[box type=”bio”] What to Learn from this Article?[/box]
Tendon rupture in needle aponeurotomy for Dupuytren disease is a rare complication leading to surgical revision, for those who wish to perform the PNA, they need to know some technical artifices that enable these complications to be reduced, albeit not eliminated.
Case Report | Volume 6 | Issue 3 | JOCR July-Aug 2016 | Page 88-90 | Salma Otayek, Jérôme Pierrart, Emmanuel H. Masmejean. DOI: 10.13107/jocr.2250-0685.528
Authors: Salma Otayek, Jérôme Pierrart, Emmanuel H. Masmejean
[1]Departement of Hand, Upper Limb and Peripheral Nerve Surgery. European Georges, Pompidou Hospital (HEGP) AP-HP, Paris. France.
[2]Faculty of Medicine, René Descartes. Paris. France.
Address of Correspondence
Dr. Otayek Salma,
Department of Hand, Upper Limb and Peripheral Nerve Surgery. European Georges Pompidou Hospital (HEGP). 20, rue Leblanc, 75908 Paris cedex 15, France.
E-mail : salma_otayek@hotmail.com
Abstract
Introduction: The Percutaneous Needle Aponeurotomy (PNA) is a known and validated non-surgical treatment for Dupuytren’s disease with a low rate of complications. Initially described for purely palmar forms, the indications extended to digital adhesions. Numerous surgeons remain hesitant about performing the PNA for digital treatment because of the risk of lesions in the noble structures. In literature, one complication is still rare, even non-existent, i.e. the tendon rupture.
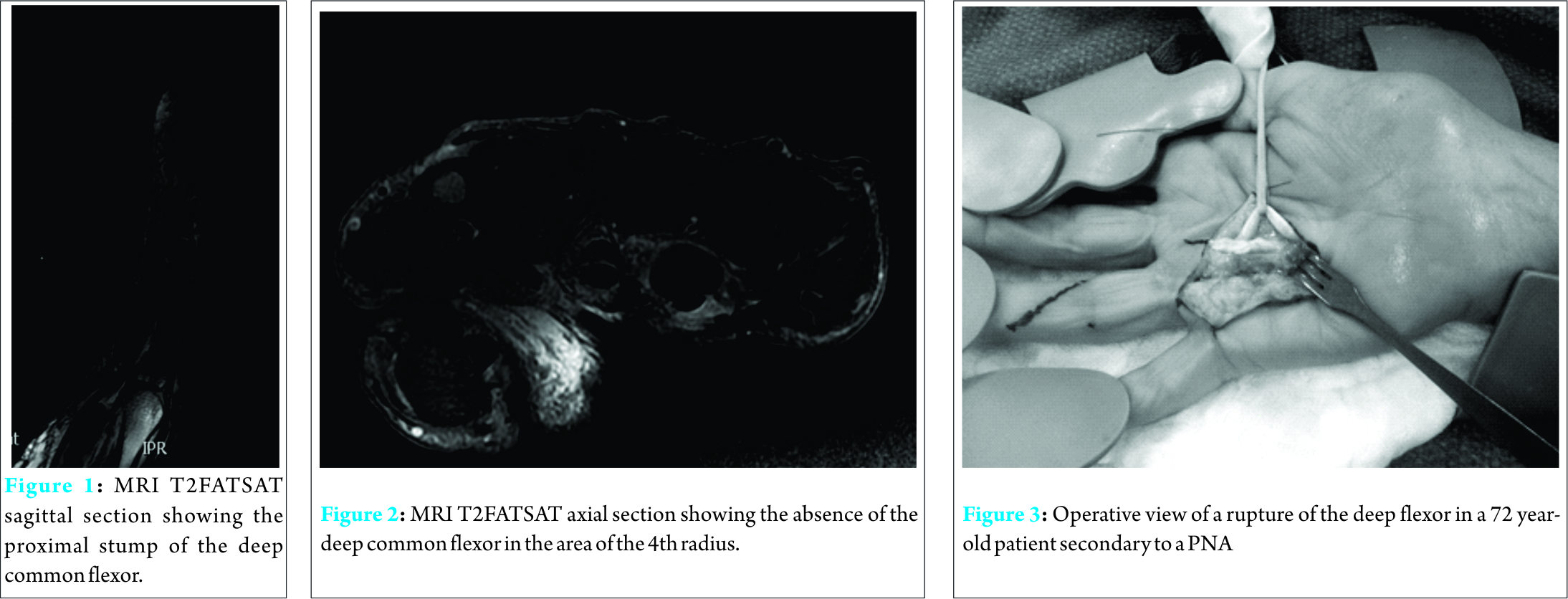
Case Presentation: We are reporting here the case of a rupture of the deep common flexor tendon, secondary to a needle aponeurotomy, for a recurring digital form in a 72 year-old woman. We performed surgical treatment by tenodesis of the distal stump and resection of the proximal stump. The result was satisfactory.
Conclusion: The purpose of describing this case is to report this rare complication leading to surgical revision. Within our team, we do not recommend performing PNAs for digital cases, and even less so for recurrences. For those who wish to perform the PNA, they need to know some technical artifices that enable these complications to be reduced, albeit not eliminated.
Keywords: Dupuytren, aponeurotomy, needle, tendon rupture
Introduction
Dupuytren’s disease is a disease affecting the palmar aponeurotic complex that is the cause of adhesions responsible for retractions of the fingers [1], which sometimes is a disabling condition. The goal of current treatments, be they surgical or not, is to reduce or even eliminate this digital retraction. These treatments are, above all, symptomatic. The Percutaneous Needle Aponeurotomy (PNA) is a known and validated non-surgical treatment [2, 3]. The principle consists in performing one or more percutaneous sections of the aponeurotic adhesions with the help of the bezel of a needle [4]. Historically, the fasciotomy was introduced by Henry Cline Senior (1777), then resumed by Sir Astley Cooper (1822) and Baron Guillaume Dupuytren. It was publicized by Lermusiaux in 1972 [5]. It is a simple, effective and quick treatment [6,7] that has been the subject of several studies showing satisfactory results with a low rate of complications [2, 4, 6–8]. Initially, this technique was reserved for palmar adhesions. Currently, the indications have been extended to digital [9] adhesions. According to many authors, the percutaneous needle aponeurotomy of digital adhesions can be performed with no risk. The percutaneous needle aponeurotomy on the palm is performed by a majority of hand surgeons and is part of the therapeutic arsenal. With regard to digital adhesions, many of these surgeons are reluctant because of the potential risks of neurovascular or tendinous [6, 7] lesions. There is a close relationships between the digital adhesion and the neurovascular and tendinous [7] structures. Therefore, it may be difficult to guarantee the safety of these noble structures. The most frequently reported complications in literature are: cutaneous rupture, transient dysesthesia, pain, local infection and hematoma [6, 7, 10]. On the other hand, to our knowledge [8, 10, 11], reports of tendon rupture as a complication are more the exception than the rule. Here, we report the case of a rupture of the deep common flexor tendon secondary to a needle aponeurotomy for a recurring digital form. The purpose of describing this case is to report this rare complication leading to surgical revision.
Case Presentation
This case involved a 73-year-old woman who was retired, right-handed, a smoker, with no medical history and was not taking any medication. The patient underwent a bilateral aponeurectomy for digitopalmar Dupuytren’s disease. Two years later, she presented an excellent result in the left hand, but a recurrence on the right hand involving the fourth radius on the central digital adhesion next to the proximal interphalangeal joint. A sewing machine-type rheumatological PNA was performed in the digital area. Three weeks later, the after effects were marked by a deficiency of flexion in the distal interphalangeal (DIP) joint, which occurred without making an effort; the patient did not undergo any rehabilitation and did not wear a splint. The MRI confirmed the rupture of the deep common flexor tendon at the first phalanx of the fourth radius with a proximal stump retracted into the palm (Fig. 1) (Fig. 2). The surgical indication was retained. The operation was performed in outpatient surgery Under locoregional anesthesia. Under loupe magnification, a Z-shaped incision was made, according to Bruner. The exploration permitted detection of the proximal stump of the deep common flexor at the palm (Fig. 3). The latter was resected. In a subsequent surgery, tenodesis of the distal stump was performed at the digital canal and at the palmar plate of the DIP at 10° of flexion. A dorsal splint supporting the DIP was worn for a duration of five weeks.
Six months after surgery, the patient was satisfied and did not present any pain; her DIP was stable, she could curl up her fingers almost completely and functionally, with a pulp-to-palm distance at 1 cm. We observed a flexum of the proximal interphalangeal [PIP) joint of 20°.
Discussion
Tendon rupture is a rare complication that deserves to be known. It would be lower than 1% in case of a trained surgeon, according to Lermusiaux et al [3]. In literature, five tendon ruptures were reported for the palmar-digital forms in the Lariboisière series of 60,000 PNAs [3,4], 0.2% in the series of Badois et al [5] of 779 PNAs and none in the series of 311 cases of Foucher et al [6]. It requires surgical treatment. The latter is difficult, because the indication of secondary reconstruction of the flexor tendons and the choice of technique depend on the condition of the tendons involved [12]. In post-PNA ruptures, the tendons are dilacerated by the needle,thus making any direct suture impossible [13]. The local and inflammatory context linked to Dupuytren’s disease makes a single or second tendon graft technically difficult. In this context, one generally uses palliative treatments. These involve tenodesis and arthrodesis, the purpose of which is to stabilize the DIP at the time of the digital [12] operations. In our observation, tendon rupture occurred after a PNA of a digital adhesion was performed on a recurrence. Badois et al [5] showed that it was possible to resume the surgical recurrences by means of the PNA but with a higher risk of tendon rupture. Our clinical case reinforces their conclusions. Two PNA techniques exist, i.e. the sewing machine technique according to the vertical Lariboisière school, and the pendular technique of the micro scalpel with the needle’s Bezel [9, 10, 13]. The pendular technique utilized by surgeons is safer for protecting oneself against nerve and tendon lesions. In the pendular technique, the transverse movements permit improved control over depth when sectioning the adhesion into successive layers, going from the surface down into the deep area. The surgeon has better control of his/her senses in order to avoid damage to tendons and nerves [7, 9]. To us, it seems impossible to control the depth when using the sewing machine technique. For numerous hand surgeons, the needle PNA should not be performed in the digital area due to the risks of iatrogenic lesions [9] linked to the close relationships between the adhesions and the neurovascular structures. The adhesions at the finger may have a spiral path around the pedicle. These so-called spiral adhesions develop alternately behind and ahead of the collateral neurovascular pedicle, and they trace a spiral path around it [14]. They originate from a pretendinous palmar adhesion and terminate at the tendon sheath or on the bone ahead of the collateral neurovascular pedicle. These adhesions change the path of the neurovascular pedicles by medializing them and making them more superficial. At the time of the surgical aponeurectomy, these spiral adhesions are considered serious by surgeons, even under controlled magnified view. For Foucher and, prior to him, Short and Watson [14], it is possible to anticipate the areas at risk, but false positives are possible [6]. For these authors, when the skin adheres to the cord, there is no risk of interposition of the bundle between the skin and the cord; however, when the skin is mobile vis-à-vis the adhesion, there is a possibility of interposition of the bundle and, therefore, of the neurovascular section. When there is a space of mobility between the skin and the adhesion, this therefore involves contraindication against performing a PNA in this area. The other contraindications are: infiltrating forms, severe and old digital localizations and postsurgical digital recurrences [6]. With regard to the tendons, that is not the issue. Tendons are always situated under the adhesion; their location is not changed by the adhesions and, therefore, is foreseeable. For us, this involves technical problems. To avoid tendon rupture, it is necessary to always check, by means of movements of flexion and extension of the finger, that the needle is not touching the tendon. If this is the case, one must visually note to what depth one feels this contact in order to avoid pricking deeper [2]. Tendon rupture is late or semi-late; it can occur a few days to a few weeks after the PNA, and occurs most often at the time of a forced contraction of the flexors [13]. This belated onset is in favor of a partial rupture that accumulates. The tendons behave like cords and, like it, the deficit only occurs when the rupture is complete. Therefore, it is likely that many partial ruptures of tendons occur unnoticed, because they are asymptomatic and the rate of post-PNA tendon problems is perhaps underestimated. It seems to us that a post-PNA study of flexor tendons would be useful in analyzing the actual rate of tendinous lesions. An ultrasound study would be quite appropriate for this.
Conclusion
Tendon rupture is a rare complication. It requires informing the patient beforehand regarding the risk of definite after effects if a tendon rupture occurs. Due to the close relationships between the adhesion and the noble structures, the PNA must not be performed in the digital area, especially at the time of recurrences. For surgeons who wish to perform this, only an experienced practitioner should do it by prioritizing the pendular technique and by using the artifices that enable verification of the absence of contact between the needle and the tendons.
Clinical Message
Tendon rupture is a rare complication.The purpose of describing this case is to report this rare complication leading to surgical revision. For those who wish to perform the PNA, they need to know some technical artifices that enable these complications to be reduced, albeit not eliminated.
References
1. Carvalhana G, Auquit-Auckbur I, Milliez P-Y. Maladie de Dupuytren : état desconnaissances et de la recherche en physiopathologie. Chir Main. 2011;30(4):239–45
2. Lermusiaux JL, Lellouche H, Badois JF, Kuntz D. How should Dupuytren’sContracture be managed in 1997? Rev Rhum Engl Ed. 1997;64(12):775–6.
3. Lermusiaux J-L, Badois F, Lellouche H. Maladie de Dupuytren. Rev Rhum – Vol68 – N° 6 – P 542-547.
4. Beaudreuil J, Lellouche H, Roulot E, Orcel P, Bardin T. Maladie de Dupuytren.EMC – Appar Locomoteur. 2011 Jan;6(4):1–13.
5. Badois FJ, Lermusiaux JL, Massé C, Kuntz D. [Non-surgical treatment ofDupuytren disease using needle fasciotomy]. Rev Rhum Ed Fr 199330;60(11):808–13.
6. Foucher G, Medina J, Navarro R. Percutaneous needle aponeurotomy:complications and results. J Hand Surg EdinbScotl. 2003;28(5):427–31.
7. Raimbeau G, Le Bourg M, Fouque PA, Saint-Cast Y. Aponévrotomie à l’aiguille:technique utile ou dangereuse dans le traitement de la maladie de Dupuytren? E-MémAcadémie NatlChir. 2013;12(1):046–50.
8. Cheng HS, Hung LK, Tse WL, Ho PC. Needle aponeurotomy for Dupuytren’scontracture. J Orthop Surg Hong Kong 2008;16(1):88–90.
9. Ganeval A, Blancher M-C, Gouzou S, Liverneaux P. L’aponévrotomie digitale àl’aiguille dans la maladie de Dupuytren entraîne-t-elle des lésions des nerfs collatéraux ?À propos d’une série de 25 doigts. Ann Chir Plast Esthét. 2010;55(1):35–41.
10. Beaudreuil J, Lellouche H, Orcel P, Bardin T. Needle aponeurotomy inDupuytren’sdisease. Joint Bone Spine. 2012;79(1):13–6.
11. Van Rijssen AL, Werker PMN. Percutaneous needle fasciotomy in dupuytren’sdisease. J Hand Surg EdinbScotl. 2006;31(5):498–501.
12. Santa DD. Lésions anciennes des tendons fléchisseurs des doigts. Rev Rhum -Vol 68 – N° 6 – P 542-547.
13. Manet M-P, Roulot E, Teyssedou J-P, Lahalle S, et al. Maladie deDupuytren : l’aponévrotomie percutanée à l’aiguille est une alternative à la chirurgie. RevMédecine Interne 2011;32(4):241–8.
14. Short WH, Watson HK. Prediction of the spiral nerve in Dupuytren’s contracture.J Hand Surg. 1982;7(1):84–6.
| How to Cite This Article: Salma Otayek, Jérôme Pierrart, Emmanuel H. Masmejean. Dupuytren’s disease and needle aponeurotomy: rupture of a deep common flexor tendon: A case report and literature review. Journal of Orthopaedic Case Reports 2016 July-Aug;6(3):88-90. Available from: https://www.jocr.co.in/wp/2016/07/10/2250-0685-528-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com