Tenosynovial giant cell tumors, despite being benign, require a meticulous surgical technique for complete excision along with the use of adjuvants such as chemical cauterization (e.g., phenol) and a long-term follow-up due to a high potential for local recurrence.
Dr. Soumyajit Bhattacharjee, Department of Orthopaedics, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India. E-mail: drsoumyajitbhattacharjee@gmail.com
Introduction: Tenosynovial giant cell tumor (TSGCT), formerly known as pigmented villonodular synovitis, is a rare, benign, locally aggressive neoplasm originating from the tendon, bursa, or synovium. It is broadly categorized into localized TSGCT (L-TSGCT) and diffuse TSGCT types, with the localized form more commonly affecting the tendon sheaths of the hand and fingers. This report describes a rare presentation of a L-TSGCT involving the flexor tendon sheath of the right thumb in a 40-year-old male, managed successfully with complete excision.
Case Report: We report a case of a 40-year-old male who presented with a 1-year-old history of a slowly growing, painless mass over the right thumb, along with restriction of movement. Clinical examination revealed a firm, non-tender, mobile mass measuring approximately 3 cm × 3 cm. X-ray revealed a soft-tissue shadow with pressure scalloping and erosion over the distal phalanx of the right thumb. Magnetic resonance imaging (MRI) demonstrated a well-defined lobulated T1 and T2 isointense lesion with erosion of the distal phalanx of the thumb. The patient underwent complete marginal surgical excision along with the use of local adjuvant chemical cauterization of the bony erosion bed with 88% phenol for 1 min to prevent recurrence. Intraoperatively, it was a well-encapsulated, yellowish-brown nodular mass adherent to the flexor sheath without infiltration into the neurovascular bundle. The post-operative course was uneventful, and the patient achieved a full range of motion at 4 months of follow-up.
Conclusion: L-TSGCT of the thumb is uncommon but should be considered in the differential diagnosis of soft-tissue swellings in the digits. MRI assists in delineating lesion extent and planning surgical excision. Histopathological analysis confirms the diagnosis of L-TSGCT. The tumor’s characteristic imaging profile and indolent clinical course highlight the need for accurate pre-operative diagnosis. Complete surgical excision, preferably preserving digital function, remains the gold standard, offering a high chance of cure. Use of adjuvants such as phenol might reduce the risk of recurrences, especially in cases of bony involvement. Long-term follow-up is strictly advisable.
Keywords: Tenosynovial giant cell tumor, localized, pigmented villonodular synovitis, soft-tissue swellings, phenol, bony erosion
Tenosynovial giant cell tumor (TSGCT) is the second most common tumor of the hand, following ganglion cysts, and represents a benign but potentially recurrent neoplasm (10–50%) which may arise from the tendon or bursae, or the synovium. It was first described by Chassaignac in 1852 as “fibrous xanthoma” of the tendon sheath. Earlier, it was thought to be a reactive process, but it is now considered a neoplastic etiology due to the translocation involving locus 1p13, which leads to overexpression of colony-stimulating factor 1 (CSF-1) [1,2]. The lesion’s characteristic histology-proliferation of mononuclear cells with multinucleated giant cells and hemosiderin-laden macrophages supports a neoplastic nature. The exact etiology, however, remains uncertain, and various hypotheses include chronic inflammation, trauma, and metabolic disturbances. Among the two forms – localized and diffuse, the localized form is more common, accounting for nearly 80–90% of all TSGCTs of the hand and typically affects adults between the 3rd and 5th decade of life with a slight female predominance [3]. The most common location is usually the palmar surface of the radial three digits near the distal interphalangeal joints. Although benign, TSGCT can cause significant functional impairment when involving the digits because of the compact anatomy and crucial role of tendons in the pinch and grasp mechanism, and typically presents as a painless, slow-growing mass. Sometimes it may become painful along with rapid progression. The localized form is typically treated by simple excision, contrasting sharply with the aggressive nature and management complexities of the diffuse form. Instances of scalloping of bone due to the pressure effects of large TSGCTs have been reported, which may be directly linked to increasing chances of recurrences [4]. In such cases, the use of adjuvant agents, such as phenol, cryotherapy, or electrocautery, can be advocated to reduce recurrence, although no proper guideline exists as to the bony management of such cases [5,6]. We present this case report of a localized TSGCT of the flexor tendon sheath of the right thumb in a 40-year-old male, along with evidence of bony scalloping, managed successfully by en bloc excision, along with the use of phenol as an adjuvant to prevent any local recurrence.
A 40-year-old right-hand-dominant male, carpenter by occupation, presented with a 1-year history of a gradually enlarging swelling on his right thumb. It was insidious in onset and was associated with pain on movement and restricted thumb flexion at the interphalangeal joint, which led to difficulty in grasping. There was no preceding trauma, infection, or systemic symptoms. On physical examination, a firm, well-circumscribed, multilobulated mass was present involving both the volar and dorsal aspects of the right thumb, measuring approximately 5 × 3 cm. The overlying skin was tense and shiny, and the mass moved slightly with tendon motion, suggesting its origin from the flexor sheath (Fig. 1 and 2).

Figure 1: Clinical image from the front and back views.

Figure 2: Clinical image from the lateral view and while making a fist.
The range of motion (ROM) of the interphalangeal joint was restricted, whereas the metacarpophalangeal joint was fully mobile. There was no distal neurovascular deficit.
Initial plain radiographs (anteroposterior and oblique) of the right hand demonstrated significant soft-tissue swelling around the thumb, along with pressure erosion (scalloping) around the distal phalanx of the right thumb (Fig. 3).

Figure 3: Pre-operative X-ray of the right hand (anteroposterior and oblique views) shows soft-tissue swelling over the thumb, along with erosion and scalloping on the distal phalanx of the thumb.
A magnetic resonance imaging (MRI) scan was performed, revealing a well-defined, lobulated T1 mass adjacent to the flexor pollicis longus tendon. The mass demonstrated a T1 and T2 isointense lesion with hypointense septation within, which is noted to arise from the soft-tissue plane of the distal phalanx of the right thumb. The lesion appears heterointense on proton density (PD) sequences without any suppression on PD fat saturation and shows intense heterogeneous post-contrast enhancement. There was associated scalloping and erosion of the distal phalanx of the thumb (Fig. 4).
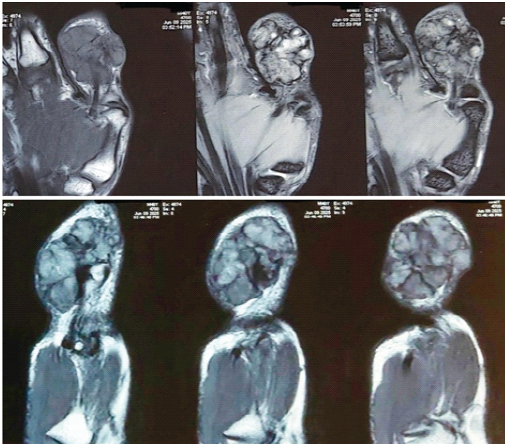
Figure 4: Magnetic resonance imaging showing a lobulated mass adjacent to the flexor pollicis tendon of the thumb.
Surgical excision was performed under regional anesthesia, using a wide zig-zag incision (Bruner type) that was made over the thumb (Fig. 5).
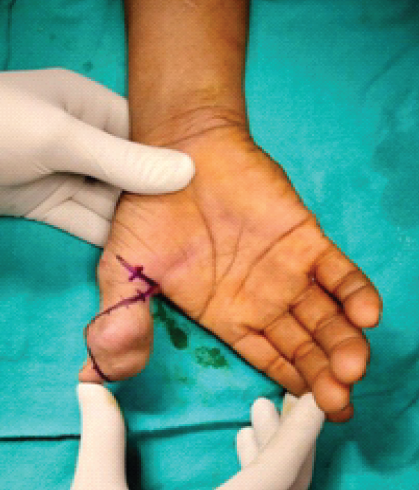
Figure 5: Intraoperative picture showing skin marking – A zig-zag Bruner type incision taken on the volar aspect of the right thumb.
A yellowish brown, multinodular, pseudo-encapsulated tumor was identified. The mass was found to be adherent to the flexor pollicis longus tendon and infiltrated the metacarpophalangeal joint capsule with direct involvement of the eroded distal phalanx of the thumb. The extensor tendon was uninvolved. Meticulous dissection was performed to achieve complete marginal excision of the tumor while protecting both the digital arteries of the thumb (Fig. 6).
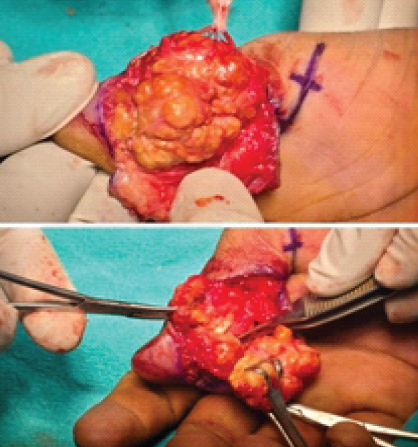
Figure 6: Intraoperative picture showing the excision of the tumor, isolation of the digital artery above, and flexor pollicis tendon underneath the tumor mass below.
Following tumor removal, the areas of bony erosion on the distal phalanx were treated with adjuvant chemical cauterization. An 88% phenol solution was applied to the bony bed for about a minute using a cotton-tipped applicator, followed by copious neutralization and irrigation with hydrogen peroxide and normal saline. This was done to ablate any microscopic residual tumor cells and reduce the risk of local recurrence. Hemostasis was achieved, and the wound was closed in layers (Fig. 7).

Figure 7: Hemostasis achieved and wound closure done.
Grossly, the excised specimen measured approximately 4.5 × 3.5 cm in aggregate (Fig. 8).

Figure 8: Gross specimen of tumor mass.
Histopathological examination remains the gold standard for diagnosis [7]. It demonstrated a tumor composed of mononuclear stromal cells, large multinucleated giant cells, and foamy macrophages. No mitosis or pleomorphism was observed (Fig. 9).
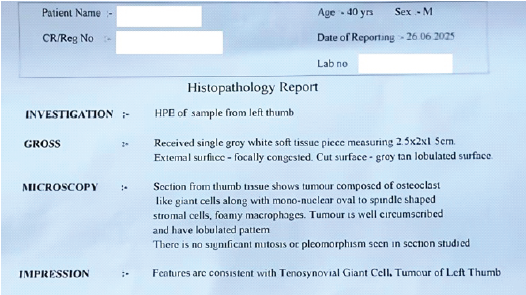
Figure 9: Histopathology report.
The patient’s post-operative course was uneventful. Sutures were removed at 2 weeks. At 4 months follow-up, the patient had significant improvement in ROM of the thumb with easy continuation of his occupational activities, normal grip, and no clinical or radiological signs of recurrence (Fig. 10).

Figure 10: Follow-up after 4 months.
This case presents a classic, albeit large TSGCT of the thumb with the important finding of bony erosion. Typically presenting as a painless, slow-growing mass, TSGCTs may be commonly overlooked by patients and thus present at later stages. The most significant challenge in managing TSGCT is its high local recurrence rate, which is often due to incomplete excision. The literature reports a wide range of local recurrence rates, from as low as 10% to as high as 50% [8,9]. The presence of bony erosion as seen in this case suggests a more locally aggressive tumor and increases the difficulty of achieving complete surgical clearance [10]. To address this, adjuvant therapies such as phenol can be employed. We chose to use intraoperative 88% phenol as a local chemical adjuvant. Phenol causes cell necrosis and is a simple, inexpensive, and effective method for ablating residual microscopic disease in the tumor bed, particularly in bony crevices that are difficult to curette mechanically. Its use as an adjuvant in bone tumor surgery, such as the giant cell tumor of bone, is well established, and its application in aggressive TSGCTs, while less documented, follows the same principle of reducing local recurrence[11]. Other options include external beam radiation therapy, but it carries significant long-term risks, including joint stiffness, skin necrosis, and secondary malignancy. More recently, systemic therapies such as CSF-1 inhibitors (e.g., pexidartinib) or tyrosine kinase inhibitors (e.g., imatinib) have been approved for severe unresectable cases, but these have potential systemic toxicity, including hepatotoxicity [12,13].
This case report demonstrates a large TSGCT of the thumb with bony erosion, where the combination of classic MRI findings and intra-operative findings guided a two-pronged treatment strategy – meticulous surgical excision and adjuvant phenol cauterization. This approach successfully managed the aggressive local nature of the tumor, resulting in an excellent functional outcome with no evidence of recurrence. Adjuvant phenol should be considered a viable tool for managing TSGCT cases with bony involvement.
In cases of large TSGCTs with bony erosion (scalloping), complete surgical excision supplemented with adjuvants such as phenol cauterization to the tumor bed is an effective strategy to minimize the high risk of local recurrence.
References
- 1. Stacchiotti S, Dufresne A, Palmerini E, Dürr HR, Schaefer IM, Woertler K et al. Tenosynovial giant cell tumour: A systematic review and meta-analysis of current practice and outcomes. Cancer Treat Rev 2022;102:102312. [Google Scholar] [PubMed]
- 2. Bravo M, Wana D, Lazar A. Tenosynovial giant cell tumor: A review of the literature and update on management. J Clin Orthop Trauma 2020;11:963-9. [Google Scholar] [PubMed]
- 3. Verspoor FG, Flanagan AM, Schreuder HW. The spectrum of tenosynovial giant cell tumor and pigmented villonodular synovitis: A systematic review and meta-analysis. JBJS Rev 2021;9:e20. [Google Scholar] [PubMed]
- 4. Mastboom MJ, Verspoor FG, Hanff DF, Gademan MGJ, Dijkstra PDS, Schreuder HWB, Bloem JL et al. Severity classification of tenosynovial giant cell tumours on MRI and its association with local recurrence. Eur Radiol 2019;29:1431-41. [Google Scholar] [PubMed]
- 5. Van Der Heijden L, Gibbons CL, Hassan AB, Kroep JR, Gelderblom H, van Rijswijk CS, Nout RA et al. A multidisciplinary approach to giant cell tumors of the bone: A review of the literature and a consensus statement from the European society for medical oncology (ESMO). Ann Oncol 2017;28:1890-902. [Google Scholar] [PubMed]
- 6. O’Donnell PW, Griffin AM, Eward WC, Ferguson P, Chung WP, Catton CN et al. Can curettage and phenol ablation successfully manage giant cell tumors of the bone with soft tissue extension? Clin Orthop Relat Res 2018;476:568-74. [Google Scholar] [PubMed]
- 7. Yadav S, Singhal S, Patel S, Jaiswal S, Mishra R. A rare case of giant-cell tumor of hand in a young male. Cureus 2022;14:e21408. [Google Scholar] [PubMed]
- 8. Müller DA, Beltrami G, Scoccianti G, Cuomo P, Totti F, Capanna R et al. The role of surgery and adjuvant therapy in the management of diffuse-type tenosynovial giant cell tumors of the extremities: A systematic review and meta-analysis. J Surg Oncol 2018;118:1010-22. [Google Scholar] [PubMed]
- 9. Gouin F, Noailles T, Localized and diffuse forms of tenosynovial giant cell tumor (formerly giant cell tumor of the tendon sheath and pigmented villonodular synovitis). Orthop Traumatol Surg Res. 2017 Feb;103(1S):S91-S97. doi: 10.1016/j.otsr.2016.11.002. Epub 2017 Jan 2. PMID: 28057477. [Google Scholar] [PubMed] [CrossRef]
- 10. Spierenburg G, Grimison P, Chevreau C, Randall RL, Thorpe WS, Houdek TM et al. Outcome after surgical treatment of recurrent tenosynovial giant cell tumor: A retrospective analysis from the tenosynovial giant cell tumor (TGCT) consortium. Eur J Surg Oncol 2022;48:1143-50. [Google Scholar] [PubMed]
- 11. Errani C, Ruggieri P, Asenzio MA, Toscano A, Colangeli S, Rimondi E, Rossi G, et al. Giant cell tumor of the extremity: A review of 349 cases from a single institution. Cancer Treat Rev 2018;62:1-12. [Google Scholar] [PubMed]
- 12. Tap WD, Gelderblom H, Palmerini E, van de Sande M, Qian M, Shuster DE et al. Long-term efficacy and safety of pexidartinib in patients with tenosynovial giant cell tumor: Final results of the ENLIVEN study. Lancet Oncol 2023;24:64-76. [Google Scholar] [PubMed]
- 13. Nakayama R, Matsumoto Y. The role of CSF1R inhibitors in the treatment of tenosynovial giant cell tumor. Cancers 2021;13:2675. [Google Scholar] [PubMed]