Surgical management of symptomatic Bertolotti syndrome can provide significant pain relief and functional recovery in selected patients who fail conservative treatment.
Dr. Joaquín Zúñiga Soria, Universidad del Desarrollo - Clínica Alemana de Santiago, Chile. E-mail: jzunigasoria.med@gmail.com/j.zunigas@udd.cl
Introduction: Bertolotti syndrome (BS) is an underdiagnosed cause of chronic low back pain associated with lumbosacral transitional vertebrae (LTV). Although conservative management is usually the first-line approach, a subset of patients remains refractory and may benefit from surgical intervention. Reports on surgical outcomes remain scarce, and evidence is predominantly limited to isolated case reports. We present a case series of three patients with symptomatic BS who did not respond to conservative management and underwent surgical treatment.
Case Report: Three patients (two females, one male; age range 21–32 years) presented with chronic low back pain and radicular symptoms. All had imaging findings consistent with Castellvi Type II or Type III LTV. Prior management included physical therapy, non-steroidal anti-inflammatory drugs, image-guided injections, and activity modification, with inadequate symptom relief. Surgical management consisted of resection of the anomalous transverse process articulation in all cases. Clinical follow-up evaluated pain Visual Analog Scale, function, and return to activity. All patients reported significant improvement in pain and functional outcomes, with sustained benefit at final follow-up (6–24 months). No neurological complications or reoperations occurred.
Conclusion: Surgical resection may be considered in carefully selected patients with symptomatic BS who fail conservative management. This case series reinforces the importance of appropriate diagnosis, patient selection, and surgical expertise in addressing this uncommon but impactful cause of persistent low back pain. Further studies with larger cohorts are needed to better define indications and outcomes.
Keywords: Bertolotti syndrome, lumbosacral transitional vertebra, low back pain, minimally invasive spine surgery, case series.
Bertolotti syndrome (BS) is an uncommon but clinically significant cause of chronic lumbar pain, particularly in young adults. This syndrome refers to the association between a lumbosacral transitional vertebra (LTV) and mechanical low back pain, usually without specific findings in magnetic resonance imaging (MRI) [1]. LTV is a congenital anomaly characterized by articulation or fusion of the L5 transverse process with the sacrum or ilium, which results in a transitional joint. This condition was first described by Mario Bertolotti in 1917 [2]. The Castellvi classification is the most commonly used method for categorizing LTV and divides the classification into four types according to their type of union and laterality [3]. Although LTV is observed in up to 30% of the population, only a few individuals develop symptoms. The prevalence of BS in patients with low back pain is between 4.6% and 7% [4]. The exact physiopathology has not been clearly established, and it is postulated that pain may occur due to mechanical overload of the pseudoarticulation, subchondral inflammation, early disc degeneration, or segmentary movement restriction [5,6]. The diagnosis of BS requires clinical and radiological correlation, in which imaging techniques such as X-rays, MRI, and computed tomography (CT)/single-photon emission computed tomography (SPECT)-CT are fundamental. The diagnosis is confirmed through selective corticosteroid injection of the transitional articulation with local anesthetics, which helps distinguish between symptomatic LVT and incidental imaging findings [7]. Conservative treatment includes analgesia, physiotherapy, and lifestyle modifications. In refractory cases, surgical management has been described, particularly through resection of the symptomatic transverse process. However, surgical management should be indicated in patients without advanced disc degeneration, facet joint or sacroiliac osteoarthritis, and in the absence of bone fusion [5,8]. This study describes a series of three BS cases of Castellvi type IIa with surgical management through resection of the symptomatic transverse process, with adequate clinical follow-up. The diagnostic criteria and surgical indications are also discussed.
Patient 1
A 33-year-old male presents with long-standing left low back pain with predominantly mechanical characteristics. Pain presents in the morning and quickly improves when the patient is sitting or standing. No radicular pain, paresthesia, or neurologic deficits are present. Upon physical examination, localized left lumbar pain was noted, with no signs of radicular involvement affecting the lower extremities. Imaging studies revealed lumbosacral articulation Castellvi type IIa, with radiological signs of pseudoarthrosis. MRI and X-ray confirmed the presence of LTV with partial fusion between the transverse process and the sacrum. MRI also revealed subchondral bone edema in the contact area between the L5 transverse process and the sacrum, which suggests active mechanical overload (Fig. 1).
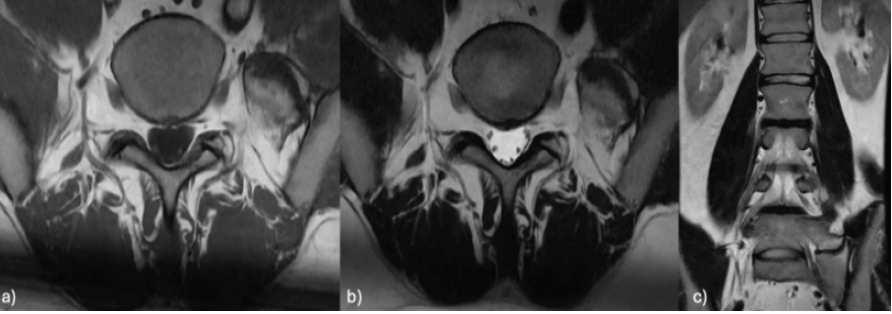
Figure 1: Lumbar magnetic resonance imaging in axial T1 (a) and T2 (b) sequences and coronal T2 (c) sequences showing subchondral edema at the contact area between the left L5 mega-transverse process and the sacrum.
Owing to the patient’s symptoms, a diagnostic corticosteroid injection into the pseudoarticulation was performed, with positive results, resulting in significant pain relief. Given this favorable response and the persistence of disabling symptoms, surgical management with pseudoarticulation resection was selected. Surgery was performed through a modified Wiltse-type posterolateral approach assisted by neuronavigation to ensure accurate resection limits and prevent retroperitoneal damage. The conflicting left transverse-sacroiliac osseous components were removed.
Patient 2
A 14-year-old female with no previous medical history presented with 9 months of focal low-back pain. The first episode occurred during a volleyball match, with no associated trauma. Pain was initially managed conservatively, without clinical improvement.
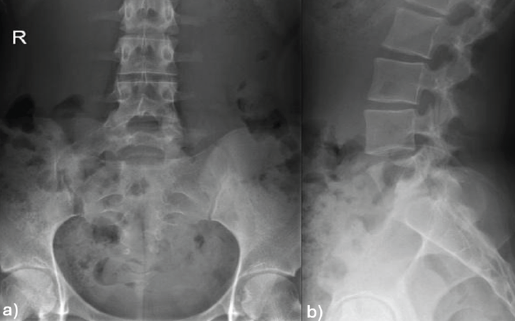
Figure 2: Lumbar spine X-rays in the anteroposterior (a) and lateral (b) views showing a right L5 mega-transverse process.
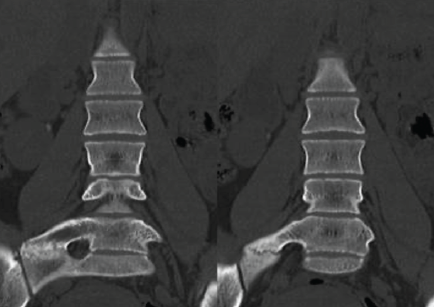
Figure 3: Computed tomography scan of the lumbar spine in the coronal view: Right L5 mega-transverse process pseudoarticulated with the sacrum.
X-rays (Fig. 2), CT scan (Fig. 3), and MRI revealed a LVT with a right hypertrophic transverse process at L5, which articulated with the sacrum and was compatible with Castellvi type IIa. SPECT findings indicated focal hypercaptation within the pseudoarticulation, suggesting symptomatic focus (Fig. 4).
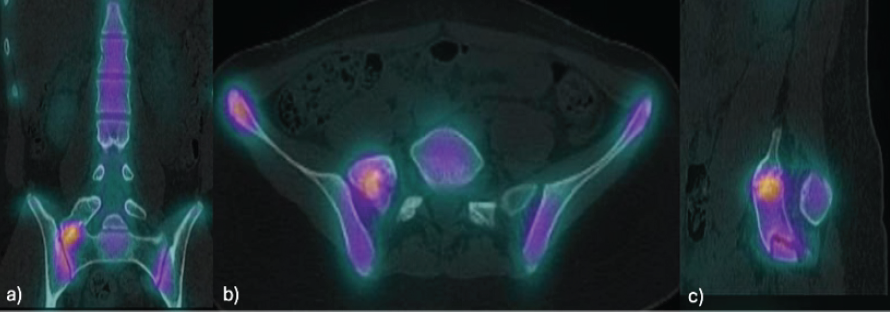
Figure 4: Single-photon emission computed tomography-computed tomography of the lumbosacral region: Focal area of increased uptake at the pseudoarticulation between the right L5 mega-transverse process and the sacrum in the coronal (a), axial (b), and sagittal (c) views.
Within this context, two diagnostic corticosteroid injections of the compromised segment were performed with favorable, yet transient, responses. Owing to pain persistence and functional limitations, surgical resection of the transverse process was suggested. Surgery was performed through the Wiltse posterolateral approach at the right lumbosacral level. Fluoroscopic guidance was used to localize the transverse-sacral pseudoarticulation (Fig. 5) and to define the anatomical limits of the mega-transverse process.
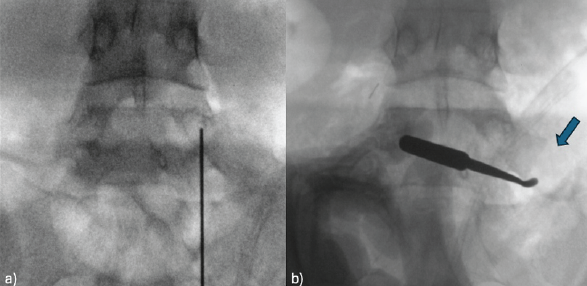
Figure 5: An intraoperative fluoroscopic image. (a) Preop and (b) postop with resection of the transverse-sacral pseudoarticulation (arrow) are shown.
An osteotomy was performed, followed by resection of the fragment, which preserved the L5-S1 joint. Complete resection was confirmed with an intraoperative CT scan (O-arm). Three months postoperatively, the patient presented significant clinical improvement with only occasional lumbar pain in extension exercises, especially during training (Fig. 6).
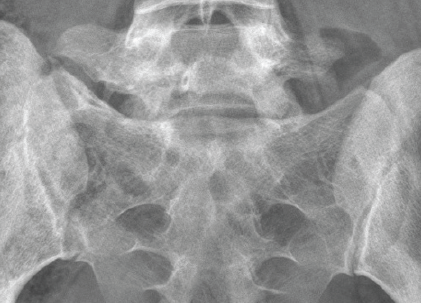
Figure 6: Lumbosacral X-ray at the 2-year follow-up.
Patient 3
A 33-year-old male presented with low back pain for 2 months predominantly on the left side. The patient reported a progressive increase in pain during the previous weeks, which limited his daily activities.
A physical examination revealed significant paravertebral muscle spasms and contracture in the absence of neurologic deficit. Imaging studies revealed that LTV with contact between the L5 transverse process and sacral ala was compatible with symptomatic pseudoarticulation. For diagnostic confirmation and therapeutic purposes, a selective corticosteroid injection was performed within the contact area between the L5 mega-transverse process and the left iliac wing, which achieved complete pain relief. However, pain recurred on the 3rd post-operative day. Thus, surgical management was indicated with resection of the mega-transverse process aided by neuronavigation. Adequate osteotomy was confirmed through an intraoperative CT scan. Post-operative evolution was favorable and complete pain resolution was achieved.
BS is an uncommon yet relevant cause of chronic low back pain, especially in young and physically active patients [1]. Although LTV is present in up to 30% of the population [2], only a few of these patients develop symptoms attributable to abnormal transitional articulation. In the present case series, all patients presented with Castellvi type IIa LTV, which is defined as a unilateral pseudoarticulation between the L5 transverse process and the sacrum or ilium [3]. The exact pathophysiology of BS remains controversial. The literature suggests that pain originates from chronic mechanical overload during pseudoarticulation, early adjacent disc degeneration, or segmentary movement restriction [4,9]. Elster demonstrated that patients who present with LTV had a greater incidence of disc protrusion at the immediate superior level [5]. In contrast, Aihara et al. reported less disc degeneration at the L5-S1 level in patients with transitional fusion, possibly due to movement restriction [6]. As an uncommon pathophysiological mechanism, the literature describes low back pain contralateral to the mega-transverse process facet caused by altered load transmission to the contralateral articulation. This hypothesis is supported by contralateral symptomatic relief after resection of the mega-transverse process [7]. BS diagnosis requires correlation between clinical and radiological findings. Imaging must reveal clear transitional articulation and its symptomatic nature must be confirmed by selective corticosteroid injection, which remains the diagnostic standard [8]. Within the present series, all patients underwent diagnostic infiltration with local anesthetics, which allowed the identification of pseudarthrosis as the pain origin. With respect to treatment, previous studies have reported favorable outcomes with surgical resection in selected patients [10,11]. Nevertheless, not all patients with BS are eligible for surgery. According to Sumarriva et al., the following cases should be excluded from surgical management: Severely degenerated or rudimentary intervertebral discs where there is no functional segment; significant sacroiliac or adjacent facet joint osteoarthritis, which suggests that pain could originate from a site other than the pseudoarticulation; and complete bone fusion (Castellvi type III) cases, in which resection is not technically viable or has questionable benefits [11]. In these cases, conservative management, referral to chronic pain specialists, or lumbosacral fusion may be considered. In this case series, all patients met the following resection criteria: Localized pain, positive diagnostic corticosteroid injection, and the absence of significant disc degeneration or osteoarthritis. A Wiltse-type approach was used, with intraoperative navigation in two patients. All patients had favorable functional outcomes, with complete pain resolution and a return to their previous activities. Resection of a mega-transverse process forming a pseudoarticulation with a lumbosacral segment that retains an intact intervertebral disc and functional facets contributes to eliminating the source of pain both by resecting the inflamed pseudoarticulation and by restoring the anatomy and normal mechanical load. The results presented in our patient series are consistent with those of previously published series, which reported that surgical resection is effective in some selected cases [10,11]. Nevertheless, further investigations with long-term follow-up and comparative studies that standardize the surgical criteria, define the role of fusion in complex cases, and establish evidence-based therapeutic guidelines are needed.
BS must be considered as a differential diagnosis of chronic low back pain, especially in young patients with imaging findings of LTV. Its diagnosis requires careful clinicoradiological correlation, and confirmation of the pain source through selective corticosteroid injection is essential. Surgical resection of the symptomatic mega-transverse process is safe and effective in patients presenting with refractory mechanical pain and in the absence of significant disc degeneration, adjacent osteoarthritis, and consolidation of bone fusion. This report presents three cases involving the Castellvi IIa vertebra. Surgical resection was associated with favorable clinical outcomes and functional reintegration without complications. Notably, not all patients with LVT require surgical management. Adequate surgical selection on the basis of rigorous clinicoradiological criteria is essential for obtaining optimal results and avoiding unnecessary interventions. Further prospective studies are needed that compare surgical and conservative management with long-term observations to standardize the treatment of BS.
Recognizing BS as a potential cause of persistent low back pain is essential, especially in young patients with refractory symptoms. When conservative measures fail, surgical resection of the pseudo-articulation can offer substantial pain relief and functional improvement in carefully selected cases.
References
- 1. Quinlan JF, Duke D, Eustace S. Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br 2006;88:1183-6. [Google Scholar] [PubMed]
- 2. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984;9:493-5. [Google Scholar] [PubMed]
- 3. Konin GP, Walz DM. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol 2010;31:1778-86. [Google Scholar] [PubMed]
- 4. Almeida DB, Mattei TA, Sória MG, Prandini MN, Leal AG, Milano JB, et al. Transitional lumbosacral vertebrae and low back pain: Diagnostic pitfalls and management of Bertolotti’s syndrome. Arq Neuropsiquiatr 2009;67:268-72. [Google Scholar] [PubMed]
- 5. Elster AD. Bertolotti’s syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976) 1989;14:1373-7. [Google Scholar] [PubMed]
- 6. Aihara T, Takahashi K, Ogasawara A, Itadera E, Ono Y, Moriya H. Intervertebral disc degeneration associated with lumbosacral transitional vertebrae: A clinical and anatomical study. J Bone Joint Surg Br 2005;87:687-91. [Google Scholar] [PubMed]
- 7. Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimäki H. Lumbosacral transitional vertebra: Relation to disc degeneration and low back pain. Spine (Phila Pa 1976) 2004;29:200-5. [Google Scholar] [PubMed]
- 8. Brault JS, Smith J, Currier BL. Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine 2001;26:226-9. [Google Scholar] [PubMed]
- 9. Nardo L, Alizai H, Virayavanich W, Liu F, Hernandez A, Lynch JA, et al. Lumbosacral transitional vertebrae: Association with low back pain. Radiology 2012;265:497-503. [Google Scholar] [PubMed]
- 10. Santavirta S, Tallroth K, Ylinen P, Suoranta H. Surgical treatment of Bertolotti’s syndrome. Follow-up of 16 patients. Arch Orthop Trauma Surg 1993;112:82-7. [Google Scholar] [PubMed]
- 11. Sumarriva G, Cook B, Celestre P. Surgical resection of Bertolotti syndrome. Ochsner J 2022;22:76-9. [Google Scholar] [PubMed]