Accurate bone cuts using robotic assistance alone are insufficient for stable TKA; continuous dynamic robotic gap tracking enables objective, real-time soft-tissue balance assessment across motion, detecting subtle instabilities and supporting more precise, personalised, and reproducible knee arthroplasty outcomes.
Dr. Adarsh Krishna K Bhat, Department of Orthopaedic Surgery, Apollo Hospitals, Bannerghatta Road, Bengaluru - 560076, Karnataka, India. E-mail: adarshbhat118@gmail.com
Introduction: Mid-flexion instability and variable gap balancing across the range of motion remain key challenges in achieving optimal outcomes in total knee arthroplasty (TKA). Different robotic systems, as well as traditional methods of gap assessment, are static and subjective, often failing to detect subtle instabilities intraoperatively. We describe a novel technical approach using a computed tomography-based Cuvis joint robotic system to perform real-time, dynamic assessment of coronal plane stability throughout knee motion.
Technique: Using the Cuvis joint robotic system, intraoperative gap assessment was performed in a dynamic fashion during TKA. The robot enabled continuous quantification of medial and lateral gaps across the entire arc of motion (0–120°/maximum possible range) after putting in the trails prosthesis, both in neutral alignment and under controlled valgus and varus stress. The data-driven interface allowed for precise numerical evaluation of joint stability and identification of any mid-flexion or range-dependent instabilities.
Results: The robotic-assisted method provided comprehensive, reproducible, and objective stability profiles, aiding intraoperative decision-making. Adjustments in soft-tissue balancing and component positioning were guided by quantitative feedback, allowing tailored correction of asymmetric or unstable gaps.
Conclusion: Dynamic, robot-assisted intraoperative assessment using the Cuvis joint system offers a promising advancement in TKA, improving the precision of coronal plane balancing across the full range of motion. This technique enhances the surgeon’s ability to detect and address instabilities that may be missed with static assessments.
Keywords: Robotic-assisted knee arthroplasty, mid flexion instability, cuvis, knee arthroplasty.
Total knee arthroplasty (TKA) outcomes continue to evolve with refinements in implant design, alignment philosophies, and surgical technologies. However, despite these advances, soft-tissue imbalance – particularly mid-flexion instability – remains a common contributor to pain, instability, and early revision. Traditional gap-balancing tools, such as laminar spreaders, spacer blocks, tensioners, and manual stress testing, assess the knee at discrete angles and depend heavily on surgeon interpretation. These static methods provide only partial insight into joint behavior and may fail to identify subtle instabilities that occur during dynamic motion. Robotic systems have been shown to improve accuracy in bone resection, limb alignment, and component positioning [1,2,3]. Early robotic platforms demonstrated improved precision compared with manual instrumentation [1]. More recent studies have highlighted enhanced patient satisfaction and alignment accuracy with functional alignment and advanced robotic balancing algorithms [2,4,5,6,7]. However, most systems still assess soft-tissue balance at only a few discrete positions. The Cuvis joint robotic system incorporates a dynamic gap-tracking function that continuously monitors medial and lateral compartment behavior through the full flexion arc and presents the data in numerical form, which many other robotic systems don’t. This allows the surgeon to visualize real-time changes, detect mid-flexion instability, identify non-physiological asymmetry, and adjust balancing strategies accordingly. This technical note outlines the detailed method for incorporating this assessment into the routine TKA workflow.
Preoperative planning
All patients underwent a standard computed tomography-based preoperative protocol. The robotic system generated a three-dimensional model of the femur and tibia, allowing precise planning of:
- Bone resections
- Component alignment
- Joint-line restoration
- Soft-tissue tension expectations
Preoperative planning was reviewed and refined as required to achieve the desired alignment as per functional alignment principles.
Patient positioning and exposure
The patient was positioned supine with the leg supported on mayo leg kit with a lateral post to allow a full range of flexion for dynamic assessment (Fig. 1). A standard medial parapatellar approach was used. After joint exposure, reflective trackers were attached, and anatomical landmarks were accurately registered.
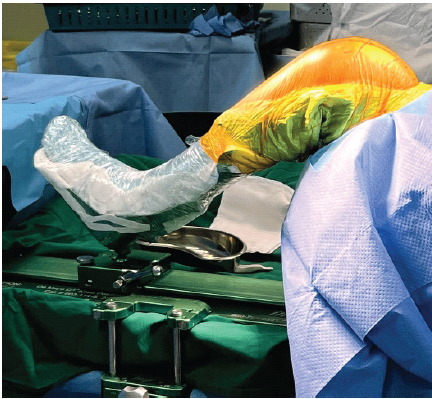
Figure 1: Leg supported on De Mayo leg kit.
Robotic bone preparation
Once registration was validated, the dynamic gap assessment protocol was followed, and once the component sizes, mediolateral gap balancing was confirmed, and then bone resections were executed using the fully automatic burr-based Cuvis robotic system. Post-bony resections, the precision was confirmed, and then trial components matching the planned sizes were inserted. Post-inserting the trial components, dynamic gap assessment was again repeated to look for any imbalances, which could be fine-tuned before final cementation.
Dynamic gap assessment protocol
Dynamic gap assessment was first performed initially after removing osteophytes, minimal soft tissue release, and performing adjustments in component positioning to achieve the desired alignment and balanced mediolateral gaps. These are done before going ahead with bony resections. Second, it is done post-resection and after inserting the trial components. The steps involved are
- Neutral range-of-motion assessment
- 0° extension → 120° flexion/full range possible, And back to extension.
Throughout the range of motion, the system recorded:
- Medial compartment gap
- Lateral compartment gap
- Limb alignment
- Varus–valgus moment contributions.
These data were presented numerically by the system throughout the range.
- Varus stress assessment
A controlled varus stress was applied manually, and the robot quantified lateral opening patterns across the range. This provided insight into:
- Lateral ligament elasticity
- Laxity patterns
- Stress-dependent instability
- Valgus stress assessment
A similar maneuver was performed in valgus stress to evaluate medial structures. The system displayed:
- Medial gap widening
- Behavior of the medial collateral ligament (MCL)
- Consistency of tension through flexion.
Interpretation and intraoperative adjustments
Identifying the problems
The dynamic numerical data of the gaps frequently revealed the issues that are not apparent on static testing. The intends gaps are kept at 10 mm mediolaterally with a plan to finally insert a 9 mm or 10 mm polyethylene insert with functional alignment principles.
- Mid-flexion instability (30–60°) characterized by sudden increases in both medial and lateral gap width.
-
- Managed with flexing the femoral component (multi radii femoral component), adjusting the extension gap, and using a thicker insert or modification of tibial slope.
- Asymmetric flexion behavior
-
- Lateral gap widening in flexion suggested excessive LCL laxity
- Medial tightness in flexion indicated over-tensioned MCL.
- Deep-flexion tightness (>90°)
-
- Identified by a rapid reduction in gap width
- Corrected by adjusting the posterior condylar offset or femoral posterior cut.
- Extension–flexion imbalance
-
- Differing gap magnitudes between 0° and 90° required selective anterior/posterior soft-tissue releases or minimal recuts.
Real-time correction cycle
After each correction, the dynamic scan was repeated. This iterative process continued until the medial and lateral gaps were demonstrated:
- Smooth progression
- Physiological tension pattern
- Equal to near equal mediolateral gaps.
This approach provided numerically quantifiable confirmation of stability before and after bony resections rather than relying solely on tactile feedback.
- Video 1: Dynamic assessment -limb video after osteophyte removal and component adjustments before bony cuts
- Video 2: Dynamic assessment -limb video after trial component insertion
- Video 3: Numerical visualization of the mediolateral gaps (9–10 mm without imbalances) and limb alignment through the arc of motion.
Use of dynamic robotic-assisted assessment has provided several consistent advantages:
- Reproducible objective data
Unlike manual assessment, which varies between surgeons, the robotic data were consistent and quantifiable.
- Early identification of subtle instability
Mid-flexion instability – often missed by traditional tools – was routinely detected.
- Improved precision in soft-tissue balancing
Surgeons could target specific structures or modify component positioning based on numerical data, particularly in complex deformities.
- Enhanced confidence in final balancing
Repeating dynamic scans allowed confirmation that adjustments resulted in predictable improvements.
Although long-term outcome studies are needed, the experience aligns with reports showing improved early recovery, limb alignment accuracy, and reduced outliers in robotic TKA [2-7].
Instability is one of the leading causes of revision TKA, accounting for a significant percentage of reoperations [8-10]. Mid-flexion instability, in particular, may be subtle during static intraoperative testing and is influenced by posterior femoral condyle geometry, MCL isometry, component rotation, and tibial slope. Robotic assistance has greatly improved precision in bone resection and alignment [1,2,3,4]. Gustke and Simon demonstrated superior results using robotic-assisted functional alignment and balancing compared with manual TKA at 2-year follow-up [2]. Matsumoto et al. additionally demonstrated improved tibial alignment accuracy and early functional recovery with image-free robotic TKA [3]. However, even the most accurate bone cuts do not guarantee balanced soft tissues. The key novelty of the present technique is the continuous, dynamic assessment of soft-tissue behavior throughout the entire motion arc. The ability to visualize this behavior numerically and balance it accurately, may reduce soft-tissue errors, especially in valgus knees, post-traumatic deformity, and cases requiring collateral releases. The technique described here integrates seamlessly into the workflow and requires minimal additional operative time once mastered.
Dynamic robotic-assisted intraoperative gap assessment using the Cuvis joint system offers a comprehensive and objective method for evaluating coronal plane stability across the full range of motion. By identifying subtle instabilities that static techniques frequently overlook, this method enables more precise balancing and may improve postoperative outcomes. Incorporating dynamic stability analysis into routine TKA represents a promising next step in personalized, data-driven arthroplasty.
Dynamic robotic-assisted gap assessment during TKA allows objective, real-time evaluation of soft-tissue balance throughout the full range of motion, enabling early detection and correction of mid-flexion and subtle coronal instabilities that are often missed with static techniques. Integrating this approach into routine TKA can improve intraoperative decision-making, enhance balancing precision, and may reduce postoperative instability and revision risk.
References
- 1. Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res. 2007;464:111–6. [Google Scholar] [PubMed]
- 2. Gustke KA, Simon P. Two-year outcome comparison of a matched set of total knee arthroplasties performed with robotic-arm-assisted functional alignment balancing or manual instrument-assisted adjusted mechanical alignment. J Arthroplasty. 2025;40(7):S116-122. [Google Scholar] [PubMed]
- 3. Matsumoto K, Ishimaru D, Sohmiya K, Terabayashi N. Benefits of image-free robotic-assisted total knee arthroplasty in postoperative recovery and tibial alignment accuracy. Cureus. 2025;17(9):e92044. [Google Scholar] [PubMed]
- 4. Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic technology in TKA improves alignment and early functional outcomes: a systematic review. Bone Joint J. 2021;103-B:901–10. [Google Scholar] [PubMed]
- 5. Marchand RC, Sodhi N, Anis HK. Robotic-arm assisted total knee arthroplasty: an update on clinical outcomes. J Knee Surg. 2020;33(1):102–7. [Google Scholar] [PubMed]
- 6. T RK, Bhat AKK, Biradar N, Patil AR, Mangsuli K, Patil A. Gap Balancing Technique With Functional Alignment in Total Knee Arthroplasty Using the Cuvis Joint Robotic System: Surgical Technique and Functional Outcome. Cureus. 2025 Feb 12;17(2):e78914. doi: 10.7759/cureus.78914. [Google Scholar] [PubMed] [CrossRef]
- 7. Rajashekhar KT, Patil AR, Bhat AKK, Bagrecha A. Achieving Accuracy and Gap Balancing in Fully Autonomous Robotic-Assisted Total Knee Arthroplasty with Functional Alignment in Valgus Knee Deformity. J Orthop Case Rep. 2025 Nov;15(11):265-273. doi: 10.13107/jocr.2025.v15.i11.6378. [Google Scholar] [PubMed] [CrossRef]
- 8. Dennis DA. Evaluation of painful total knee arthroplasty. J Arthroplasty. 2004;19(4 Suppl 1):35–40. [Google Scholar] [PubMed]
- 9. Al-Jabri, T., Brivio, A., Maffulli, N. Management of instability after primary total knee arthroplasty: an evidence-based review. J Orthop Surg Res 16, 729 (2021). https://doi.org/10.1186/s13018-021-02878-5 [Google Scholar] [PubMed] [CrossRef]
- 10. Chang MJ, Lim H, Lee NR, Moon YW. Diagnosis, causes and treatments of instability following total knee arthroplasty. Knee Surg Relat Res. 2014 Jun;26(2):61-7. doi: 10.5792/ksrr.2014.26.2.61. Epub 2014 May 30. PMID: 24944970; PMCID: PMC4061408. [Google Scholar] [PubMed] [CrossRef]