In the article, the author has described a novel technique for non-uniting fractures of the proximal pole of scaphoid using proximal pole of hamate as graft.
Dr. Ankit Kumar, Department of Orthopaedics, Rehabilitation and Research Centre, Dr. S.N. Medical College and Associated Group of Hospitals, Jodhpur, Rajasthan, India. E-mail: drankitkumar9472@gmail.com
Introduction: Scaphoid is the most common carpal to be fractured (60%), caused by fall on outstretched hand, and proximal pole fractures are difficult to manage due to the high risk of non-union and osteonecrosis due to retrograde blood supply. Conservative management of proximal pole fractures leads to high rates of non-union; hence, different surgical techniques have been devised to address bone loss and optimize vascularity at fracture site to promote healing, such as vascularized bone grafting (VBG) and non-VBG. We report the use of proximal hamate as a replacement arthroplasty in the context of proximal pole non-unions with collapse, bone loss, and/or osteonecrosis as an innovative approach.
Case Report: A 26-year-old Air Force personnel presented with left wrist pain and difficulty in movement and lifting. He had a fall on an outstretched hand causing a proximal scaphoid fracture, initially treated with Herbert screw fixation, resulting in non-union. A revision surgery with iliac crest bone grafting and Kirschner wire fixation was performed after 6 months, but non-union persisted.
Conclusion: This novel surgical technique of using proximal hamate autograft for reconstruction of osteonecrosis proximal pole of scaphoid has shown promising result with union within 10 weeks and good functional outcome with pain-free near full wrist arc
Keywords: Scaphoid, hamate, capitohamate ligament, non-union.
Scaphoid is the most common carpal to be fractured (60%), caused by fall on outstretched hand, with the mechanism being axial loading of the wrist on forced hyperextension and radial deviation [1]. The fractures of proximal pole of scaphoid can indeed be difficult to manage due to the high risk of non-union and osteonecrosis, due to 70–80% of its blood supply being retrograde from dorsal scaphoid branch of radial artery, which can lead to long-term issues such as carpal collapse [2]. The statistics from the recent meta-analysis highlight the considerable risk of non-union associated with non-operative treatment for acute proximal pole fractures, especially when there is displacement [3]. Hence, different surgical techniques have been devised to address bone loss and optimize vascularity at the fracture site to promote healing, such as vascularized bone grafting (VBG) and non-VBG (NVBG). Proximal pole fractures are usually addressed by NVBG as they maintain their vascularity and have successful union rates between 36 and 89% [4], with the graft donor site being iliac crests, distal radius and ribs autograft [5,6,7,8,9,10]. In follow-up cases that demonstrate failed fixations, non-union, osteonecrosis, VBG has shown to give better union rates than NVBG, union rates being documented in the range of 27–100% [4]. VBGs could either be pedicled like 1,2 intercompartmental supraretinal dorsal radius graft [11] and volar carpal artery pedicled pronator quadratus graft [12] or free like metatarsal grafts, medial femoral condyle/trochlear grafts [13,14,15]. Elhassan et al. [16] proposal of using the proximal hamate as a replacement arthroplasty in the context of proximal pole non-unions with collapse, bone loss, and/or osteonecrosis is an innovative approach. The use of a non-vascularized osteochondral autograft that retains its attached volar capitohamate (CH) ligament offers several advantages. It provides a local solution for osteochondral reconstruction, minimizes donor site morbidity, and utilizes the CH ligament for scapholunate (SL) ligament reconstruction. This approach represents an important development in addressing complex proximal pole fractures and offers potential benefits over traditional graft choices.
A 26-year-old Airforce personnel presented with complaints of pain left wrist and difficulty in movement and lifting objects to our outpatient department. The patient had a history of a fall on an outstretched hand leading to fracture of proximal pole of scaphoid, which was managed primarily by internal fixation using Herbert screw (Fig. 1), which resulted in non-union.
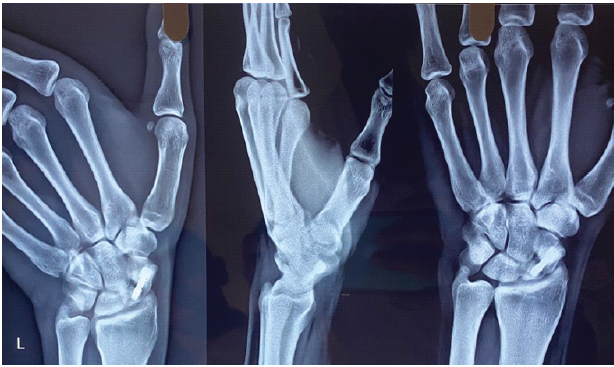
Figure 1: Pre-operative radiograph showing no signs of bony union.
It was followed by a revision surgery after 6 months, in which surface bone grafting taken from the opposite iliac crest was done along with fixation with Kirschner wire, again resulting in non-union.
Pre-operative clinical examination
A healed scar approximately 5–6 cm long is present on volar aspect of wrist. The range of motion at wrist was limited with painless arc of wrist flexion extension only being 50-60° with weak finger grip strength. After radiological evaluation, the patient was planned for bone grafting using NVBG from ipsilateral distal end radius.
Surgical technique
Patient positioned supine on OT table with arm on side table and under unsterile tourniquet with pressure 220 mm of Hg skin incision taken over previous incision site under all aseptic precautions, after exposing the fracture site gross non-union (Fig. 2) along with osteomalacia of proximal pole of scaphoid (Fig. 3) and large bone defect was found which could not be addressed with simple bone grafting.

Figure 2: Clinical non-union site.
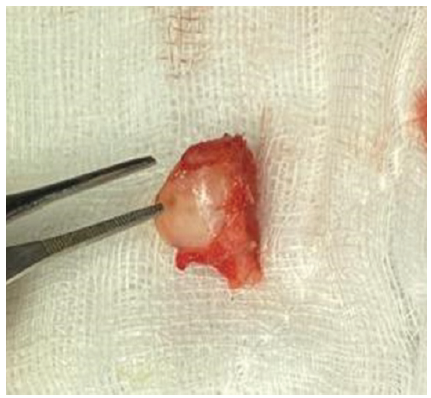
Figure 3: Proximal Hamate autograft.
Intraoperative decision of using proximal pole of hamate graft was taken after obtaining due consent. Another incision was given over the dorsal aspect of hand over hamate 3–4 cm in length, the proximal pole of hamate was harvested along with preserving CH ligament and prepared (Fig. 4). At the same time proximal pole of scaphoid was excised and donor site prepared (Fig. 5) then reconstruction was done with proximal hamate graft after flipping it 180° along with reconstruction of SL ligament using CH ligament and cancellous bone graft from distal end radius was compacted in gaps and retrograde fixation done with 3 Kirschner wire (Fig. 6) and their position checked under C-arm in volar and dorsal aspect (Fig. 7). A thumb spica slab was applied postoperatively and kept for 3 month.
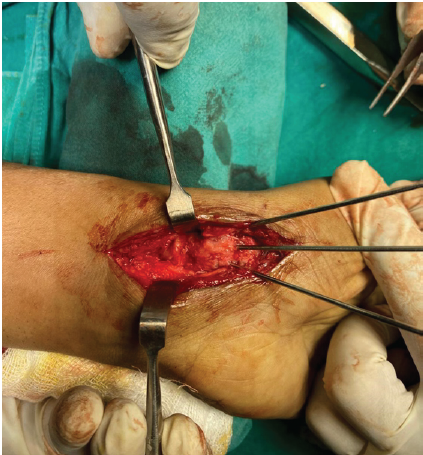
Figure 4: Intraoperative picture of graft fixed with k-wires.
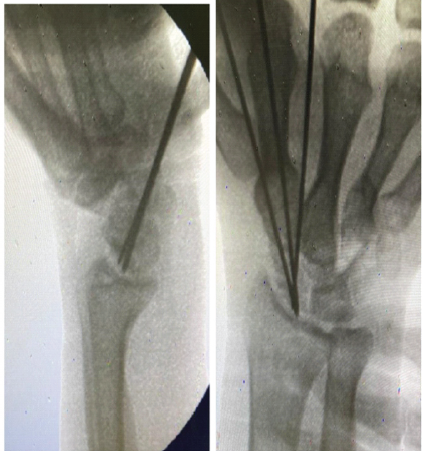
Figure 5: Fluoroscopy image confirming K-wire position.

Figure 6: Radiograph showing 10 weeks and 3 years follow- up with definitive signs of bony union.
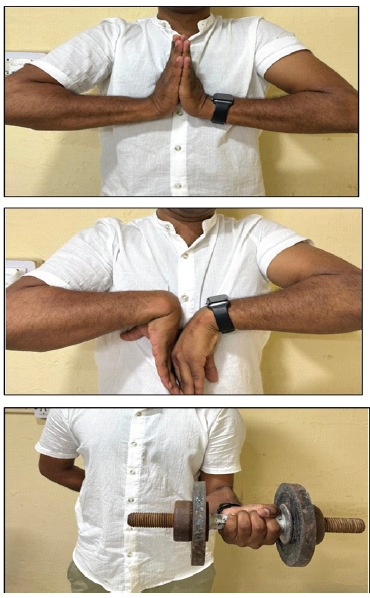
Figure 7: Full range of pain-free motion after bony union.
Follow-up after 12 weeks and 3 years postoperatively showed union of the fracture after which Kirschner wires were removed, the slab was discontinued, and physiotherapy was initiated. Post-operative clinical examination (at 12 months). Pain-free arc of wrist flexion extension up to 160–170° with complete pronation and supination, finger grip strength comparable to non-operated hand.
Achieving surgical union of the proximal pole of the scaphoid can be particularly challenging, especially in cases of unsalvageable fragmentation, carpal collapse, or avascular necrosis (AVN). Various surgical techniques have been developed to address these issues, notably vascularized bone graftsVBGs) and NVBGs. Current literature suggests that VBGs yield better proximal pole union rates compared NVs in such difficult circumstances. A meta-analysis conducted by Merrell et al. [17] reported that the union rate following NVBG use for non-union and proximal pole AVN was 47%, while VBGs achieved a significantly higher union rate of 88%. Goldberg et al. [18] proposed that the success of VBGs may be attributed higher rates of osteocyte survival, which helps reduce creeping substitution and graft resorption. However, despite the promising results associated with VBGs, their outcomes can be quite variable. Factors influencing these outcomes include the type of graft, the size of the proximal pole, and the presence of scaphoid collapse or AVN. In clinical practice, considerations such as the graft selection and surgical technique play a crucial role in maximizing the chances of successful union of the proximal pole in complex cases.
The use of a proximal hamate osteochondral autograft offers a viable and effective alternative for managing complex proximal pole scaphoid non-unions, especially in cases with bone loss, collapse, or AVN. It provides anatomical and biomechanical compatibility, avoids donor site morbidity, and facilitates SL ligament reconstruction. This technique shows promising functional and radiological outcomes without requiring microvascular expertise, making it a practical solution in challenging cases.
Scaphoid is the most common carpal bone to be fractured and is notorious to heal due to its retrograde blood supply often resulting in non-union even after repeated procedures. A proximal hamate autograft used for reconstruction of the proximal pole of scaphoid has shown promising results in this case and should be considered as a promising treatment options when dealing with non-union of scaphoid.
References
- 1. Clementson M, Björkman A, Thomsen NO. Acute scaphoid fractures: Guidelines for diagnosis and treatment. EFORT Open Rev 2020;5:96-103. [Google Scholar] [PubMed]
- 2. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg Am 1980;5:508-13. [Google Scholar] [PubMed]
- 3. Eastley N, Singh H, Dias JJ, Taub N. Union rates after proximal scaphoid fractures; meta-analyses and review of available evidence. J Hand Surg Eur Vol 2013;38:888-97. [Google Scholar] [PubMed]
- 4. Steinmann SP, Adams JE. Scaphoid fractures and nonunions: Diagnosis and treatment. J Orthop Sci 2006;11:424-31. [Google Scholar] [PubMed]
- 5. Robbins RR, Ridge O, Carter PR. Iliac crest bone grafting and Herbert screw fixation of nonunions of the scaphoid with avascular proximal poles. J Hand Surg Am 1995;20:818-31. [Google Scholar] [PubMed]
- 6. Shah J, Jones WA. Factors affecting the outcome in 50 cases of scaphoid nonunion treated with Herbert screw fixation. J Hand Surg Br 1998;23:680-5. [Google Scholar] [PubMed]
- 7. Sandow MJ. Costo-osteochondral grafts in the wrist. Tech Hand Up Extrem Surg 2001;5:165-72. [Google Scholar] [PubMed]
- 8. Veitch S, Blake SM, David H. Proximal scaphoid rib graft arthroplasty. J Bone Joint Surg Br 2007;89:196-201. [Google Scholar] [PubMed]
- 9. Lanzetta M. Scaphoid reconstruction by a free vascularized osteochondral graft from the rib: A case report. Microsurgery 2009;29:420-4. [Google Scholar] [PubMed]
- 10. Yao J, Read B, Hentz VR. The fragmented proximal pole scaphoid nonunion treated with rib autograft: Case series and review of the literature. J Hand Surg Am 2013;38:2188-92. [Google Scholar] [PubMed]
- 11. Zaidemberg C, Siebert JW, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg Am 1991;16:474-8. [Google Scholar] [PubMed]
- 12. Kuhlmann JN, Mimoun M, Boabighi A, Baux S. Vascularized bone graft pedicled on the volar carpal artery for non-union of the scaphoid. J Hand Surg Br 1987;12:203-10. [Google Scholar] [PubMed]
- 13. Del Pinal F, Klausmeyer M, Moraleda E, De Piero GH, Galindo C, Studer A, et al. Vascularized graft from the metatarsal base for reconstructing major osteochondral distal radius defects. J Hand Surg Am 2013;38:1883-95. [Google Scholar] [PubMed]
- 14. Kazmers NH, Thibaudeau S, Levin LS. A scapholunate ligament-sparing technique utilizing the medial femoral condyle corticocancellous free flap to reconstruct scaphoid nonunions with proximal pole avascular necrosis. J Hand Surg Am 2016;41:e309-15. [Google Scholar] [PubMed]
- 15. Burger HK, Windhofer C, Gaggl AJ, Higgins JP. Vascularized medial femoral trochlea osteocartilaginous flap reconstruction of proximal pole scaphoid nonunions. J Hand Surg Am 2013;38:690-700. [Google Scholar] [PubMed]
- 16. Elhassan B, Noureldin M, Kakar S. Proximal scaphoid pole reconstruction utilizing ipsilateral proximal hamate autograft. Hand (N Y) 2016;11:495-9. [Google Scholar] [PubMed]
- 17. Merrell GA, Wolfe SW, Slade JF 3rd. Treatment of scaphoid nonunions: Quantitative meta-analysis of the literature. J Hand Surg Am 2002;27:685-91. [Google Scholar] [PubMed]
- 18. Goldberg VM, Shaffer JW, Field G, Davy DT. Biology of vascularized bone grafts. Orthop Clin North Am 1987;18:197-205. [Google Scholar] [PubMed]