[box type=”bio”] Learning Points for this Article: [/box]
Spondylodisicits caused by NTM is rare and often missed. High degree of suspicion is required. It can present as progressive consecutive vertebral body sclerosis. If required, open biopsy should be done to procure adequate samples for diagnosis. Prolong culture techniques are required to grow the organism.
Case Report | Volume 7 | Issue 6 | JOCR November – December 2017 | Page 89-92| Kunal Shah, Gaurang Atodaria, Milind Patwardhan, Abhay Nene. DOI: 10.13107/jocr.2250-0685.964
Authors: Kunal Shah [1], Gaurang Atodaria [2], Milind Patwardhan [2], Abhay Nene [2]
[1] Department of Spine, “We Are Spine “, Ghatkopar, Mumbai, Maharashtra. India.
[2] Department of Spine, Wockhardt Hospital, Mumbai, Maharashtra. India.
Address of Correspondence:
Dr. Kunal Shah,
Consultant Spine Surgeon, We Are Spine Centre, Aarav Polyclinic LBS Road, Opposite Telephone Exchange, Ghatkopar (West), Mumbai -86, Maharashtra, India.
E-mail: orthokunal@yahoo.com
Abstract
Introduction: Non-tuberculous mycobacteria (NTM) are slow-growing organisms affecting both immunocompromised and immunocompetent patients. As compared to tuberculosis, they pose formidable challenge in successful management beginning with diagnosis extending through its treatment.
Case Report: Our case highlights unusual spinal presentation of NTM, intricacies in diagnosis, and successful management.
Conclusion: As the prevalence of NTM is rising, it is important as clinicians to understand unique aspects which differ from tuberculosis for appropriate and successful treatment.
Keywords: Non-tuberculous mycobacteria, spondylodiscitis, vertebral sclerosis.
Introduction
Common causes of spondylodiscitis of spine are tuberculosis and pyogenic. Atypical infections of spine are not uncommon. We have seen isolated reports of various kinds of atypical infections such as fungal (mucormycosis, Cryptococcus, and blastomycosis), parasitic (hydatid disease, toxoplasmosis, and cysticercosis), and non-tuberculous mycobacteria (NTM) [1, 2, 3]. Therefore, high degree of suspicion and methodical approach is important in early diagnosis and successful treatment. NTM are widely distributed in environment and comprises more than 150 species of mycobacteria. It commonly affects immunocompromised patients; however, it is also seen in immunocompetent patients. NTM are of two types; slow growing and fast growing. Osteomyelitis is commonly caused by slow-growing organisms such as Mycobacteria avium-intracellulare complex, Mycobacterium ulcerans, and Mycobacterium marinum. [4, 5] It most commonly affects pulmonary system. Skeletal affection is not uncommon and is seen in the form of chronic granulomatous affection in bursae, joints, and bone. It is caused by direct inoculation through puncture wound, injection, surgical incision, or accidental trauma [4]. Vertebral osteomyelitis is extremely rare with only few case reports described in literature. Thoracic spine is commonly affected followed by lumbar spine. Unlike other skeletal affection, vertebral involvement is rarely caused by direct inoculation. Hematogenic or lymphogenic route has been described. Delayed diagnosis is a major concern and independent risk factor in successful management of NTM spondylodiscitis, especially in slow-growing mycobacteria [4, 6]. We describe a case of NTM spondylodiscitis with its clinic-radiological presentation, diagnostic dilemma, and successful management.
Case Report
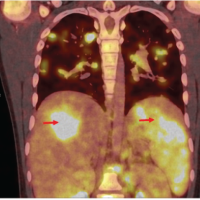
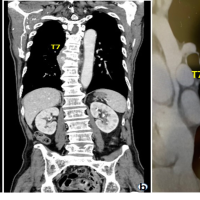
We report a case of 28-year-old female, presented to the outpatient department with mechanical mid back pain with the right girdle radiation, since 2 years. She also had rest pain and night pain. There were no constitutional symptoms. On examination, there was no neurological involvement. There was local tenderness present over mid-thoracic region. No other local signs of infection were present. Straight leg raise test was negative. She was diabetic on oral hypoglycemic drugs. She had magnetic resonance imaging (MRI) scans dating 4 years back which revealed spondylodiscitis at T8-T9 level with prespinal and paraspinal soft tissue component and intense enhancement of T8-T9 vertebral body (Fig. 1). Based on that computed tomography-guided biopsy (histopathology and tuberculous culture) was done elsewhere which came negative. Empirical antituberculous treatment (ATT) (primary line drugs) was given thereafter for 2 years. However, she did not improve clinically and radiologically. At this time, radiograph showed vertebral body sclerosis T8-9 (Fig. 2) and MRI showed T8-9-10 marrow edema and prevertebral and paravertebral soft tissue component with epidural compression (Fig. 3), worsening seen in spite on ATT. This time transpedicular decompression was done elsewhere and sample was sent for examination, which unfortunately again came to be negative (histopathology and tuberculous culture). Empirical ATT (primary line drugs) was started and given for 18 months, but there was no clinical improvement.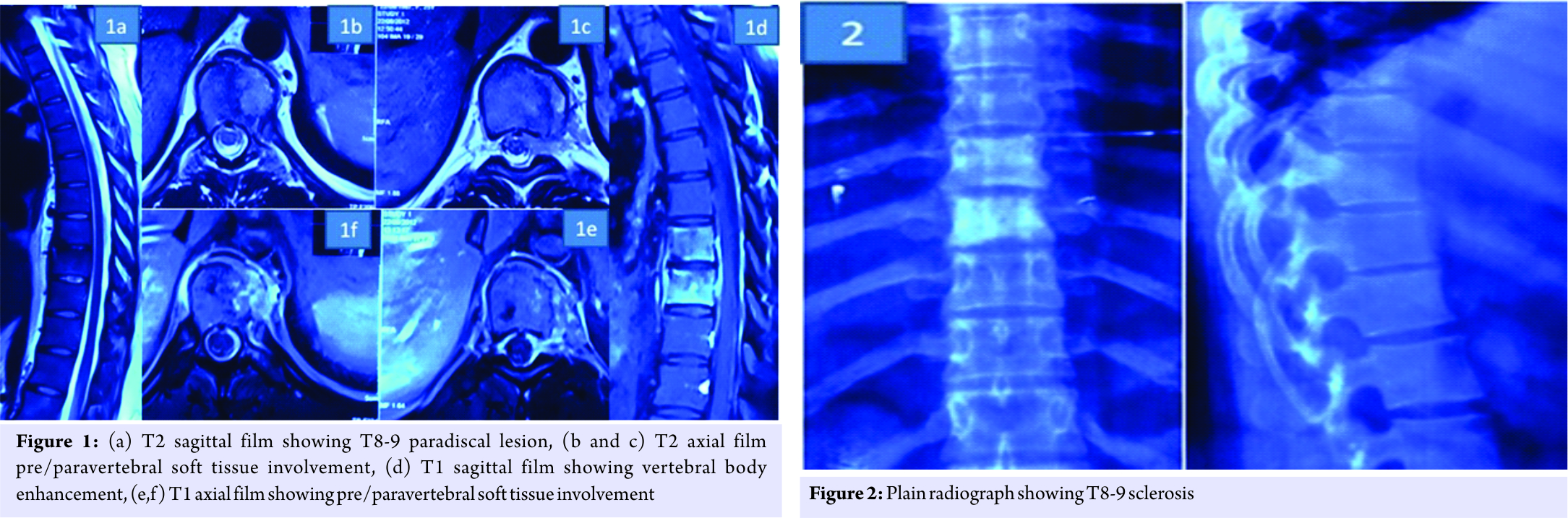
We did plain radiograph (Fig. 4) which showed thoracic 8-9-10 sclerosis, which had progressed as compared to the previous radiograph. MRI scan (Fig. 5) showed T8-9-10 involvement with soft tissue component similar to last scan. Laboratory investigations showed erythrocyte sedimentation rate-45, C-reactive protein positive, and white blood cell counts were normal.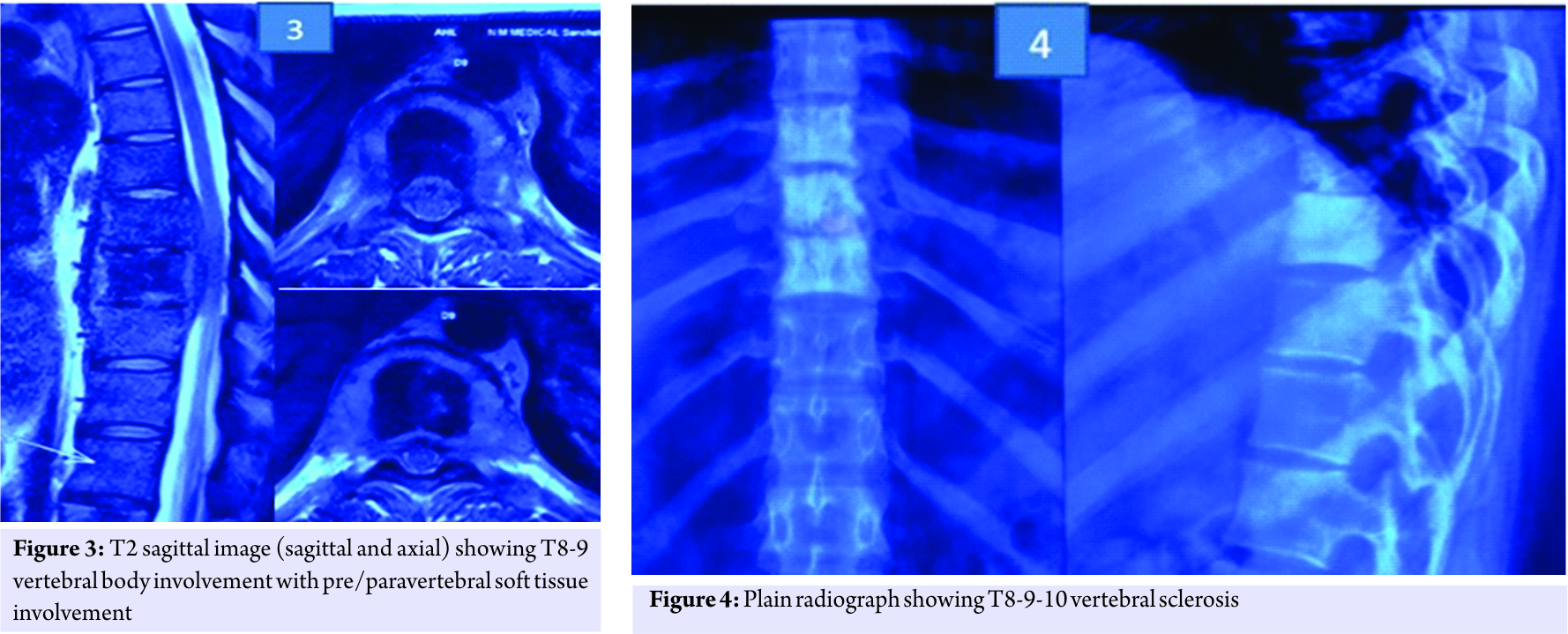
Based on imaging and history, our main differential diagnoses were as follows:
1. Mycobacteria tuberculosis.
2. Slow-growing organism’s, for example, atypical mycobacteria.
3. Sclerosing vertebral metastasis/idiopathic vertebral sclerosis was less likely as soft tissue component is rarely seen in these conditions.
4. Pyogenic or fungal causes for spondylodiscitis were less likely as the course of disease was less aggressive with lack of any other constitutional symptoms.
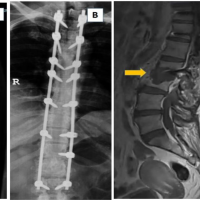
We performed a posterolateral decompression. We did not do any fixation as thoracic spine is relatively stable due to the presence of rib cage and there was no radiological evidence of instability. Intraoperatively, pus was encountered with granulation tissue. The sample was sent for histopathology and culture. Histopathology report suggested of non-granulomatous infection. Culture at 6 weeks suggested Mycobacteria intracellulare.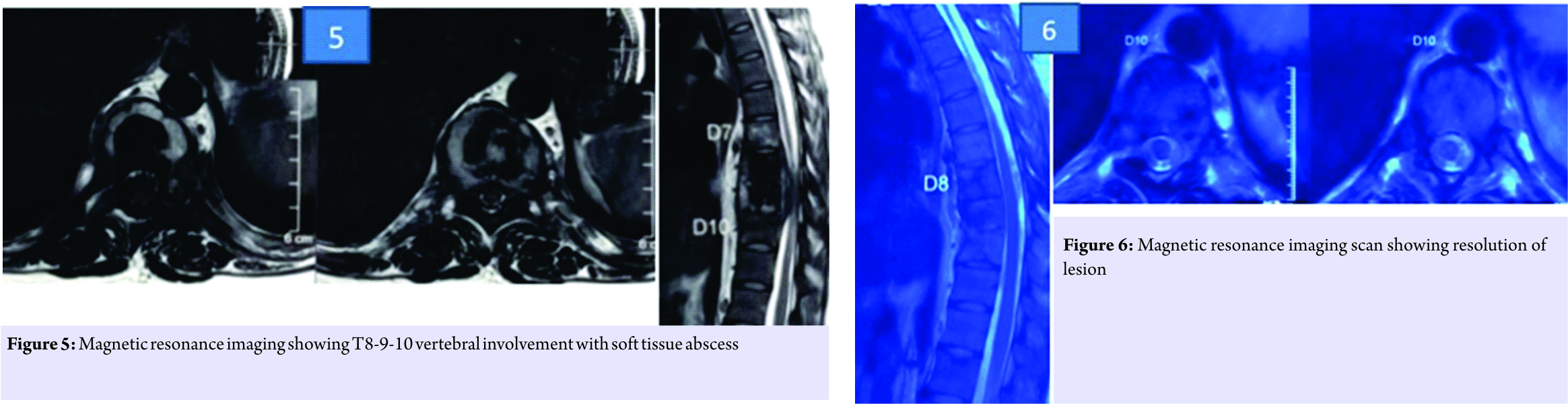
Antibiotics were started in consultation with infectious disease specialist. She was given rifampicin, ethambutol, and clarithromycin for a year. At 1-year follow-up, the patient showed good clinical improvement. Her MRI showed resolution of lesion (Fig.6). Inflammatory markers were within normal values. After 1 year of stopping the medicines, the patient shows no clinical recurrence.
Discussion
Vertebral body sclerosis is an uncommon finding. It is seen in cases of metastasis, lymphoma, tuberculosis, hemangioma, idiopathic vertebral sclerosis, and Paget’s disease of bone [7, 8]. However, sclerosis along with soft tissue component points in favor of infective etiology. Sclerosis in infection is reactive sclerosis, which tends to progress as pathology increases [8]. Our case had three consecutive vertebral body scleroses which were progressive over 4 years suggesting increase in pathology. Tissue diagnosis and culture should be done in all cases and are preferred, especially when getting diagnosis, is of prime importance. Percutaneous techniques for biopsy have a variable rate of positive yield ranging from 36% to 91% in the infectious spondylodiscitis. Percutaneous biopsy can be false negative due to various reasons such as inadequate sample size, sampling error, and empirical antibiotics at the time of biopsy [9]. Open biopsy is the most reliable method of procuring sample for diagnosis and has higher success rate [10]. Delay in diagnosis is common causing poor outcome. Therefore, multiple culture samples and more importantly prolonged culture techniques are recommended. In our case, previous biopsies were negative, so we needed better targeted sample with good quantity to grow the organism. Hence, surgery was done and prolonged culture helped in procuring the diagnosis. Surgical debridement also helped in reduction of tissue load of infection. Treatment of NTM osteomyelitis involves surgical debridement and chemotherapy. It is been shown that surgical debridement is adequate for NTM osteomyelitis. However, additional chemotherapy is beneficial [5, 9]. Kato et al. recently reported no infection recurrence in a patient with vertebral osteomyelitis treated by debridement and surgery using antibacterial iodine supported instrumentation [11]. Kim et al. in an analysis of 69 patients reported 67.6% of patients required surgery. Drug regimen should ideally be given based on drug sensitivity as per American thoracic society [6]. Literature suggests correlations between the type of organism and antibiotics to be considered. Among slow-growing NTM, clear correlations have been established for amikacin and macrolides (M. avium complex) and for rifampicin (Mycobacterium kansasii). Among rapid-growing NTM, correlations have been established in extrapulmonary disease for aminoglycosides, cotrimoxazole, and cefoxitin. In pulmonary disease, outcomes are poor and correlations are less clear, especially for Mycobacterium abscessus [12]. Duration of chemotherapy in slow-growing NTM is at least 1 year and fast-growing NTM is at least 6 months [6]. Our case had isolated of M. intracellulare, which was slow-growing organism, so antibiotics were given for a year. Differentiating NTM from tuberculosis can be tricky. The complexity of the diagnosis is due to the indolent nature of the disease, non-specific symptoms, lack of distinctive clinic radiological signs, and lack of suspicion.
Conclusion
NTM can present as progressive consecutive vertebral sclerosis. Its differentiation from tuberculosis can be sometimes tricky due to lack of specific clinic-radiological findings. High level of suspicion is required for early diagnosis and treatment.
Clinical Message
Spondylodiscitis caused by NTM can be often missed. Prolong culture techniques should be used for growth, especially in slow-growing microbes. Appropriate tissue diagnosis by open biopsy if required must be done in a timely manner to prevent delaying diagnosis.
References
1. Hadgaonkar S, Shah K, Bhojraj S, Nene A, Shyam A. Isolated mucormycotic spondylodiscitis of lumbar spine-a rare case report. J Orthop Case Rep 2015;5:55-7.
2. Chen CH, Chen WL, Yen HC. Candida albicans lumbar spondylodiscitis in an intravenous drug user: A case report. BMC Res Notes 2013;6:529.
3. Latta TN, Mandapat AL, Myers JP. Anaerobic spondylodiscitis due to Fusobacterium species: A case report review of the literature. Case Rep Infect Dis 2015;2015:759539.
4. Bi S, Hu FS, Yu HY, Xu KJ, Zheng BW, Ji ZK, et al. Nontuberculous mycobacterial osteomyelitis. Infect Dis (London Engl) 2015;47:673-85.
5. Garcia DC, Sandoval-Sus J, Razzaq K, Young L. Vertebral osteomyelitis caused by Mycobacterium abscessus. BMJ Case Rep 2013;2013. pii: Bcr2013009597.
6. Kim CJ, Kim UJ, Kim HB, Park SW, Oh MD, Park KH, et al. Vertebral osteomyelitis caused by non-tuberculous mycobacteria: Predisposing conditions and clinical characteristics of six cases and a review of 63 cases in the literature. Infect Dis (Lond) 2016;48:509-16.
7. McCarthy EF, Dorfman HD. Idiopathic segmental sclerosis of vertebral bodies. Skeletal Radiol 1982;9:88-91.
8. Russell AS, Percy JS, Lentle BC. Vertebral sclerosis in adults. Ann Rheum Dis 1979;38:18-22.
9. Aithala JP. Role of percutaneous image guided biopsy in spinal lesions: Adequacy and correlation with MRI findings. J Clin Diagn Res 2016;10:RC11-5.
10. Rimondi E, Staals EL, Errani C, Bianchi G, Casadei R, Alberghini M, et al. Percutaneous CT-guided biopsy of the spine: Results of 430 biopsies. Eur Spine J 2008;17:975-81.
11. Kato S, Murakami H, Demura S, Yoshioka K, Hayashi H, Yokogawa N, et al. Vertebral osteomyelitis caused by Mycobacterium abscessus surgically treated using antibacterial iodine-supported instrumentation. Case Rep Orthop 2014;2014:197061.
12. Ryu YJ, Koh WJ, Daley CL. Diagnosis and treatment of nontuberculous mycobacterial lung disease: Clinicians’ perspectives. Tuberc Respir Dis (Seoul) 2016;79:74-84.
 |
 |
 |
 |
| Dr. Kunal Shah | Dr. Gaurang Atodaria |
Dr. Milind Patwardhan |
Dr. Abhay Nene |
| How to Cite This Article: Shah K, Atodaria G, Patwardhan M, Nene A. Mycobacteria Intracellulare Spondylodiscitis Presenting as Progressive Consecutive Vertebral Sclerosis: A Case Report. Journal of Orthopaedic Case Reports 2017 Nov-Dec; 7(6): 89-92. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com