[box type=”bio”] Learning Point of the Article: [/box]
Overall, making surgical decisions in such a case can be challenging. We advocate multi- disciplinary approach and seeking further opinions from colleagues if in doubt which should help in providing the best care possible for a child.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 21-25 | Ethan Toner, Ahmad Khaled, Yacoob Nakhuda, Randeep Mohil. DOI: 10.13107/jocr.2250-0685.1352
Authors: Ethan Toner[1], Ahmad Khaled[1], Yacoob Nakhuda[2], Randeep Mohil[1]
[1]Department of Trauma and Orthopaedic, Royal Blackburn Hospital, Blackburn, BB2 3HH, England, United Kingdom,
[2]Department of Radiology, Royal Blackburn Hospital, Blackburn BB2 3HH, England, United Kingdom.
Address of Correspondence:
Dr. Ethan Toner,
Department of Trauma and Orthopaedic, Royal Blackburn Hospital, Haslingden Rd, Blackburn BB2 3HH, England, United Kingdom.
E-mail: ethantoner@doctors.org.uk.
Abstract
Introduction: The presentation of an unwell child with a short history of a limp is not an uncommon referral to the orthopaedic on-call team. In the acute setting, this is most commonly secondary to trauma or infection. An unusual differential that clinicians should be aware of is pyomyositis of the muscles around the hip joint. The rarity of our case makes this a very interesting one, with only a few other recorded cases within the UK.
Case Report: A 3-year-old Caucasian girl presented to the Paediatric ED, with 6 days’ history of general malaise, vomiting, and intermittent pyrexia. 5 days before prior to attendance, she also developed a limp, which progressively worsened until she refused to weight bear on the left side with obvious distress and pain. No history of trauma was reported. According to the parents, she had become more irritable each day. The patient had no significant medical history and no family history of congenital or developmental hip disorders. Her vital signs were in keeping with sepsis as she was tachycardiac (154) and pyrexial (38.1°). The referring GP also recorded a high temperature of 38.9°. Physical examination proved difficult, due to pain. No obvious erythema or swelling was noted around either groin or lower limb. When asked to walk, she held the left hip in flexion and refused to weight bear.
Conclusion: Treatment of pyomyositis is essential to prevent subsequent life-threatening sepsis. Intravenous antibiotics, radiologically guided or surgical drainage of the collection, or debridement may be indicated in the management. Good understanding of the anatomy surrounding the hip joint is vital. The iliopsoas muscle inserts into the lesser trochanter of the hip joint. Therefore, inflammation in the origin or along the track of the muscle can mimic a septic arthritis picture. Radiological modalities, including ultrasound and magnetic resonance imaging, should be considered, particularly when diagnostic doubt exists. Overall, making surgical decisions in such a case can be challenging. We advocate multii-disciplinary approach and seeking further opinions from colleagues if in doubt which should help in providing the best care possible for a child.
Keywords: Iliacus pyomyositis, septic arthritis, paediatric orthopaedics, non-weight bearing.
Introduction
The presentation of an unwell child with a short history of a limp is not an uncommon referral to the orthopedic on-call team. Despite this, the incidence of an acute limp in a child has been recorded in one study as <2% of all pediatric emergency department presentations [1]. In the acute setting, this is most commonly secondary to trauma or infection. An unusual differential that clinicians should be aware of is pyomyositis of the muscles around the hip joint. In the case of our patient, there was pyomyositis of the iliacus muscle. Pyomyositis is a bacterial infection of muscle, associated with purulence and abscess development. It is usually the result of hematogenous spread from Staphylococcus aureus [2]. The incidence is highest in tropical climates where it is recognized to affect children (age 2–5) and adults (age 20–45). Within the UK and similar temperate climates, it presents more commonly in immunocompromised adults, with only a few cases recorded in children [3, 4, 5]. This emphasizes the rarity of our case. A common pitfall is the incorrect diagnosis of septic arthritis, due to the striking similarities in clinical features [6]. With the aid of diagnostic magnetic resonance imaging (MRI) scanning, the correct diagnosis can be made. Treatment modalities include non-operative with intravenous (IV) antibiotics through to surgical drainage with the aim of complete resolution and functional recovery [7, 8].
Case Report
A 3-year-old Caucasian girl presented to the pediatric ED, with 6 days’ history of general malaise, vomiting, and intermittent pyrexia. 5 days before attendance, she also developed a limp, which progressively worsened until she refused to weight bear on the left side with obvious distress and pain. No history of trauma was reported. According to the parents, she had become more irritable each day. The patient had no significant medical history and no family history of congenital or developmental hip disorders. The mother of the child attributed her symptoms to a viral illness initially before things worsened. Her vital signs were in keeping with sepsis as she was tachycardiac (154) and pyrexial (38.1°). The referring GP also recorded a high temperature of 38.9°. Physical examination proved difficult, due to pain. No obvious erythema or swelling was noted around either groin or lower limb. When asked to walk, she held the left hip in flexion and refused to weight bear.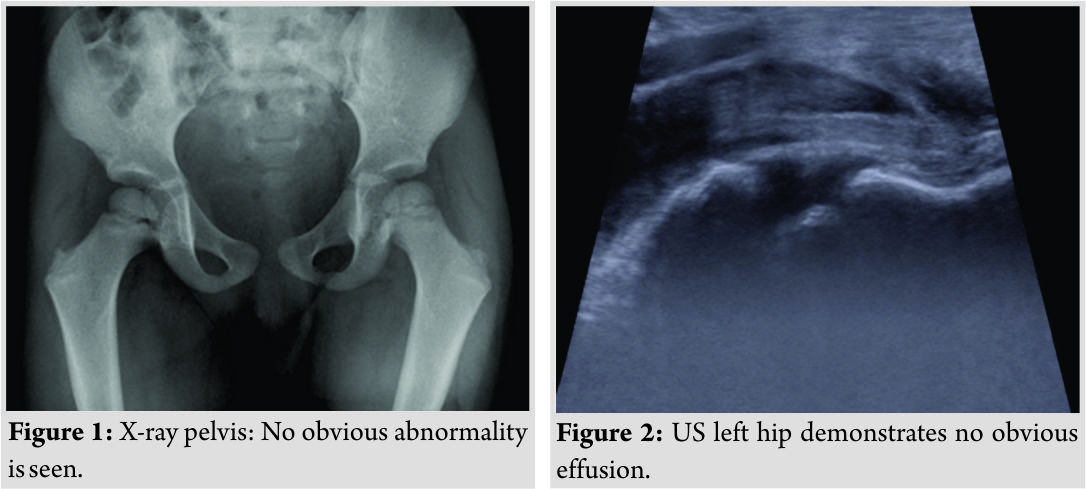
Investigations
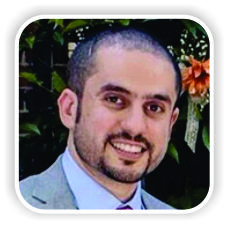
Initial laboratory studies revealed normal renal function (estimated glomerular filtration rate >90), elevated C-reactive protein (CRP) of 77, erythrocyte sedimentation rate (ESR) of 76,white cell count (WCC) of 9.3, and neutrophils of 5.0. Inflammatory markers deteriorated further during her admission with a maximum CRP of 125 and ESR of 80. Peripheral blood cultures were taken, which indicated no growth after 48h, with no causative pathogen isolated after extended culture. Pelvic X-ray and a left knee X-ray were performed to rule out any bony abnormality, and both were normal (Fig. 1). An ultrasound scan of the hips suggested a very small left-sided effusion (Fig. 2). The patient then underwent MRI abdomen and pelvis revealing approximately 1.5 × 0.9 (axial) × 4.5 cm (craniocaudal) collection, between the left iliac blade and overlying iliacus muscle, which was noted to be swollen and edematous. Inflammatory changes also tracked inferiorly into the groin (Fig. 3a-c).It was concluded that this was likely pyomyositis centered on the left iliacus muscle with a small collection.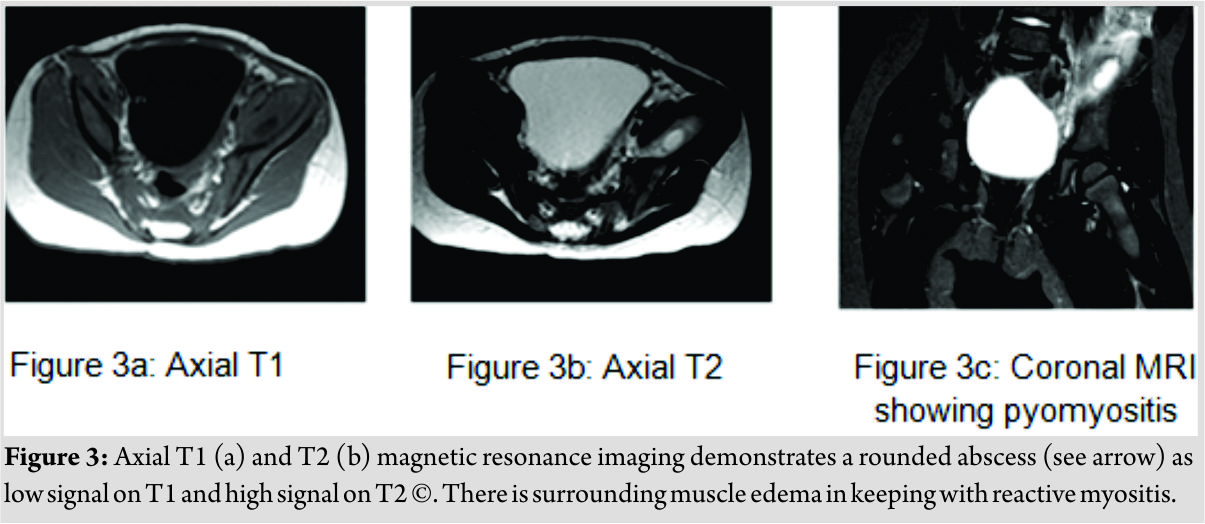
Differential diagnosis
An unwell child with a limp, in the absence of trauma, can usually be attributed to a few common differential diagnoses, such as transient synovitis, septic arthritis, or osteomyelitis. This reinforces the importance of extrapolating a concise history and knowledge of focal findings on examination. Our patient had a history of a viral illness, which preceded the onset of the limp, which may lead the clinician to think of transient synovitis. However, due to the systemic features present, this was unlikely. The Kocher criteria highlight four parameters that indicate the probability of septic arthritis (non-weight bearing, temperature >38, ESR > 40, and WCC >12). Our patient had 3 out of 4 of these and so the preliminary diagnosis of septic arthritis was made [9]. With normal X-rays and an insignificant hip effusion on ultrasound, osteomyelitis was considered. Following consultant orthopaedic and radiologist discussion, urgent MRI was indicated to rule out osteomyelitis and to look for other potential pathology, before any joint aspiration or washout [10].
Treatment
On the basis of possible septic arthritis, the patient was commenced on IV antibiotics according to trust antimicrobial guidelines (flucloxacillin 5 mg/kg). She was consented for the left hip aspiration ± proceed to open washout. On review the following morning, she was hemodynamically stable and had been apyrexial since admission. The decision was made to proceed with an ultrasound scan first before possible aspiration (Fig. 2). With the MRI findings to hand and following discussion with the pediatric surgeons, it was felt that the collection did not require surgical intervention (Fig. 3a-c). She continued with IV antibiotics until both her pain and inflammatory markers reduced significantly, and on further liaison with microbiology, she was stepped down to oral antibiotics (flucloxacillin 250 mg/5 ml), which she responded to although exact pathogen was not identified. An oral antibiotic course of a period of 3 weeks was to be completed on discharge, with outpatient follow-up arrangements.
Outcome and follow-up
Outpatient clinic follow-up was organized. Following discharge, she had been at home for 10 days, with no concerns raised by parents, was walking normally, eating and drinking well and with no recurrences of any fever. On arrival to clinic, blood investigations were repeated. CRP was <5 and WCC of 5.6. There was no indication for repeat imaging at this time, and she was to continue with the oral antibiotics for a further 11 days. Another safety net appointment had been arranged for 2 weeks times if required.
Discussion
This particular case of a limping child highlights the importance of a number of key fundamentals to establish the correct diagnosis and to potentially avoid unnecessary surgery. First, the clinician must keep in mind the possibility of other hip pathologies, other than septic arthritis. The appropriate and timely use of imaging modalities is important [11]. All children in pain present barriers to examination, and this must be acknowledged by the treating clinicians, not to cause added distress. The rarity of our case makes this a very interesting one, with only a few other recorded cases within the UK [5, 12]. Similarities between the presentation of septic arthritis and pyomyositis often lead the clinician to believe in the more common diagnosis of septic arthritis. Differentiation between the two is vital as septic arthritis of the hip joint would often require an extensive joint washout, thus hopefully preventing irreversible joint destruction. Pyomyositis if advanced requires surgical drainage of abscess development. If the correct diagnosis is not determined, this can result in adverse outcomes for a potentially treatable entity. Although in our case conservative methods were deemed sufficient for treatment, and ultimately antibiotic therapy for pyomyositis and septic arthritis similar [6]. Septic arthritis causes pain in the hip affecting a range of movement in all directions on assessment [6]. Pyomyositis of the iliacus muscle usually tends to present with pain more noticeable on passive extension of the hip joint, related to stretching of the muscle itself. The iliacus muscle sits in the posterior abdominal wall and makes up the lateral part of the iliopsoas, together with the psoas major. The main flexor of the hip. Its origin is from the iliac fossa and the anterior inferior iliac spine, with insertion on to the lesser trochanter of the femur. The iliopsoas muscle is one of the posterior relations, for much of the abdominal contents, including the diaphragm, kidneys, renal vessels, and genitofemoral nerve. To the right, it is in close proximity to both the cecum and appendix, with the sigmoid colon on the left. Behind the iliopsoas, lies the quadratus lumborum muscle. As the iliopsoas enters the thigh below the inguinal ligament, it forms part of the floor of the femoral triangle [12]. Presenting symptoms can vary, such as abdominal, thigh, and back pain all corresponding to the intricate anatomy of the pelvis [12]. Close proximity to the femoral nerve and the lateral cutaneous nerve of the thigh can lead to neuropathy as a symptom [13]. Through the use of MRI scan, we were able to establish a definitive diagnosis. MRI allowed us to identify the inflammatory changes and abscess formation, proving its value for identifying soft tissue infections. Abnormal signal intensity of the iliacus muscle along with inflammatory changes tracking down into the groin confirmed the diagnosis of pyomyositis, making MRI scanning the investigative tool of choice for pyomyositis and in excluding other differentials when in doubt [7, 14]. Of note with our case, the small collection over the iliacus muscle did not require surgical drainage. Immunocompromised patients have the highest incidence of pyomyositis in temperate climates. Associated with increased likelihood in cases complicated by HIV, diabetes, corticosteroids, IV drug usage, recent surgery or local trauma. There was no obvious evidence of recurrent infections or medical history suggestive of immunodeficiency in our patient. Many pathogens have been recorded that can be attributed to the resultant infection. These include bacterial, viral, fungal, and parasitic. Infections can be monomicrobial or mixed polymicrobial [15]. Despite this, Staphylococcus aureus has been found to be responsible in the majority of cases. Reports suggest up to 90% of cases across all climates and ages [5, 12, 15]. Treatment of pyomyositis is essential to prevent subsequent life-threatening sepsis. Treatment options include IV antibiotics, radiologically guided or surgical drainage of the collection, and in some cases, debridement which may be indicated. Surgical intervention for open drainage is reserved for complex cases or when percutaneous drainage has failed. This can be performed through an anterolateral extraperitoneal approach, and an incision along the iliac crest allows access to both the iliacus and psoas muscles [16]. Although this is a rare procedure to be performed in a pediatric population and would require input from pediatric general and orthopedic surgeons. One may want to consider image-guided drainage of the abscess to avoid a major open procedure if possible. The safest way when considering surgical management is to have a multidisciplinary approach and to preserve surgery for cases where patients do not respond to less invasive management options. Antibiotic choice and treatment duration are variable, with limited evidence available. It is considered that the antibiotic regimen should consider likely organisms involved and local sensitivities and resistance traits. Antibiotic therapy can then be targeted specifically following pathogen identification through Gram stain and cultures [15]. It is noted that our patient did not have any positive blood culture results and was continued on empirical antibiotic treatment, to which she responded very well. She made a full recovery with non-operative management, with empirical IV antibiotics alone.
Conclusion
Treatment of pyomyositis is essential to prevent subsequent life-threatening sepsis. IV antibiotics, radiologically guided or surgical drainage of the collection, or debridement may be indicated in the management. Examining a child in pain can be difficult. One should be very thorough with the clinical history and examination. Being aware of other differentials in the diagnosis is important. Good understanding of the anatomy surrounding the hip joint is vital. The iliopsoas muscle inserts into the lesser trochanter of the hip joint. Therefore, inflammation in the origin or along the track of the muscle can mimic a septic arthritis picture. Radiological modalities, including ultrasound and magnetic resonance imaging, should be considered, particularly when diagnostic doubt exists.
Clinical Message
Overall, making surgical decisions in such a case can be challenging. We advocate a multidisciplinary approach and seeking further opinions from colleagues if in doubt which should help in providing the best care possible for a child.
References
1. Fischer SU, Beattie TF. The limping child: Epidemiology, assessment and outcome. J Bone Joint Surg 1999;81-B:1029-34.
2. Chauhan S, Jain S, Varma S, Chauhan SS. Tropical pyomyositis (myositis tropicans): Current perspective. Postgrad Med J 2004;80:267-70.
3. Hall RL, Callaghan JJ, Moloney E, Martinez S, Harrelson JM. Pyomyositis in a temperate climate. Presentation, diagnosis, and treatment. J Bone Joint Surg Am 1990;72:1240-4.
4. Gibson RK, Rosenthal SJ, Lukert BP. Pyomyositis. Increasing recognition in temperate climates. Am J Med 1984;77:768-72.
5. Peckett WR, Butler-Manuel A, Apthorp LA. Pyomyositis of the iliacus muscle in a child. J Bone Joint Surg Br 2001;83:103-5.
6. Chen WS, Wan YL. Iliacus pyomyositis mimicking septic arthritis of the hip joint. Arch Orthop Trauma Surg 1996;115:233-5.
7. Theodorou SJ, Theodorou DJ, Resnick D. MR imaging findings of pyogenic bacterial myositis (pyomyositis) in patients with local muscle trauma: Illustrative cases. EmergRadiol 2007;14:89-96.
8. Chiedozi LC. Pyomyositis. Review of 205 cases in 112 patients. Am J Surg 1979;137:255-9.
9. Kocher MS, Mandiga R, Zurakowski D, Barnewolt C, Kasser JR. Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children. J Bone Joint Surg Am 2004;86-A:1629-35.
10. Sukswai P, Kovitvanitcha D, Thumkunanon V, Chotpitayasunondh T, Sangtawesin V, Jeerathanyasakun Y, et al. Acute hematogenous osteomyelitis and septic arthritis in children: Clinical characteristics and outcomes study. J Med Assoc Thai 2011;94Suppl 3:S209-16.
11. Mitsionis GI, Manoudis GN, Lykissas MG, Sionti I, Motsis E, Georgoulis AD, et al.Pyomyositis in children: Early diagnosis and treatment. J PediatrSurg 2009;44:2173-8.
12. Martin A, Aftab S, Grewal U, Pampiglione T, Bracewell T, Macerola A. Infectious myositis of the iliacus muscle: An important differential in the unwell child with a limp. J Case Rep Images Surg 2015;1:17-20.
13. Pai VS, Yee E, Lawson D, Curtis G. Iliacus pyomyositis with involvement of lateral cutaneous nerve of the thigh. N Z Med J 1994;107:378-9.
14. Yuh WT, Schreiber AE, Montgomery WJ, Ehara S. Magnetic resonance imaging of pyomyositis. Skeletal Radiol 1988;17:190-3.
15. Brook I. Microbiology and management of myositis. IntOrthop 2004;28:257-60.
16. Khedkar K, Sharma C, Kumbhar V, Waghmare M, Dwivedi P, Gandhi S, et al. Management of paediatric psoas abscess: Our experience. J PediatrNeonatIndivid Med 2018;7:e070213.
 |
 |
 |
 |
| Dr. Ethan Toner | Dr. Ahmad Khaled | Dr. Yacoob Nakhuda | Dr. Randeep Mohil |
| How to Cite This Article: Toner E, Khaled A, Nakhuda Y, Mohil R. The Limping Child, a Rare Differential: Pyomyositis of the Iliacus Muscle -A Case Report. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9(2): 21-25. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




