteroposterior (AP) (A) and lateral (B) radiographs showing fracture line reduction (green arrow) and placement of osteosynthesis material (red arrow); (C) AP; and (D) lateral radiographs at 3 weeks postoperatively showing maintained reduction and Grade II consolidation (green arrow).
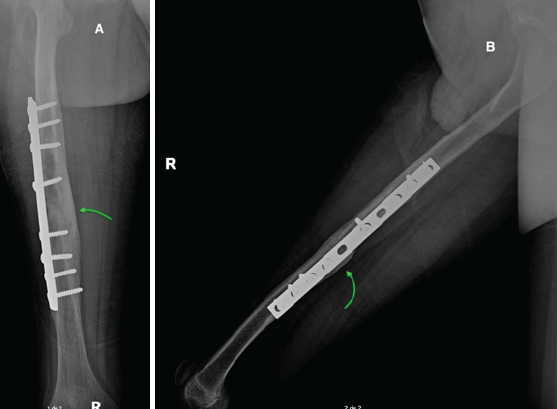
Figure 3: X-ray 6 months follow-up. Anteroposterior (A) and lateral (B) radiographs at 6-month follow-up showing Grade IV consolidation with prominent callus formation (green arrow), osteosynthesis material without signs of fatigue or loosening, and proper alignment without rotation or angular deformities.
The skeletal phenotype in HSS includes craniofacial and axial deformities, but literature on long bone fragility is sparse. Radiologically, features include poor ossification, thin diaphyseal cortices, and narrow medullary canals [8,9]. In our patient, cortical thinning was evident, though the corticomedullary differentiation appeared adequate. Existing literature reports congenital fractures in neonates with HSS, typically discovered during the perinatal period or at autopsy (Table 1). These cases often lack a traumatic trigger and are associated with impaired bone remodeling or abnormal ossification. However, no prior reports have documented traumatic or periprosthetic femoral fractures in HSS patients, making this case unique.
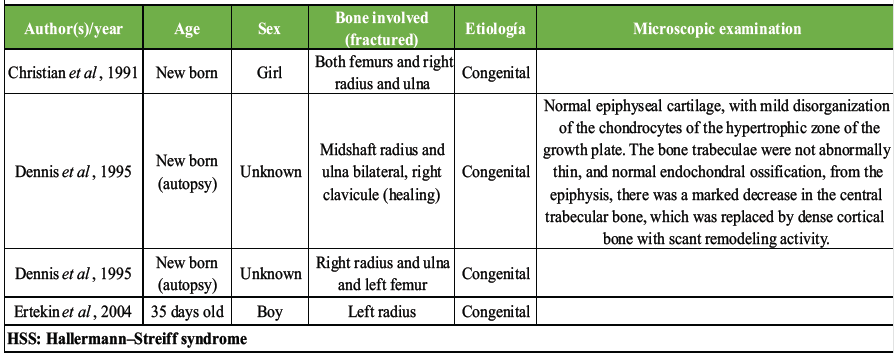
Table 1: Summary of reported cases of fracture in patient with HSS
This case suggests that, beyond craniofacial anomalies [10], patients with HSS may possess underlying long bone fragility predisposing them to fractures even under low-energy trauma. The presence of previous internal fixation may further increase the risk of peri-implant fractures due to stress shielding and local bone remodeling. From a surgical standpoint, challenges include anatomical abnormalities, altered biomechanics, and limited literature to guide implant selection or weight-bearing protocols. A low-profile DCP was selected to accommodate the narrow femoral diameter and avoid further periosteal damage. The favorable outcome observed supports the use of tailored internal fixation in such patients, along with close monitoring of healing progression. It underscores the importance of multidisciplinary management, involving orthopedic, genetic, and rehabilitation teams.
This is the first reported case of a traumatic periprosthetic femoral fracture in a patient with HSS. The case illustrates the need for heightened clinical awareness of possible bone fragility in these patients, especially in the context of previous fractures or implants. Multidisciplinary management, individualized surgical planning, and vigilant follow-up are essential in ensuring optimal outcomes. Documenting such cases contributes to the scarce literature and may guide future management strategies for similar rare presentations.
HSS, though extremely rare, can present with unanticipated long bone fragility, making patients vulnerable to fractures even after minor trauma. Awareness of these skeletal abnormalities, combined with multidisciplinary evaluation and individualized surgical planning, is critical to prevent complications, optimize recovery, and expand the scarce evidence base to guide management of future cases.
References
- 1. Genetic and Rare Diseases Information Center. Hallermann-Streiff Síndrome. Genetic and Rare Diseases Information Center (GARD) – an NCATS Program; 2020. Available from: https://rarediseases.info.nih.gov/diseases/288/hallermannstreiff-syndrome#ref_5346 Accessed September 18, 2025 [Google Scholar] [PubMed]
- 2. Cohen MM Jr. Hallermann-Streiff syndrome: A review. Am J Med Genet 1991;41:488-99. [Google Scholar] [PubMed]
- 3. Preudhomme R, Veyssiere A, Ambroise B, Benateau H. Hallermann Streiff syndrome: Cranio-facial manifestations systematic review and report of two cases. J Stomatol Oral Maxillofac Surg 2022;123:e219-23. [Google Scholar] [PubMed]
- 4. Numabe H, Kosaki K. Prevalence of Hallermann-Streiff syndrome in a Japanese pediatric population. Pediatr Int 2021;63:474-5. [Google Scholar] [PubMed]
- 5. Ertekin V, Selimoğlu MA, Selimoğlu E. Non-lethal Hallermann-Streiff syndrome with bone fracture: Report of a case. Ann Genet 2004;47:387-91. [Google Scholar] [PubMed]
- 6. Kaissi AA, Handelbauer A, Klaushofer K, Grill F. Mid-diaphyseal endosteal thickening with subsequent medullary narrowing in a patient with Hallermann-Streiff syndrome. J Clin Med Res 2011;3:328-30. [Google Scholar] [PubMed]
- 7. Schmidt J, Wollnik B. Hallermann-Streiff syndrome: A missing molecular link for a highly recognizable syndrome. Am J Med Genet C Semin Med Genet 2018;178:398-406. [Google Scholar] [PubMed]
- 8. Pereira De Godoy AC, Pereira De Godoy HJ, Pereira De Godoy JM. Hallermann-Streiff syndrome and lower limb lymphedema with nasal obstruction. Case Rep Med 2022;2022:1520880. [Google Scholar] [PubMed]
- 9. Christian CL, Lachman RS, Aylsworth AS, Fujimoto A, Gorlin RJ, Lipson MH, et al. Radiological findings in Hallermann-Streiff syndrome: Report of five cases and a review of the literature. Am J Med Genet 1991;41:508-14. [Google Scholar] [PubMed]
- 10. Dennis NR, Fairhurst J, Moore IE. Lethal syndrome of slender bones, intrauterine fractures, characteristics facial appearance, and cataracts, resembling Hallermann-Streiff syndrome in two sibs. Am J Med Genet 1995;59:517-20. [Google Scholar] [PubMed]