[box type=”bio”] What to Learn from this Article?[/box]
Acetabular prosthetic protrusion can pose a significant challenge to the management plan. In the presence of acetabular prosthetic protrusion, clinician should raise a high suspicion for chronic infection, as they lead to osteolysis and bone resorption of the acetabulum.
Case Report | Volume 6 | Issue 3 | JOCR July-Aug 2016 | Page 28-31 | Jason BT Lim, Chia Liang Ang, Hee Nee Pang. DOI: 10.13107/jocr.2250-0685.488
Authors: Jason BT Lim[1], Chia Liang Ang[1], Hee Nee Pang[1]
[1]Department of Orthopaedic Surgery, Singapore General Hospital, Outram Road, S169608, Republic of Singapore.
Address of Correspondence
Dr. Jason Lim Beng Teck,
Department of Orthopaedic Surgery, Singapore General Hospital, 20 College Road, Academia, Level 4, Singapore 169865, Republic of Singapore.
E-mail: jason.lim@mohh.com.sg
Abstract
Introduction: Bipolar hemi-arthroplasty of the hip is a commonly performed procedure in elderly patients with intra-capsular fracture of the neck of the femur with good short-term results for pain relief, return to activity and morbidity. The incidence of intra-pelvic prosthesis migration or protrusion is rare and one of the inciting factors is chronic low-grade sepsis. Acetabular prosthesis protrusion poses a difficult and challenging surgical problem due to surrounding neurovascular structures.
Case Presentation: We present a case report of 60-year-old Chinese female suffering from chronic sepsis of the hip joint causing acetabular prosthetic protrusion with a concomitant peri-prosthetic femoral shaft fracture secondary to a fall, 5 years post index surgery of bipolar hemi-arthroplasty for an intra-capsular neck of femur fracture. This patient subsequently underwent a two-stage revision total hip arthroplasty. We aim to discuss the diagnostic approach and surgical management of this complex case of infected protruded bipolar hip hemi-arthroplasty.
Conclusion: We highlight three recommendations from this clinical experience. Firstly, there should be a high index of suspicion for chronic infection in protruded prostheses following low energy trauma. Secondly, pre-operative planning for infected protruded prosthetic hips is essential, including arteriogram and a two-staged procedure to tackle possible soft tissue complications. Thirdly, the combined use of serological markers, fluid aspiration as well as intra-operative frozen section is important in the management of PJI and to confirm bacterial eradication before re-implantation.
Keywords: Acetabular, Protrusio, Bipolar, Hemiarthroplasty, Infection
Introduction
Bipolar hemi-arthroplasty of the hip is a commonly performed procedure in elderly patients with intra-capsular fracture of the neck of the femur with good short-term results for pain relief, return to activity and morbidity [1–5]. However, some of the long-term problems associated with hemi-arthroplasty include more rapid progressive acetabular cartilage degeneration due to articulation with a metallic hemi-arthroplasty component [6], groin pain, protrusion, stem loosening and subsidence. Some of the late complications leading to failure of hemi-arthroplasty include chronic infection, acetabular erosion and protrusion, aseptic femoral stem loosening and subsidence, which causes groin, thigh and the typical “start-up” pain [1–4]. The incidence of intra-pelvic prosthesis migration or protrusion is rare and one of the inciting factors is chronic low-grade sepsis [7, 8]. The destructive osteolytic process can lead to loss of the structural integrity of the hip joint, causing protruded bipolar hemi-arthroplasties [9, 10]. Acetabular prosthesis protrusion poses a difficult and challenging surgical problem, especially when the prosthesis migrates into the pelvis due to scarring of the protruded implants and adjacent neurovascular structures, such as the external iliac artery and femoral nerve [9–11]. We present a case of chronic sepsis of the hip joint causing acetabular prosthetic protrusion with a concomitant peri-prosthetic femoral shaft fracture secondary to a fall; 5 years post index surgery of bipolar hemi-arthroplasty for an intra-capsular neck of femur fracture. This patient subsequently underwent a two-stage revision total hip arthroplasty. We aim to discuss the diagnostic approach and surgical management of this complex case of infected protruded bipolar hemi-arthroplasty of the hip with a review of the literature.
Case Presentation
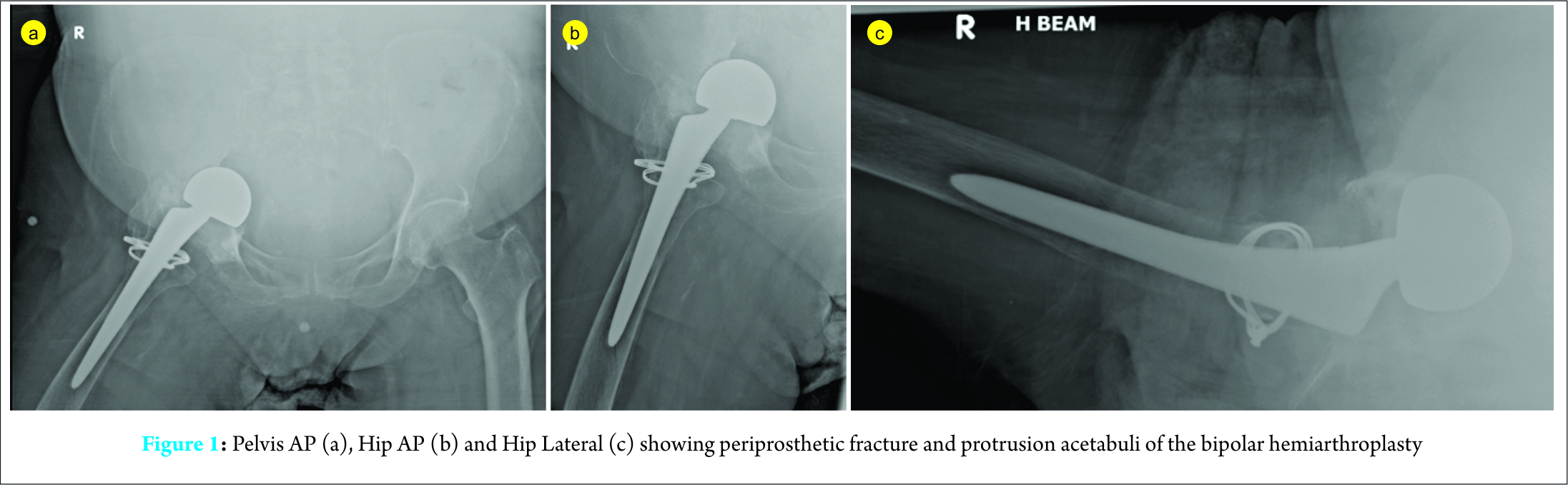
In 2009, a 60-year-old Asian woman presented with a displaced fracture of the neck of femur after a mechanical fall. She is a non-smoker and her co-morbidities include hypertension, non insulin-dependent diabetes mellitus, ischaemic heart disease and peripheral vascular disease. A right hip bipolar hemi-arthroplasty was performed and she recovered well post-operatively. She was later lost to follow-up after one year post-operatively. She was community ambulant with a walking frame 3 years post-operatively with intermittent right hip pain. 5 years later, she presented with right hip pain following a low velocity mechanical fall. Pelvic AP X-ray and right hip AP/lateral X-ray demonstrated grade III (Sotelo-Garza and Charnley 1978) severe acetabular prosthetic protrusion with peri-prosthetic fracture,causing loosening over the femoral stem implant, ( Fig. 1(a), (b) and (c)). Her C-reactive protein (CRP) was 21.7 milligram/litre and erythrocyte sedimentation rate (ESR)was 87mm/hour. CT angiogram showed a patent abdominal aorta and iliac arteries. The right common femoral artery travelling closest to the implant (within 8 mm at the 12 o’clock position) with no evidence of aneurysm or dissection noted. Aspiration of her right hip under fluoroscopic guidance was performed with negative culture and unremarkable histological findings with no malignant cells or significant acute inflammation. However, in view of the elevated inflammatory markers, there was significant concern for peri-prosthetic joint infection and the patient was counseled for a 2-stage revision arthroplasty.
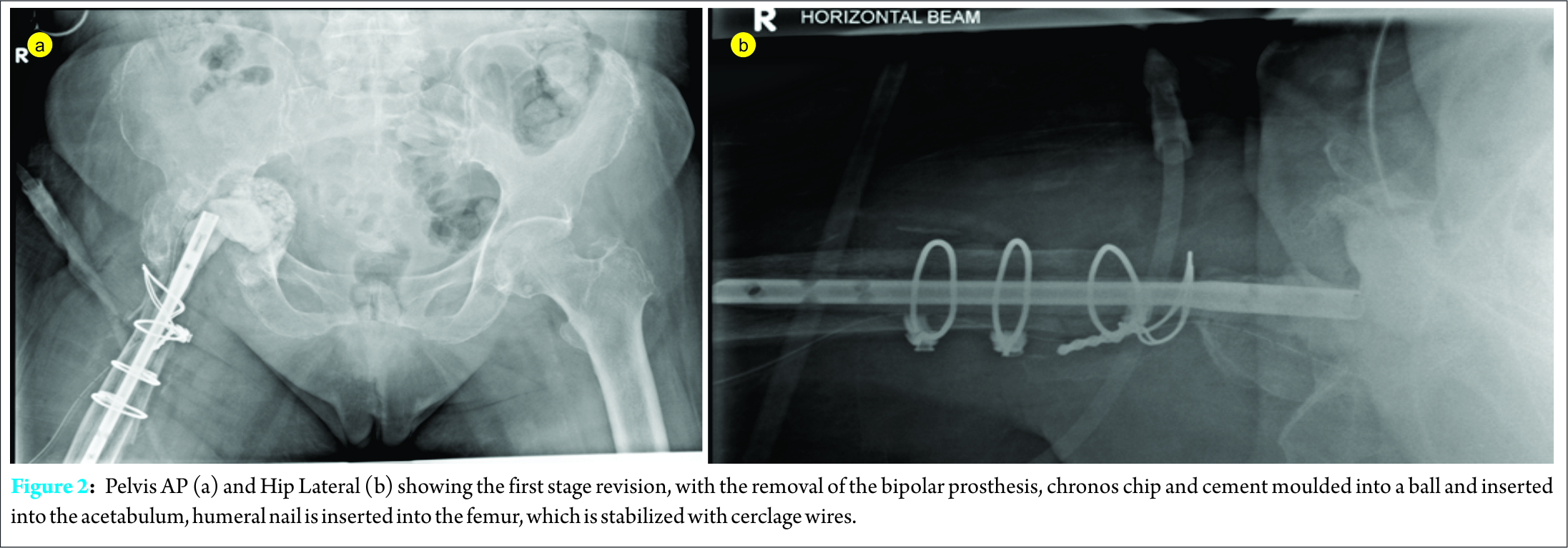
The first stage revision surgery was performed under general anaesthesia in a left lateral position. The old surgical incision via posterior approach was used. Intra-operatively, there was a large amount of fibrotic scar tissue and heterotropic ossification around the proximal femur, with no frank pus or purulent fluid collection. A thick pseudomembrane was present at the base of the protruded bipolar cup. The wires were removed and a proximal, extended trochanteric osteotomy was performed to expose the femoral stem and gain access to the acetabulum. Tissues were sent for cultures and histology. The femoral stem was removed and the superior, anterior edge of the acetabulum was osteotomised to remove the bipolar head. Methylene blue and tobramycin Simplex cement was moulded over a humeral nail and inserted into the femur as a spacer and the femoral fracture was stabilized with cable wires. The pseudomembrane at the acetabulum was covered with chronos chips and cement was moulded into a ball and inserted into the acetabulum. The greater trochanter was then stabilized to the femur and spacer with wires. Post-operative images are shown in Fig. 2(a) and (b).
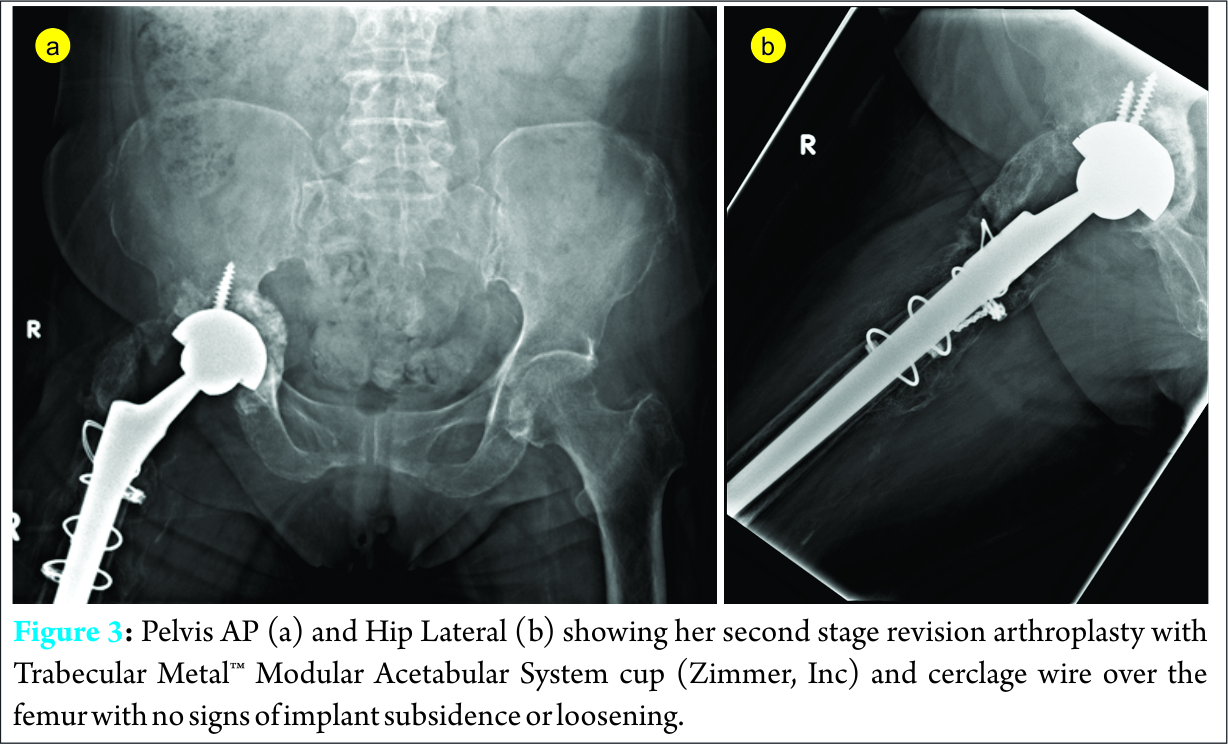
Intra-operative tissue cultures yielded pan-sensitive Citrobacter koseri. Under the advice of infectious disease specialist, the patient was started on long-term intravenous antibiotics (Aztreonam 2 grams Q8 Hourly) for 8 weeks and subsequently oral ciprofloxacin 500mg BD with trending of inflammatory markers. Before the second stage surgery, a CT-guided core biopsy of the right hip was performed to rule out residual inflammation which showed a negative culture. The patient then underwent a second stage revision arthroplasty 4 months after the first stage of revision arthroplasty. Intra-operatively, frozen section of peri-prosthetic tissues revealed no significant acute inflammatory cell infiltrate. The humeral nail and cement puck was removed. The acetabulum was reamed and fitted with Trabecular Metal™ Modular Acetabular System cup (Zimmer, Inc) with rim fit and press fit in 45 degrees inclination and 20 degrees anteversion and secured with two screws. The femur was reamed with tapered reamers and a press fit femoral stem implant was used, which is further stabilized with cerclage wires. Post-operatively the patient underwent physiotherapy and was able to ambulate on post-operative day 4 and was discharged well after one week. At six months post surgery, the patient is, ambulating well, able to do activities of daily living with minimal right hip pain, her follow-up images are shown in Fig. 3(a) and (b).
Discussion
In a meta-analysis by Bhandari et al.(2003) [13], the use of arthroplasty for the treatment of displaced femoral neck fractures significantly reduces the risk of revision surgery, at the cost of greater infection rates, blood loss and longer operative timing. Acetabular prosthetic protrusio is a known late complication following bipolar hemi-arthroplasty. In some retrospective studies [14, 15], there are no reports of protrusion in their follow-up. One of the main reasons for protruded bipolar hemi-arthroplasties is due to the presence of infection [9, 10]. The surgical approach to prosthetic protrusion requires several considerations. A pre-operative arteriogram is required to assess the external iliac vessels, which could be entrapped in the scar tissue from the protruded implants. This is because the presence of false aneurysms or any neurovascular involvement could pose a substantial challenge for the surgeon, requiring meticulous removal of the protruded prosthesis [10,11,16]. The diagnosis of peri-prosthetic joint infection (PJI) remains a challenge, as there is no single pre-operative investigative modality that is completely reliable. In addition, there are various diagnostic criteria for PJI. The American Academy of Orthopaedic Surgeons [17] has developed recommendations for the diagnosis of PJI, including the use of hip aspiration if both the ESR and CRP tests are abnormal. More recently, the Musculoskeletal Infection Society (MSIS) has developed a set of criteria for the diagnosis of PJI [18].The ultimate goal of management of PJI is to eradicate the infection and reconstruct a functional, painless and stable hip joint [19]. Single-stage revision (i.e. irrigation, debridement, and re-implantation performed during the same surgery) has been reported to be successful for infected THA [20]. However, due to the wound complexity and soft tissue involvement in infected acetabular prosthetic protrusio, a two-stage reconstruction is recommended [10,11], which was performed in our case report. A decline in ESR and CRP levels along with absence of clinical signs of infection are often taken as an indication that it is safe to proceed with the second stage of revision surgery. The use of joint fluid analysis before second stage procedure is helpful to determine the eradication of PJI. In the study by Shukla et al. [21], they reported that the synovial white blood cell count best identified persistent infection with a cutoff value of 3,528 cells/L, which has 78% sensitivity and 96% specificity. This value is close to the commonly accepted value of 3,000 cells/L for the diagnosis of PJI [22]. We report a rare occurrence of chronic sepsis that is associated with intra-pelvic protrusion of acetabular components following bipolar hemi-arthroplasty. From literature review, it has been obsesrved that the infected cases were mostly female with no apparent explanation for this finding [10]. The presence of acetabular prosthetic protrusion should raise a high suspicion for chronic infection, as they lead to osteolysis and bone resorption of the acetabulum [23]. In our case report, the use of hip aspiration prior to the first and second stage revision surgeries yielded negative cultures. As there were other indications of chronic sepsis of the hip, with elevated inflammatory markers, as well as protrusion of the acetabulum, there was significant concern for peri-prosthetic joint infection, which necessitates the use of 2-stage revision arthroplasty for a long-term successful result. During the first staged procedure, the intra-operative cultures were positive, confirming the presence of PJI. In the second stage of the procedure, the use of frozen section was important to aid in confirmation of the eradication of PJI before proceeding with re-implantation, as the presence of infection would cause a failure of the re-implantation.
Conclusion
This case report contributes to the literature for acetabular prosthetic protrusion secondary to infection. The presence of acetabular prosthetic protrusion should raise a high suspicion for chronic infection, as they lead to osteolysis and bone resorption of the acetabulum.
Clinical Message
There are three recommendations from this clinical experience. Firstly, there should be a high index of suspicion for chronic infection in protruded prostheses following low energy trauma. Secondly, pre-operative planning for infected protruded prosthetic hips is essential, including arteriogram and a two-staged procedure to tackle possible soft tissue complications. Thirdly, the combined use of serological markers, fluid aspiration as well as intra-operative frozen section is important in the management of PJI and to confirm bacterial eradication before re-implantation
References
1. Sierra R J, Cabanela M E. Conversion of failed hip hemi- arthroplasties after femoral neck fractures. Clin Orthop 2002;399:129-39.
2. Haidukewych G J, Israel T A, Berry D J. Long-term survivorship of cemented bipolar hemiarthroplasty for fracture of the femoral neck. Clin Orthop 2002;(403:118-26.
3. Eiskjaer S, Ostgard S E. Survivorship analysis of hemiarthroplasties. Clin Orthop 1993;(286:206-11.
4. Pankaj A, Malhotra R, Bhan S. Conversion of failed hemiarthroplasty to total hip arthroplasty: a short to mid-term follow-up study. Indian J Orthop. 2008;42(3):294-300.
5. Diwanji SR, Kim SK, Seon JK, Park SJ, et al. Clinical results of conversion total hip arthroplasty after failed bipolar hemiarthroplasty. J Arthroplasty. 2008;23(7):1009-15.
6. Dalldorf P G, Banas M P, Hicks D G, Pellegrini V D, Jr. Rate of degeneration of human acetabular cartilage after hemiarthroplasty. J Bone Joint Surg (Am) 1995;77 (6): 877-82.
7. Garvin KL, Hanssen AD. Infection after total hip arthroplasty. Past, present, and future. J Bone Joint Surg Am. 1995;77(10):1576-88. Review.
8. Ibrahim MS, Raja S, Khan MA, Haddad FS. A multidisciplinary team approach to two-stage revision for the infected hip replacement: a minimum five-year follow-up study. Bone Joint J. 2014;96-B(10):1312-8.
9. Cameron HU, Hood-Szivek P, Turner R. Femoral head migration after single assembly total hip arthroplasty. Clin Orthop Relat Res. 1982;(164):230-3.
10. Stiehl JB. Acetabular prosthetic protrusion and sepsis: case report and review of the literature. J Arthroplasty 2007;22(2):283-8. Review.
11. Stiehl JB, Harlow M, Hackbarth D. Extensile triradiate approach for complex acetabular reconstruction in total hip arthroplasty. Clin Orthop Relat Res. 1993;294:162-9.
12. Sotelo-Garza A, Charnley J: The results of Charnley arthroplasty of the hip performed for protrusio acetabuli. Clin Orthop 1978;132:12-18.
13. Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P 3rd, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85-A(9):1673-81.
14. Mazen S, Julien G, Riad F. Retrospective evaluation of bipolar hip arthroplasty in fractures of the proximal femur. N Am J Med Sci. 2010;2(9):409-15.
15. Overgaard S, Jensen TT, Bonde G, Mossing NB. The uncemented bipolar hemiarthroplasty for displaced femoral neck fractures. 6-year follow-up of 171 cases. Acta Orthop Scand. 1991;62(2):115-20.
16. Giacchetto J, Gallagher JJ. False aneurysm of the common femoral artery secondary to migration of a threaded acetabular component. A case report and review of the literature. Clin Orthop Relat Res. 1988;231:91-6.
17. Della Valle C, Parvizi J, Bauer TW; American Academy of Orthopaedic Surgeons, et al: American Academy of Orthopaedic Surgeons clinical practice guideline on: The diagnosis of periprosthetic joint infections of the hip and knee. J Bone Joint Surg Am 2011;93(14):1355-1357.
18. Parvizi J, Zmistowski B, Berbari EF, et al: New definition for periprosthetic joint infection: From the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469(11):2992-2994.
19. Kuzyk PR, Dhotar HS, Sternheim A, Gross AE, et al. Two-stage revision arthroplasty for management of chronic periprosthetic hip and knee infection: techniques, controversies, and outcomes. J Am Acad Orthop Surg. 2014:22(3):153-64.
20. Callaghan JJ, Katz RP, Johnston RC: One-stage revision surgery of the infected hip: A minimum 10-year followup study. Clin Orthop Relat Res 1999;369:139-143.
21. Shukla SK, Ward JP, Jacofsky MC, Sporer SM, et al. Perioperative testing for persistent sepsis following resection arthroplasty of the hip for periprosthetic infection. J Arthroplasty 2010;25(6):87-91.
22. Schinsky MF, Della Valle CJ, Sporer SM, Paprosky WG. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg Am 2008;90(9):1869-1875.
23. Tigges S, Stiles RG, Roberson JR. Appearance of septic hip prostheses on plain radiographs. AJR Am J Roentgenol. 1994;163(2):377-80.
| How to Cite This Article: Jason BT Lim, Chia Liang Ang, Hee Nee Pang. Acetabular Prosthetic Protrusio after Bipolar Hemi-Arthroplasty of the Hip: Case Report and Review of the literature. Journal of Orthopaedic Case Reports 2016 July-Aug;6(3):28-31. Available from: https://www.jocr.co.in/wp/2016/07/10/2250-0685-488-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com