[box type=”bio”] Learning Point for the Article: [/box]
Gluteal muscle necrosis is an uncommon yet potentially devastating orthopedic consequence of pelvic arterial embolization.
Case Report | Volume 8 | Issue 3 | JOCR May – June 2018 | Page 23-27| Michelle C O’Brien, Benjamin A Schell, Harrison Lands, Jonathon M Spanyer, Madhusudhan R Yakkanti. DOI: 10.13107/jocr.2250-0685.1092
Authors:
Michelle C O’Brien[1], Benjamin A Schell[2], Harrison Lands[3], Jonathon M Spanyer[4], Madhusudhan R Yakkanti[4]
[1]University of Cincinnati, Department of Orthopedic Surgery, Cincinnati, Ohio, USA.
[2]University of Texas Southwestern, Department of Orthopedic Surgery, Dallas, Texas, USA.
[3]University of Virginia School of Medicine, Charlottesville, Virginia, USA.
[4]University of Louisville, Department of Orthopedic Surgery, Louisville, Kentucky, USA.
Address of Correspondence:
Dr. Jonathon MSpanyer,
Department of Orthopaedic Surgery, University of Louisville School of Medicine, 550 S. Jackson Street, 1st FL, ACB, Louisville, Kentucky – 40292, USA.
E-mail: jspanyer@gmail.com
Abstract
Introduction: Traumatic pelvic injuries causing retroperitoneal bleeding can be managed with angiographic embolization. This procedure carries a small but potentially devastating risk of gluteal muscle necrosis.
Case Report: An 18-year-old trauma patient suffered from massive gluteal muscle necrosis following angiographic embolization for hemorrhage from pelvic fracture was reported.
Conclusion: To limit morbidity and mortality, the orthopedic surgeon should have a high suspicion for gluteal muscle necrosis to allow for early diagnosis and then treatment with decompression and debridement.
Keywords: Orthopedic, trauma, gluteus, gluteal, necrosis, embolization, retroperitoneal bleeding.
Introduction
Traumatic pelvic injuries resulting in retroperitoneal bleeding have widely been managed by angiographic localization and embolization of vessels. Commonly, this procedure employs the use of commercially available foams or coils. Angiographic embolization, first described by Margolies et al. in 1972 [1], has been deemed a safe and effective way to control hemorrhage caused by pelvic fracture [2, 3]. While they are uncommon and even less frequently reported, multiple episodes of gluteal muscle necrosis as a result of embolization have been published in the literature [4]. We report a case of massive gluteal muscle necrosis following angiographic embolization for the treatment of hemorrhage after pelvic fracture in an 18-year-old trauma patient, along with the results of a review of the available literature. The purpose of the present report is to highlight the morbidity, presentation, and management options associated with this uncommon yet potentially devastating orthopedic consequence after pelvic arterial embolization.
Case Report
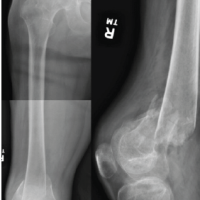
The authors obtained the patient’s informed written consent for print and electronic publication of this case report. An 18-year-old male collegiate bound football lineman was an unrestrained driver in a rollover motor vehicle accident with resulting prolonged extrication and a positive blood alcohol screen during the summer of 2012. He was intubated at the scene and taken to a Level-1 trauma center. The patient had no other past medical history. At presentation, he was found to have multiple fractures, including an open book pelvic fracture with complete disruption of the posterior sacroiliac complex resulting in both vertical and rotational instability of the left hemipelvis with associated pubic symphysis diastasis and left greater than right sacroiliac joint disruption (Fig. 1a).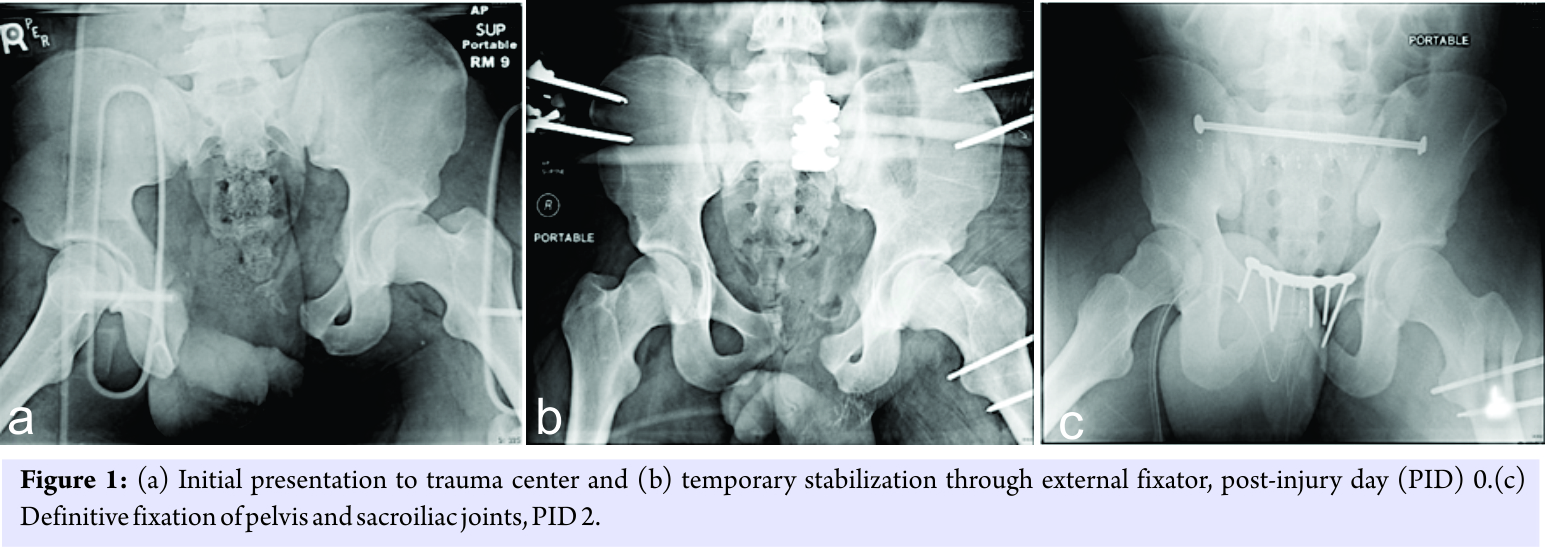 He sustained a concomitant left open comminuted femoral shaft fracture and a left distal tibia shaft fracture. His systolic blood pressure was in the 80s on admission, he was tachycardic, and the focused assessment with sonography for trauma scan was positive in the pelvic windows. The patient’s pelvis was bound with a sheet and secured using hemostats. Pulses were detected with Doppler ultrasound in the bilateral lower extremities. Due to poor response to initial fluid bolus and sustained tachycardia, he was taken to the angiography suite where significant slowing of flow within the left superior gluteal and left internal pudendal arteries with radiographic blush was found. This was thought to be due to vasospasm versus distal arterial injury, and empiric Gelfoam embolization (Pfizer Inc., New York) of the left internal iliac artery was performed (Fig. 2a and b).
He sustained a concomitant left open comminuted femoral shaft fracture and a left distal tibia shaft fracture. His systolic blood pressure was in the 80s on admission, he was tachycardic, and the focused assessment with sonography for trauma scan was positive in the pelvic windows. The patient’s pelvis was bound with a sheet and secured using hemostats. Pulses were detected with Doppler ultrasound in the bilateral lower extremities. Due to poor response to initial fluid bolus and sustained tachycardia, he was taken to the angiography suite where significant slowing of flow within the left superior gluteal and left internal pudendal arteries with radiographic blush was found. This was thought to be due to vasospasm versus distal arterial injury, and empiric Gelfoam embolization (Pfizer Inc., New York) of the left internal iliac artery was performed (Fig. 2a and b).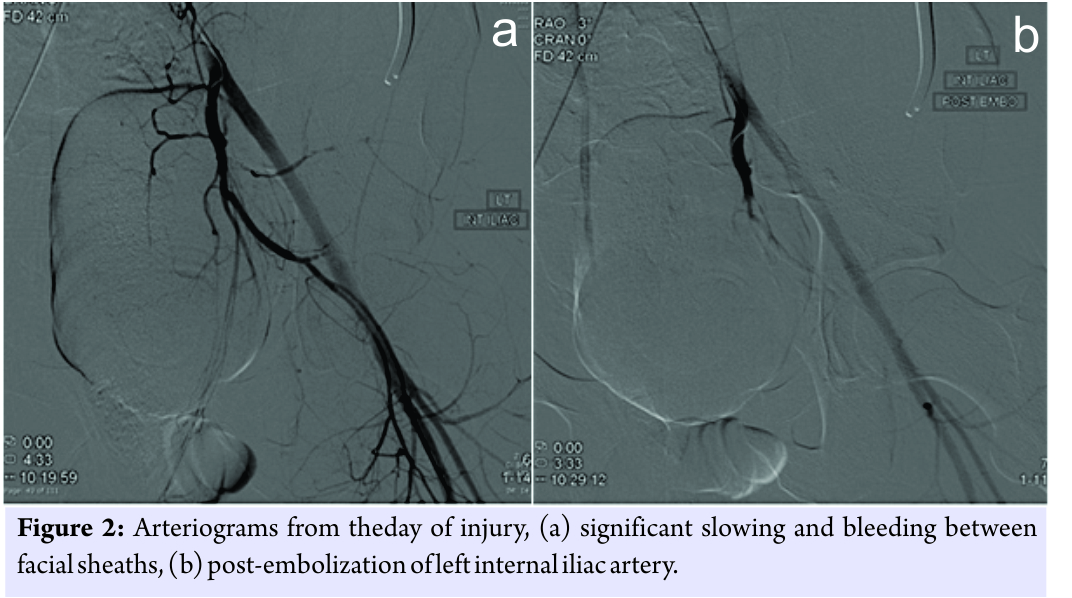 His hypotension and tachycardia subsequently stabilized, and his hemodynamic instability began to respond appropriately to resuscitation. The pelvic fractures were temporarily stabilized post-embolization through an external fixator (Hoffman III type, Stryker, Michigan, Fig. 1b), along with the left femoral shaft fracture on post-injury day (PID) 0. The patient underwent definitive fixation of the pelvis and both sacroiliac joints through symphysis plating and sacroiliac screws (Fig.1c), respectively, as well as left tibia intramedullary nailing on PID 2. On PID 4, the patient underwent definitive fixation of the left femur through intramedullary nailing. The patient remained intubated post-operatively until PID 6 and was then transferred out of the Intensive Care Unit on PID 8 to a transitional care unit. The patient’s wounds were followed through out his hospital course. Incisions remained clean and dry throughout his hospital stay. He was intermittently febrile throughout his admission. Based on an increasing lymphocyte count on routine daily collection, a computed tomography (CT) of the pelvis on PID 10 was obtained showing evidence of a 15cm diameter simple-appearing fluid collection containing scant gas collection located lateral to the left hip (Fig. 3a and b) near the area of surgical fixation.
His hypotension and tachycardia subsequently stabilized, and his hemodynamic instability began to respond appropriately to resuscitation. The pelvic fractures were temporarily stabilized post-embolization through an external fixator (Hoffman III type, Stryker, Michigan, Fig. 1b), along with the left femoral shaft fracture on post-injury day (PID) 0. The patient underwent definitive fixation of the pelvis and both sacroiliac joints through symphysis plating and sacroiliac screws (Fig.1c), respectively, as well as left tibia intramedullary nailing on PID 2. On PID 4, the patient underwent definitive fixation of the left femur through intramedullary nailing. The patient remained intubated post-operatively until PID 6 and was then transferred out of the Intensive Care Unit on PID 8 to a transitional care unit. The patient’s wounds were followed through out his hospital course. Incisions remained clean and dry throughout his hospital stay. He was intermittently febrile throughout his admission. Based on an increasing lymphocyte count on routine daily collection, a computed tomography (CT) of the pelvis on PID 10 was obtained showing evidence of a 15cm diameter simple-appearing fluid collection containing scant gas collection located lateral to the left hip (Fig. 3a and b) near the area of surgical fixation.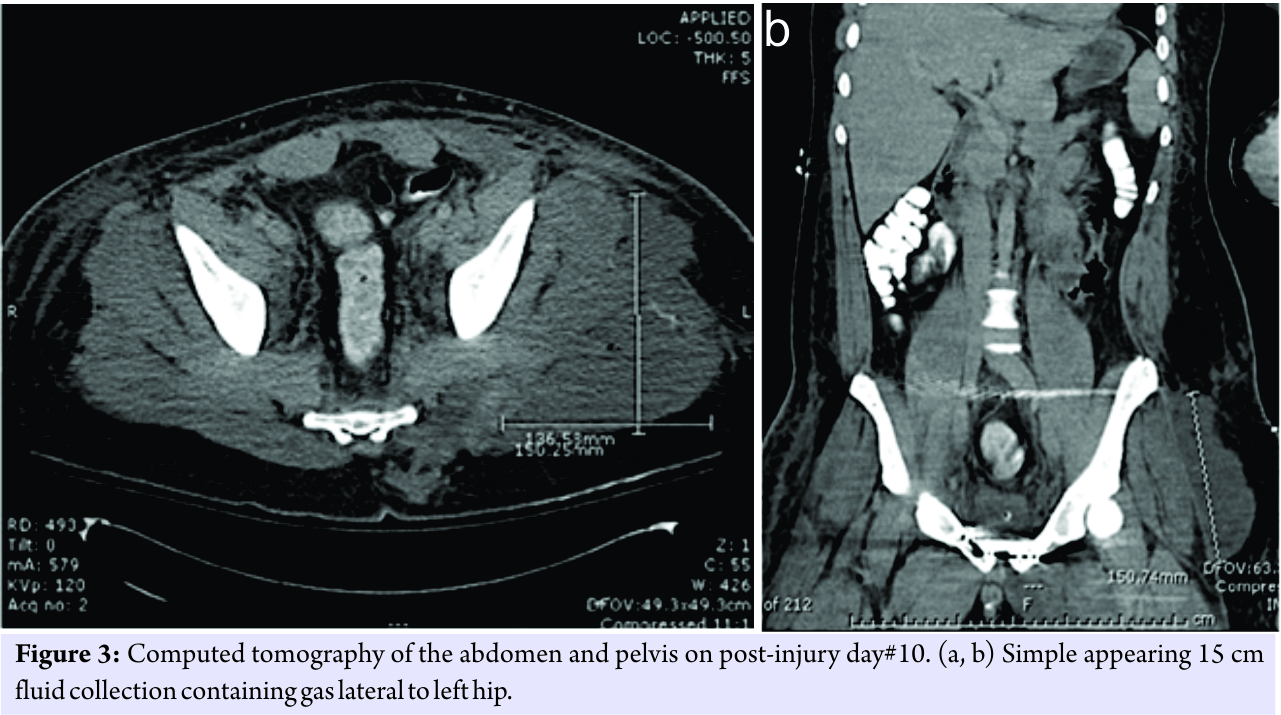 These changes were considered to be appropriate post-operative changes consistent with his percutaneous skeletal fixation of the sacroiliac joint. No clinical evidence of infection was apparent on this day, with the exception of an elevated white blood cell count of 22.9, which had been trending upward from 14.4 on PID 8. He was therefore managed with observation at this time, and the general surgery trauma team was advised by orthopedics that the cause of the leukocytosis was likely not related to the fluid collection noted on CT scan in the gluteal area. The patient progressed as expected over the next few days and on the day of discharge, and 15 days after injury, the first evidence of minimal serous drainage was observed from the patient’s left hip/buttock wound at the site of percutaneous insertion of the left sacroiliac screw. A scant amount of drainage was noted from the wound, causing minimal soiling of the patient’s sheets. No foul smell was present, and there was no evidence of purulence. No fluid could be expressed from the wound. It was believed that this could be managed expectantly with local wound care, as the wound was without erythema or induration. The patient was therefore discharged to a rehabilitation center on PID 15. In the rehabilitation facility, he continued to have drainage from the left buttock area in spite of local wet to dry wound care, and he developed early signs of wound margin epidermolysis.
These changes were considered to be appropriate post-operative changes consistent with his percutaneous skeletal fixation of the sacroiliac joint. No clinical evidence of infection was apparent on this day, with the exception of an elevated white blood cell count of 22.9, which had been trending upward from 14.4 on PID 8. He was therefore managed with observation at this time, and the general surgery trauma team was advised by orthopedics that the cause of the leukocytosis was likely not related to the fluid collection noted on CT scan in the gluteal area. The patient progressed as expected over the next few days and on the day of discharge, and 15 days after injury, the first evidence of minimal serous drainage was observed from the patient’s left hip/buttock wound at the site of percutaneous insertion of the left sacroiliac screw. A scant amount of drainage was noted from the wound, causing minimal soiling of the patient’s sheets. No foul smell was present, and there was no evidence of purulence. No fluid could be expressed from the wound. It was believed that this could be managed expectantly with local wound care, as the wound was without erythema or induration. The patient was therefore discharged to a rehabilitation center on PID 15. In the rehabilitation facility, he continued to have drainage from the left buttock area in spite of local wet to dry wound care, and he developed early signs of wound margin epidermolysis.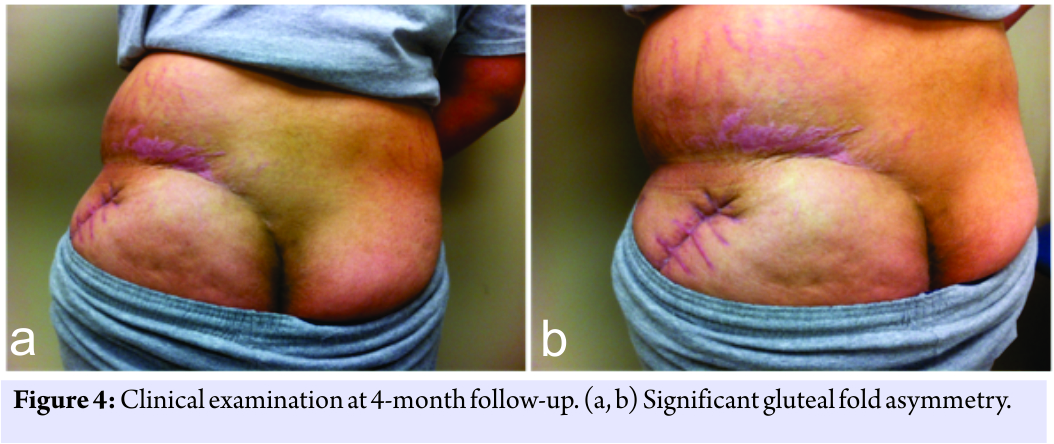 On PID 22, he was readmitted to the hospital. At this time, there was evidence of increasing drainage, marginal erythema, induration, and epidermolysis adjacent to the wound edge, as well as clinical evidence of early sepsis. He was started on intravenous vancomycin and underwent local debridement of his left hip/buttock wound. Intraoperatively, the wound was noted to have evidence of cavitation, extending posterior to the greater trochanter, with significant fat necrosis and epidermolysis. He was monitored closely and scheduled for repeat debridement. A repeat CT scan at this time noted questionable intramuscular abscess formation, and an ill-defined collection of fluid and gas in the left gluteal musculature. On PID 24, he underwent aggressive repeat surgical debridement of left hip where massive gluteal muscle necrosis was identified. Wound and tissuecultures from the left hip, obtained on PID 22 and 24, respectively, were positive for Proteus mirabilis, Serratiamarcescens, and Klebsiella pneumoniae. He underwent a third surgical debridement of the left hip wound, and a drain was placed on PID 25. He was continued on vancomycin for 8 days with piperacillin/tazobactam added for 10 days. The wound was noted on PID29 to have no erythema or drainage with a significant decrease in swelling, yet continued induration of the abductor compartment. He progressed with physical therapy and recovered as anticipated from his traumatic injuries.He was seen for 4-month follow-up where significant gluteal fold asymmetry on the left side consistent with necrosis and atrophy was identified (Fig. 4a and b). Although he had significant gains in the strength of his left hip and buttock area, he continued to ambulate with a Trendelenburg gait. His orthopedic fractures healed, but to date, he has been unable to return to competitive football due to sustained weakness, particularly of the left hip and buttock area.
On PID 22, he was readmitted to the hospital. At this time, there was evidence of increasing drainage, marginal erythema, induration, and epidermolysis adjacent to the wound edge, as well as clinical evidence of early sepsis. He was started on intravenous vancomycin and underwent local debridement of his left hip/buttock wound. Intraoperatively, the wound was noted to have evidence of cavitation, extending posterior to the greater trochanter, with significant fat necrosis and epidermolysis. He was monitored closely and scheduled for repeat debridement. A repeat CT scan at this time noted questionable intramuscular abscess formation, and an ill-defined collection of fluid and gas in the left gluteal musculature. On PID 24, he underwent aggressive repeat surgical debridement of left hip where massive gluteal muscle necrosis was identified. Wound and tissuecultures from the left hip, obtained on PID 22 and 24, respectively, were positive for Proteus mirabilis, Serratiamarcescens, and Klebsiella pneumoniae. He underwent a third surgical debridement of the left hip wound, and a drain was placed on PID 25. He was continued on vancomycin for 8 days with piperacillin/tazobactam added for 10 days. The wound was noted on PID29 to have no erythema or drainage with a significant decrease in swelling, yet continued induration of the abductor compartment. He progressed with physical therapy and recovered as anticipated from his traumatic injuries.He was seen for 4-month follow-up where significant gluteal fold asymmetry on the left side consistent with necrosis and atrophy was identified (Fig. 4a and b). Although he had significant gains in the strength of his left hip and buttock area, he continued to ambulate with a Trendelenburg gait. His orthopedic fractures healed, but to date, he has been unable to return to competitive football due to sustained weakness, particularly of the left hip and buttock area.
Discussion
Pelvic ring injuries, particularly those with significant symphyseal diastases, have been reported to be a major source of blood loss with mortality ranging between 8.8% and 35.5% [5]. Patients in these situations require multidisciplinary care, and embolization of arterial bleeding caused by trauma to the pelvis may constitute a life-saving procedure. Lopez reported a 25% mortality rate in patients who were embolized before exploratory laparotomy, compared to 60% mortality rate in those who underwent transcatheter arterial embolization (TAE) after their exploratory surgery [6]. The decrease in mortality is unfortunately accompanied by the possibility of life-altering morbidities. Many complications have been described, such as rectal necrosis, gait change, neurologic deficits, sexual dysfunction, and skin necrosis [4, 5, 7, 8, 9, 10, 11]. The authors present a detailed illustrative case of massive gluteal necrosis after iliac arterial embolization in a polytrauma patient in an effort to highlight this reported but uncommonly considered consequence of embolization, as well as to further discuss presentation and management options associated with the care of these patients. In 2010, DuBose et al. reported gluteal necrosis to occur in up to 3% of cases following internal iliac artery embolization [12]. The authors warned of the potential mortality if misdiagnosed or attributed to another source such as contusion or pressure ulcer [13]. The proposed mechanism of gluteal muscle necrosis described by Kato et al. begins with ligation of the superior gluteal artery or its tributaries near its anastomosis with the profunda femoris artery, blocking the perforating branches to the majority of the gluteal musculature. This results in the rapid onset of ischemia and necrosis [14]. Subsequent renal failure as a result of rhabdomyolysis may ensue particularly in the trauma patient already under extraordinary physiologic stress. Compression of the gluteal area while lying supine may be more poorly tolerated in these patients, potentiating the effect on the residual blood supply to the area. It remains unclear whether selective arterial embolization decreases the risk of gluteal muscle necrosis compared to a non-selective approach for TAE. Cases of muscle or skin necrosis have been described following both methods of embolization [5, 7, 10, 12, 14]. As the incidence remains rare, only small case series have been reported formally. In 2000, Velmahos et al. reviewed 30 patients that were safely treated with non-selective embolization. Auerbach et al. reported on 20 patients, 18 with selective TAE, who showed no evidence of gluteal necrosis or other complications after treatment[2,15]. The true incidence of gluteal necrosis after internal iliac arterial embolization may be more common than reported, as a subset of patients likely exist with subclinical disease, who ultimately go on to recover without significant sequella. Making the diagnosis of gluteal necrosis without overlying skin necrosis can also prove challenging. Yasumura et al. have shown the utility of magnetic resonance imaging to detect subclinical signs of gluteal area necrosis before the development of symptoms [5]. Early diagnosis may afford the orthopedic surgeon an opportunity for surgical debridement and tissue salvage, thereby limiting associated renal failure as a result of overwhelming rhabdomyolysis. Prevention of gluteal necrosis after internal iliac arterial embolization has proven challenging. This stems in part from the uncommon nature of the disease and its clinical sequelae, as well as the often critical nature of patients in uncompensated hemorrhagic shock requiring life-saving intervention who present with gluteal necrosis. In the absence of prospective studies and the paucity of reported cases and treatment regimens, a clear consensus for management remains unclear. In spite of this, for the orthopedic surgeon, maintaining a high clinical suspicion of this uncommon condition may result in early diagnosis and treatment with decompression and debridement of the affected area, there by limiting associated morbidity and mortality in the orthopedic trauma patient population.
Conclusion
As the case report illustrates, gluteal muscle necrosis is a rare but serious consequence of internal iliac arterial embolization for retroperitoneal bleeding after traumatic pelvic injury. Although there is not a consensus on the condition’s management, early diagnosis is critical to allow treatment with surgical debridement and tissue salvage to limit sequelae such as renal failure from rhabdomyolysis.
Clinical Message
Gluteal muscle necrosis is an uncommon yet potentially devastating orthopaedic consequence of pelvic arterial embolization.
References
1. Margolies MN, Ring EJ, Waltman AC, Kerr WS Jr. Baum S. Arteriography in the management of hemorrhage from pelvic fractures. N Engl J Med 1972;287:317-21.
2. Velmahos GC, Chahwan S, Hanks SE, Murray JA, Berne TV, Asensio J, et al. Angiographic embolization of bilateral internal iliac arteries to control life-threatening hemorrhage after blunt trauma to the pelvis. Am Surg 2000;66:858-62.
3. Agolini SF, Shah K, Jaffe J, Newcomb J, Rhodes M, Reed JF 3rd, et al. Arterial embolization is a rapid and effective technique for controlling pelvic fracture hemorrhage. J Trauma 1997;43:395-9.
4. Takahira N, Shindo M, Tanaka K, Nishimaki H, Ohwada T, Itoman M, et al. Gluteal muscle necrosis following transcatheter angiographic embolisation for retroperitoneal haemorrhage associated with pelvic fracture. Injury 2001;32:27-32.
5. Yasumura K, Ikegami K, Kamohara T, Nohara Y. High incidence of ischemic necrosis of the gluteal muscle after transcatheter angiographic embolization for severe pelvic fracture. J Trauma 2005;58:985-90.
6. Lopez PP. Unstable pelvic fractures: The use of angiography in controlling arterial hemorrhage. J Trauma 2007;62:S30-1.
7. Suzuki T, Shindo M, Kataoka Y, Kobayashi I, Nishimaki H, Yamamoto S, et al. Clinical characteristics of pelvic fracture patients with gluteal necrosis resulting from transcatheter arterial embolization. Arch Orthop Trauma Surg 2005;125:448-52.
8. Wells I. Internal iliac artery embolization in the management of pelvic bleeding. Clin Radiol 1996;51:825-7.
9. Duff C, Simmen HP, Brunner U, Bauer E, Turina M. Gluteal necrosis after acute ischemia of the internal iliac arteries. Vasa 1990;19:252-6.
10. Suzuki T, Kataoka Y, Minehara H, Nakamura K, Uchino M, Kawai K, et al. Transcatheter arterial embolization for pelvic fractures may potentially cause a triad of sequela: Gluteal necrosis, rectal necrosis, and lower limb paresis. J Trauma 2008;65:1547-50.
11. Tompkins RG, McCabe CJ, Burke JF, Keating MA, Wright CD. Rectal necrosis after pelvic crush injury. J Trauma 1988;28:697-9.
12. DuBose J, Inaba K, Barmparas G, Teixeira PG, Schnüriger B, Talving P, et al. Bilateral internal iliac artery ligation as a damage control approach in massive retroperitoneal bleeding after pelvic fracture. J Trauma 2010;69:1507-14.
13. Gilleard O, Stammers J, Ali F. Gluteal necrosis following pelvic fracture and bilateral internal iliac embolization: Reconstruction using a transposition flap based on the lumbar artery perforators. Int J Surg Case Rep 2012;3:86-8.
14. Kato H, Otomo Y, Homma M, Inoue J, Hasegawa E, Henmi H, et al. Gluteal soft tissue necrosis after transcatheter angiographic embolization for pelvic fracture: A Report of two cases. Eur J Trauma Emerg Surg 2007;33:301-5.
15. Auerbach AD, Rehman S, Kleiner MT. Selective transcatheter arterial embolization of the internal iliac artery does not cause gluteal necrosis in pelvic trauma patients. J Orthop Trauma 2012;26:290-5.
 |
 |
 |
 |
 |
| Dr. Michelle C O’Brien | Dr. Benjamin A Schell | Dr. Harrison Lands | Dr. Jonathon M Spanyer | Dr. Madhusudhan R Yakkanti |
| How to Cite This Article: O’Brien MC, Schell BA, Lands H, Spanyer JM, Yakkanti MR. Massive Gluteal Muscle Necrosis after Iliac Arterial Embolization in Pelvic Trauma: A Literature Review and Illustrative Case Report. Journal of Orthopaedic Case Reports 2018. May- June; 8(3): 23-27. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com