[box type=”bio”] What to Learn from this Article?[/box]
A salvage treatment of badly injured and seemingly unsalvageable elbow is possible with a judicious use of mega prosthesis of the elbow.
Case Report | Volume 6 | Issue 2 | JOCR April-June 2016 | Page 46-49 | Raju Vaishya, Vipul Vijay, Ram Sagar Pandit, Amit K Agarwal DOI: 10.13107/jocr.2250-0685.428
Authors: Raju Vaishya[1], Vipul Vijay[1], Ram Sagar Pandit[1], Amit K Agarwal[1]
[1] Department of Orthopaedics, Indraprastha, Apollo Hospitals, Sarita Vihar, New Delhi, India.
Address of Correspondence
Dr. (Prof) Raju Vaishya,
Senior Consultant, Room no 1210, Department of Orthopaedics, Indraprastha Apollo Hospitals, Sarita Vihar, New Delhi – 110076, India.
E-mail: raju.vaishya@gmail.com
Abstract
Introduction: Fractures of the distal humerus are a rare entity accounting for approximately 2% of the humeral fractures. Non union of the distal humerus is further rare and poses a major challenge. These fractures usually respond to open reduction and bone grafting but some may fail multiple surgical attempts at union and hence are labelled as “resistant” non union. We report a case of resistant non union of the distal humerus which was managed by total elbow arthroplasty.
Case Presentation: A 49-year-old male presented to the out patient department with history of a compound comminuted fracture of the distal end of the humerus approximately 25 years back. The fracture was treated with multiple debridements and plaster cast application. There was involvement of the radial and the ulnar nerves as well. The patient continued to use the disabled upper limb with severe difficulties in activities of daily living (ADL). The patient finally presented to us for regaining some range of motion and improvement in his ADL. In view of the grossly distorted anatomy, bone loss and chronic nature of the problem, patient was offered total elbow arthroplasty. The Wadsworth extensile posterior approach was used for exposure of the non union site. The fragments were found to be small, osteoporotic and deformed. In view of the distorted anatomy, the elbow was finally salvaged with mega-prosthetic replacement of the elbow. Posterior elbow splint was used for 2 weeks and active as well as passive range of motion was started after that. The post-operative Mayo elbow score improved from 50 to 80 and the patient was able to achieve a range of motion from 10 degrees to 110 degrees.
Conclusion: Total elbow arthroplasty can be used as a salvage procedure for resistant non union of the elbow with failed multiple failed attempts at union. It can also be used as a definitive procedure for severely distorted non union with massive bone loss with satisfactory functional results.
Keywords: megaprosthetic replacement, distal humerusnon union.
Introduction
Amongst all the humeral fractures, only 2% are located in distal humerus and the non-union of these fractures is rare and accounts for about 2 % [1]. Non-union of distal humerus is often difficult and challenging to treat surgically. Open reduction and internal fixation (ORIF) using locking plates and bone grafting is the treatment of choice but still the reoperation rates are reportedly high [1]. Resistant non-union is considered when the union of a fracture does not occur even after multiple failed surgical approaches and is associated with a bone gap, poor bone stock and ankylosis of the joint. Total elbow arthroplasty (TEA) using standard hinged prosthesis has been used, where there is enough bone stock in the distal humerus [9]. However, when the resistant non-union is associated with significant bone loss or poor bone stock then mega prosthetic replacement may be a good alternative to repeated internal fixation in these types of resistant non-union. Mega prosthetic replacement of the joints has been reported mainly for neoplastic conditions but we have the experience of using it for the resistant non-union of the distal femoral fracture with poor bone stock and severe joint damage [2]. We present a case of neglected resistant non-union of distal humerus in a patient with bomb blast injury managed by mega prosthetic replacement of the elbow. To the best of our knowledge, the use of mega prosthesis for resistant non-union of the distal humerus has not been reported before in the literature.
Case Report
A 49-year-old male presented with a history of bomb blast injury to his left elbow 25 years back, when he had sustained an open and comminuted fracture of left distal humerus with extension into the elbow joint. The injury was treated with wound debridement and cast application for 6 weeks. Distal humerus progressed to atrophic non-union, with severe deformity and stiffness of the elbow. He also had partial involvement of radial and ulnar nerves with stiffness and deformities of the fingers of the left hand. He presented to us for correction of the elbow deformity and to gain reasonable elbow and hand function.
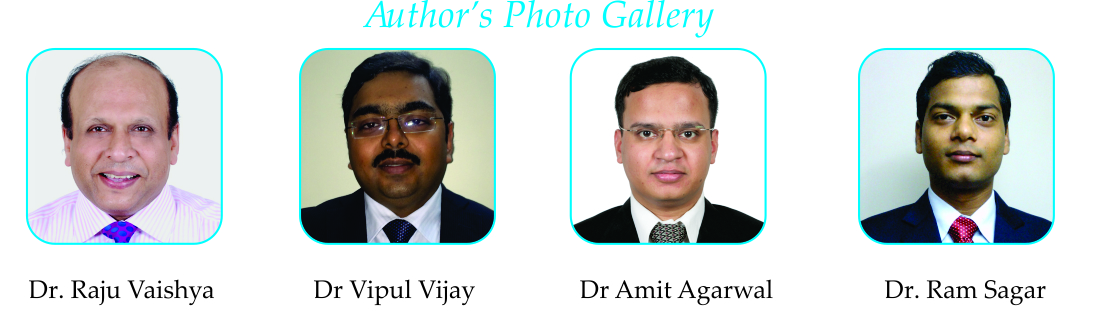
On local examination, there were multiple scars present medially, laterally and posteriorly around his left elbow suggestive of healed wounds by secondary intention after compound injury. There was fixed flexion deformity of the elbow of 900 with further flexion up to 120 degree was possible (Fig. 1a, 1b). There was partial sensory loss in the little and ring fingers and the muscle power (as per MRC grading) of the finger flexors was 3/5; wrist and those of elbow flexors was 2/5. The motor power of left fingers, wrist and elbow extensors were 1/5. Plain radiographs revealed atrophic non-union of the supracondylar fracture along with the deformity at the distal humerus due to mal-united distal humeral fracture (Fig. 2a, 2b). CT scan confirmed these radiographic findings and demonstrated a significant gap at the fracture site with grossly rotated distal humeral condylar fragments and marked disuse osteopenia. In view of grossly distorted anatomy of the distal humerus, poor bone stock, bone gap at the non-united fracture, severe elbow deformity and stiffness we preferred to go for a mega prosthetic replacement of the left elbow. Under general anaesthesia, elbow was approached posteriorly by ‘Wadsworth approach’ and the fracture site was exposed. Severe fibrosis was encountered between the fractured ends of the bone, which was excised. The distal humeral condylar fragments were found to be grossly mal-positioned, osteoporosed, destructed and were not amenable to osteosynthesis or conventional total elbow replacement. Hence, the distal humeral bone fragments were excised, leading to a large bone gap at the elbow. This gap was reconstructed by using elbow mega prosthesis. Preparation for mega prosthetic replacement was done by reaming the humeral and ulnar shafts. Cemented titanium prosthesis (XLO Tm) was used for reconstruction, with ulnar stem of 132 mm and humeral stem of 175 mm length. The implant had eyes in the ulnar component for the attachment of the triceps tendon. Common flexor tendons were attached on the medial side and the common extensor tendons were attached on lateral side of triceps tendon and finally the combined tendinous complex was attached at the eye of the prosthesis with the help of non-absorbable polyester suture (Ethibond™ No. 5). Intra operatively, we could achieve good correction of the elbow deformity (with ROM of 10-1500) with stable elbow joint. The patient was given i.v. third generation cephalosporin and aminoglycoside for a period of three days post operatively. The antibiotics were shifted to oral at the time of discharge and were continued for a period of two weeks till suture removal. The limb was kept in a splint for 2 weeks followed by physical therapy to regain the movements and function of the elbow and hand (Fig. 3a, 3b). The post-operative recovery was satisfactory and uneventful. Post-operative X-ray showed good placement of the prosthesis with adequate cementation (Fig. 4a, 4b). At 12 months follow up, the the patient had significant improvement in the post-operative Mayo elbow score of 80 compared to pre-operative score of only 50. The patient could now do many of his activities of daily living with left hand, which were not possible before, apart from significant improvement in the cosmetic appearance.
Discussion
Non-union of fractures of the distal humerus produces significant functional disability due to marked instability around the elbow joint [3]. Surgery is needed to stabilize the non-union site so that the joint can be mobilized. [4, 5, 6]. The proximity of the non-union to the elbow leads to movement at the site of the non-union and subsequently to failure of fixation in some cases after osteosynthesis. There are variations in the ORIF of distal humerus non-union, but with variable success rates [7].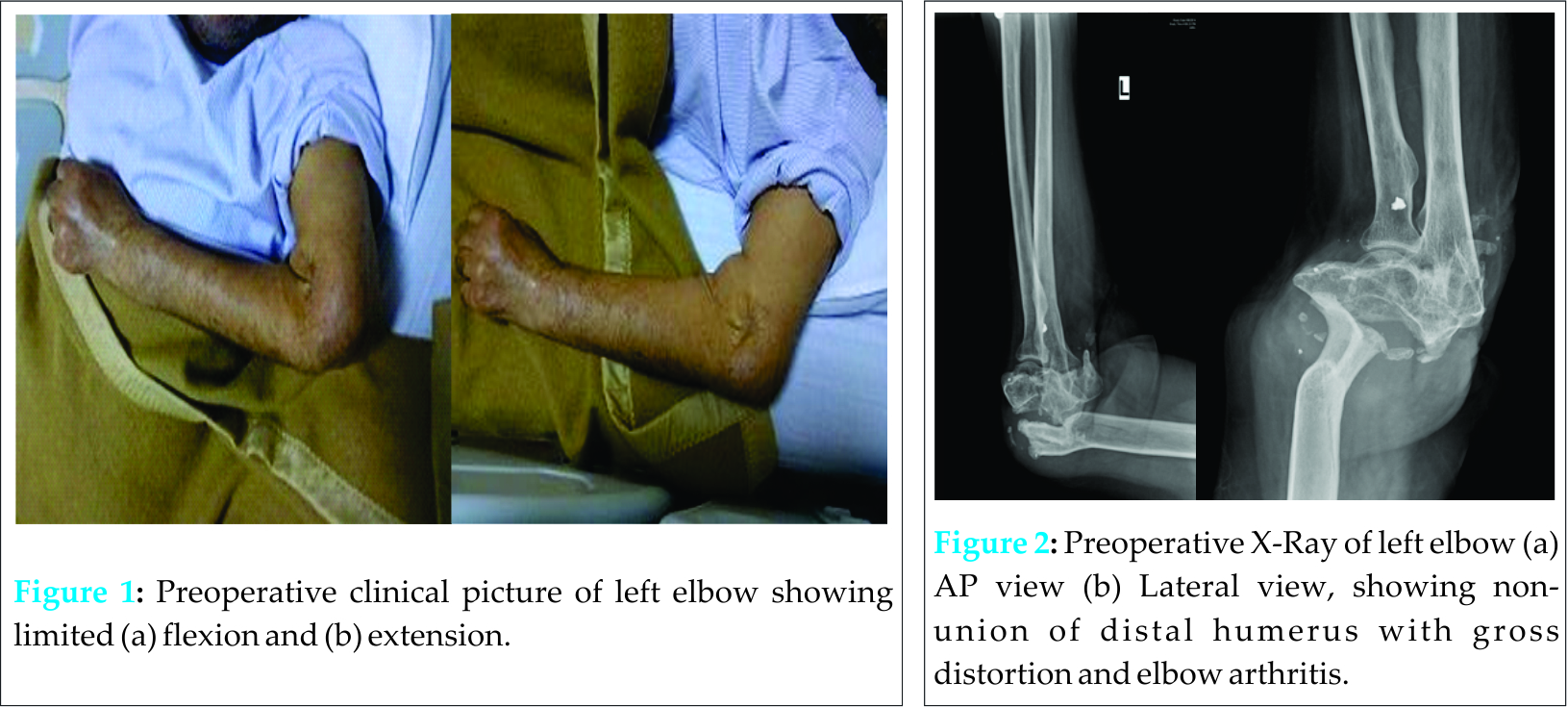
Failed osteosynthesis with non-union and significant bone loss can be managed with elbow fusion and total elbow arthroplasty. Elbow fusion can be considered as an option in heavy manual labours who need a painless fixed joint. The advantages of using a total elbow replacement is the possibility of achieving a painless mobile joint. Pros and cons of both the options were discussed with the patient who insisted on having a mobile elbow. Total elbow arthroplasty (TEA) has been reported to provide satisfactory results in several studies of well selected patients. Figgie et al [4] reported a series of 14 patients of TEA, where at an average follow-up of 5 years, the elbow score improved from 17 to 84 points. There were three failures secondary to dislocation, deep infection, and humeral component loosening. Morrey and Adams [8] reviewed 36 middle aged patients who underwent TEA with a mean follow-up of 4 years and reported satisfactory results in 86% of the patients. The Mayo Clinic experience with TEA for distal humerus resistant non-union has been updated recently [9], in 92 consecutively performed procedures. These patients were reviewed at a mean follow-up of 6.5 years with an average age of 65 years at the time of TEA. Before surgical intervention, 86% of the patients complained of moderate or severe pain. On follow-up, 79% of the patients had significant improvement in their pain score. Joint stability was restored in all patients, including nine with a grossly flail elbow. At latest visit, 85% of the patients were satisfied with their results. The risk of implant failure was increased in patients younger than 65-year-old, with prior surgical intervention, and a history of infection.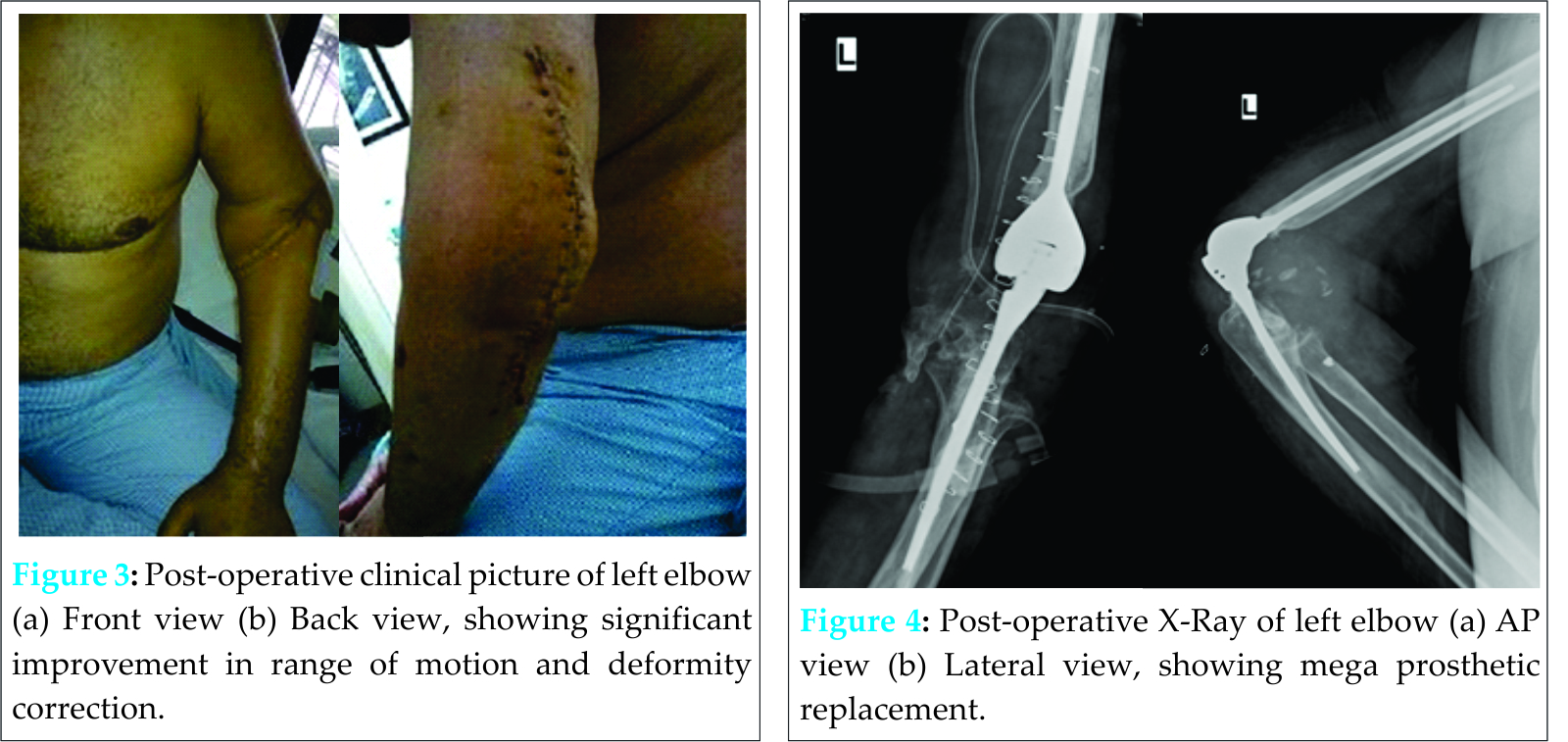
Some concerns have been raised about the effect of humeral condyle resection on elbow and forearm strength. However, McKee et al [10] reported on 32 patients who had undergone TEA with preservation (16 cases) or resection (16 cases) of the humeral condyles. Between both the groups, there were no statistically significant differences in elbow range of motion, forearm pronation and supination, or hand grip strength. According to the Mayo elbow performance score, both these groups also had similar final outcome. None of the reported series of TEA for resistant non-union of distal humerus have used mega prosthesis in their publications. We have had successful but solitary experience of using the mega prosthesis of the elbow for non-tumorous condition and would recommend its use in patients with resistant non-union of the distal humerus with secondary elbow arthritis, distorted anatomy and poor bone stock in middle to elderly aged person, where there are no other good options available for restoring the stability and function of the elbow. The use of mega prosthesis for such challenging situation provides single stage and definitive solution. The planning for a total elbow replacement starts with a detailed examination of the neuro-vascular status of the limb, along with the skin condition. The scars of any previous surgery should be carefully assessed before planning the new incision. The choice of the approach lies with the surgeon. We found the Wadsworth approach to be very useful in getting an adequate exposure to the elbow joint. Intra-operatively, care must be taken to identify and protect the ulnar nerve. This usually needs a complete exploration of the ulnar nerve along its course, before starting bone preparation. Any loose and fractured fragments are excised and the bone preserved, as it can be used as bone graft later. Extreme care should be taken while preparation of the ulna as in old age, the osteoporotic bone may undergo pathological fracture while preparation and manipulation. Trial implant should be assessed to look for any possible impingement from osteophytes during the complete flexion-extension arc. Good cementing technique is needed for achieving a good cement bone interface for a stable and long lasting prosthesis. The re-attachment of the triceps tendon should ideally be done with intraosseus sutures. Due to severe bone loss in the present case, we used the holes in the implant for re-attachment of the triceps tendon. Post-operative course of i.v. antibiotics would depend on the primary cause of the elbow arthritis. In cases of infectious arthritis, post operative i.v. antibiotics may need to be continued for a longer duration. Good rehabilitation protocol and patient compliance is needed to achieve a fair functional result. Total elbow replacement has been used in the various causes of arthritis of the elbow, its use in cases of resistant non union with severe bone loss is described here. The improvement in quality of life by the improved elbow function in these types of patients clearly outweighs the potential risks, however, the long term results need to be monitored.
Conclusion
Mega-prosthesis replacement of the elbow joint can be used for management of carefully selected resistant non union with satisfactory functional results.
Clinical Message
Management of resistant non union of the elbow joint can be a challenge due to multiple factors like bone loss, distorted anatomy, severe osteoporosis etc. Mega prosthetic replacement of the elbow can be used as a salvage surgery with satisfactory outcomes.
References
1. Morrey BF, and Sotelo JS. Elbow and Its Disorders. Fourth Edition. 2009; 800-813.
2. Vaishya R, Singh AP, Hasija R, et al. Treatment of resistant non-unionof supra condylar fractures femur by mega prosthesis. Knee Surg Sports TraumatolArthrosc. 2011;19;1137-1140.
3. Simonis RB, Nunez VA, Khaleel A. Use of the Coventry infant hip screws in the treatment of nonunion of fractures of the distal humerus. J Bone Joint Surg [Br] 2003;85-B:74-77.
4. Figgie MP, Inglis AE, Mow CS, et al. Salvage of non-union of supracondylar fracture of the humerus by total elbow arthroplasty. J. Bone Joint Surg. (Am) 1989;71:1958-65.
5. Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J. Bone Joint Surg. (Am) 1998; 80 (9):1327-35.
6. Allende C and Allende BT. Post traumatic distal humerus non-union open reduction and internal fixation long term results. IntOrthop 2009;33(5):1289-1294.
7. Ruedi TP and Murphy WM. AO principles of fracture management, 2000; 307-320.
8. Morrey BF and Adams RA. Semi constrained elbow replacement for distal humeral nonunion. J. Bone Joint Surg (Br) 1995;77:67-72.
9. Morrey BF, Bryan RS, Dobyns JH et al. Total elbow arthroplasty: a five-year experience at the Mayo Clinic. J Bone Joint Surg [Am] 1981;63-A:1050-63.
10. McKee M, Jupeter J, Toh CL, et al. Reconstruction after malunion and nonunion of intra-articular fractures of the distal humerus: methods and results in 13 adults. J Bone Joint Surg [Br] 1994;76-B:614-21.
| How to Cite This Article: Vaishya R, Vijay V, Pandit RS, Agarwal AK. Mega Prosthetic Replacement of Elbow for Resistant Nonunion of Distal Humerus. Journal of Orthopaedic Case Reports 2016 April-June;6(2): 46-49. Available from: https://www.jocr.co.in/wp/2016/04/01/2250-0685-428-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com