[box type=”bio”] Learning Point of the Article: [/box]
Primary TKA for proximal tibia fracture is an option for elderly patients based on a clinical and radiological presentation the surgeon can opt for total knee arthroplasty even in younger individuals.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 72-75 | Santhosh Srinivasan S, UThygarajan, D Gokul Raj. DOI: 10.13107/jocr.2250-0685.1378
Authors: Santhosh Srinivasan S[1], UThygarajan[1], D Gokul Raj[1]
[1]Department of Orthopedics, Sri Ramachandra Medical College, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. Santhosh Srinivasan,
Department of Orthopedics, Sri Ramachandra Medical College, Porur, Chennai, Tamil Nadu, India.
E-mail: santh5550@gmail.com
Abstract
Introduction: Post-traumaticOsteoarthritis osteoarthritis of the knee is a common complication following malunited proximal tibia fractures treated by internal fixation. Delayed treatment failed internal fixation native splinting can lead to malunited tibia plateau fractures.
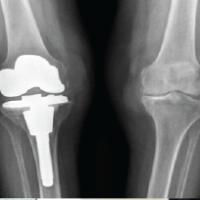
Case Report: We report a 10-month-old malunited proximal tibia fracture with osteoarthritis of the knee joint who had underwent native splinting. The patient presented with complaints of pain over the left knee joint and inability to weight bear over his left leg for the past ten 10months. Radiographs showed malunited proximal tibia fracture. Since there were signs of osteoarthritis of the affected knee joint, it was decided to treat primarily by total knee arthroplasty. Postoperatively, the patient could walk freely without a stick and had no pain. The knee was stable and had a full range of movement.
Conclusion: Post-traumatic knee arthritis is a dreaded complication following both conservative and surgical management of proximal tibia fracture due to immobilization and knee stiffness. The primary use of total knee replacement TKR can be considered an alternative treatment for patients with intra-articular fractures of the tibia not extending past the metaphysical area to provide the patient with a stable and pain-free joint.
Keywords: Proximal tibial plateau fracture, total knee replacement, osteoarthritis knee.
Introduction
Proximal Tibial plateau fractures follows Bimodal age distribution. There are various treatment options available for displaced tibial plateau fractures, the standard of care is open reduction and internal fixation (ORIF). Post-traumatic osteoarthritis is a long-term complication of tibial plateau fractures. It has a prevalence of 21%-–44% % following fractures of the proximal tibia, patella, and distal femur [1-3]. Various etiologies have been associated with this namely mechanical imbalance due to ligamentous laxity, meniscal tears [4], and non-unions and malunions of fractures [2]. The management management of post-traumatic osteoarthritis can be divided into conservative conservative and surgical. Activity modification, anti-inflammatory medications, ambulatory assist devices, and physical therapy are the conservative management [4]. Surgical options available include oarthroscopic debridement to arthrodesis [5]. In older, lower demand patients, ORIF is potentially less favorable, delayed mobilization, and knee stiffness. Total knee arthroplasty (TKA) is an option for the treatment of end-stage PTA [6].
Case Report
A 55-year-old gentleman, presented with complaints of pain over the left knee joint and inability to weight bear over his left leg for the past ten 10 months. The patient was apparently normal 10 months ago, when he had a history of slip and fall from 10 feet height at his workplace in the month of January 2017 and sustained close injury to his left knee. The patient developed pain and inability to weight bear over his left leg. The patient initially underwent native splinting for 6 months following the injury. As patient was not relieved of his symptoms following native splinting, patient came to Sri Ramachandra Medical College Porur for further management With complaints of pain, deformity, and unable to bear weight on left leg (Fig.1). There is no history of fever, loss of appetite or any other bone injury. The patient is not a known case of diabetic mellitus, Hypertension hypertension cardiac disease tuberculosis asthma epilepsy. The patient is not a smoker or an alcoholic. Examination revealed left lower limb appears to be shorter than the right lower limb. Muscle wasting was noted over the thigh and calf region. Healed abrasion scar present over the anterior aspect of the knee joint and the distal aspect of the leg. Dilated veins present over the posterolateral and the medial aspect of the knee joint. No popliteal fossa fullness was noted. Tenderness present over medial and lateral jointline Swelling present over the anterior aspect of knee joint. Bony mass is palpable over the anteromedial and lateral aspect of the knee. Broadening and thickening present over the anterior, medial, and lateral aspect of the knee joint. Abnormal mobility was noted. The Range range of Movement movement of the knee was 20 to –70°° with fixed flexion deformity of 20°.Further movements were painful. There was no neurovascular deficit noted.
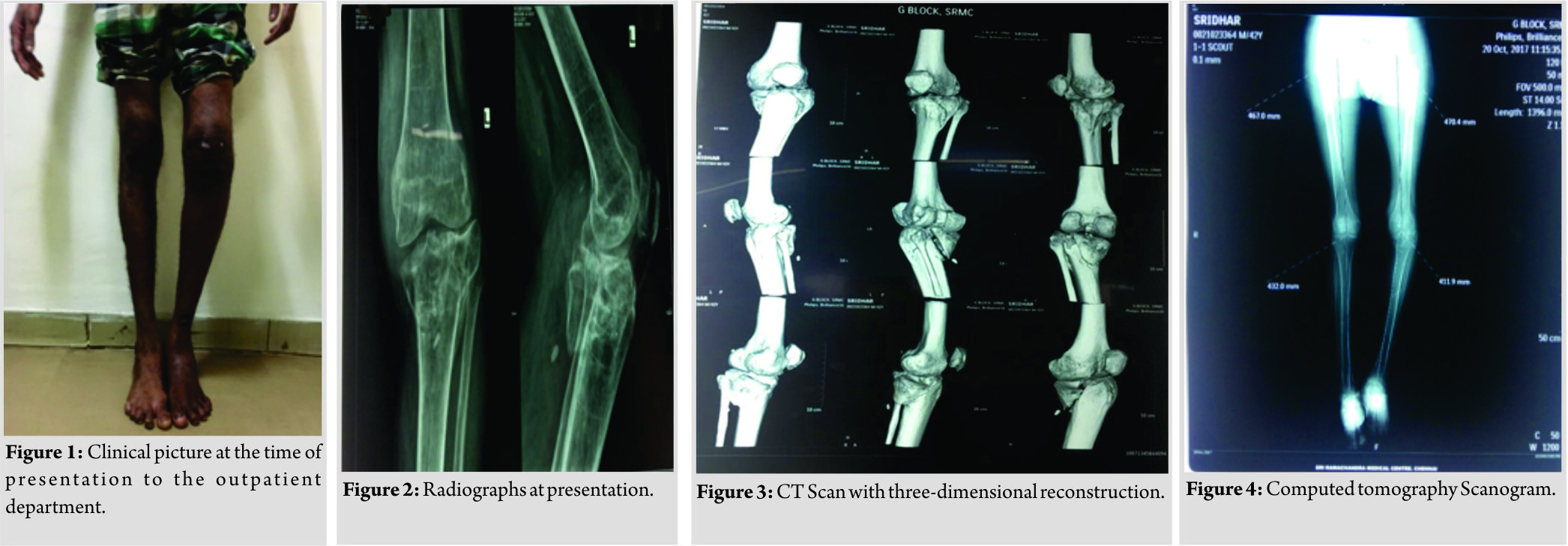
Radiographs showed comminuted malunited proximal tibia with depression over the medial condyle 1-2 cm and fracture line extending to the lateral and posterior condyle of tibia (Fig. 2). Computed tomography CT of the knee revealed that the whole of the medial condyle was depressed by more than >2 cm and the fracture line was extended into the medial and posterior condyle. (Fig. 3 and 4). There was no fracture line noted over the metaphyseal region of the shaft of the tibia. Knee joint showed significant osteoarthritis changes. Intraoperatively, we found that the articular cartilage was found to be completely damaged and there was a coronal split of the tibial plateau. The depressed medial condyle was raised and fixed with the help of of cannulated cancellous screw from the medial aspect of the tibia. (Figs. 5, and 6,). He was operated upon using a total knee prosthesis – Smith and Nephew Genesis II system with long stem tibial component and cruciate retaining femoral component. Then, appropriate femoral femoral cuts were made and and size 6 left cemented, nonmodular Genesis II cruciate retaining femoral component with Genesis II long slotted stem placed. An appropriate tibial cut made and Genesis II left nonporous tibial base plate placed. Size 5-6 13mm Genesis II dished articular insert was was placed. Movements of the knee joint were checked intraoperatively and were as found found to be satisfactory. Six 6 weeks postoperatively (Fig. 7), the patient could walk freely without a stick and had no pain. The knee was stable and had a full range of movement.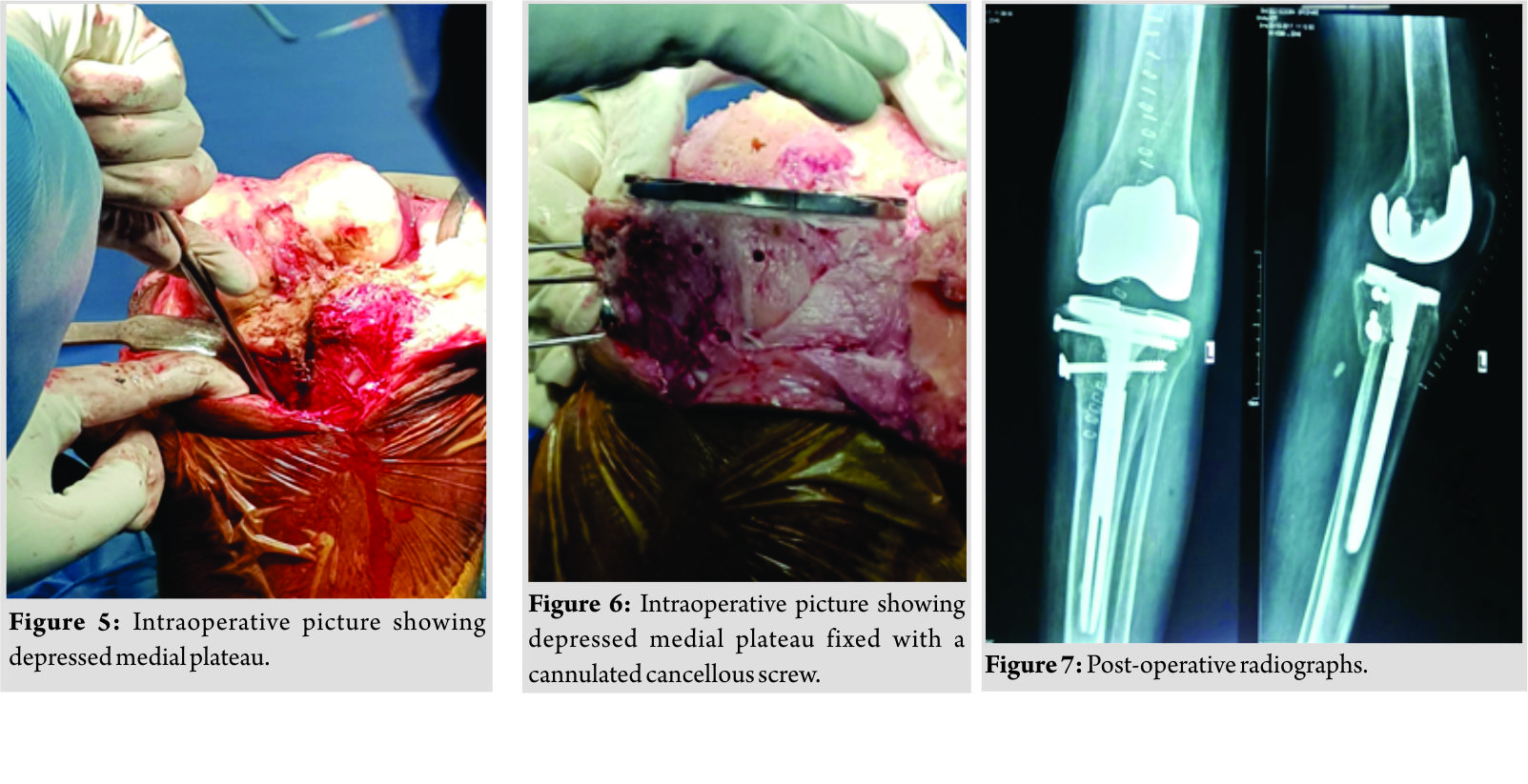
Discussion
The commonly followed method of the treatment for patients with the above history history would have been to treat with ORIF open reduction and internal fixation and autologous bone grafting. The knee would have been immobilized for four 4 weeks,and no weight bearing bearing would have been possible possible for 3-4 months. The patient was initially treated with native splinting, and there were as significant muscle wasting and fixed flexion deformity of 20°degrees of the knee joint. Further management with the usual treatment protocol will have an increased risk of developing gonarthrosis, deep vein thrombosis DVT, and significant muscle wasting necessitating total knee prosthesis [5, 6]. Hence, we planned for single stage procedure TKA Total Knee Arthroplasty, hence allowing the patient immediate mobilization and weight bearing. Knee arthroplasty has been used after failure of internal fixation of the tibial plateau [5, 7] and in patients with post-traumatic arthritis and have has given excellent results in elderly at midterm follow-up [8, 9]. Treatment with long-stemmed total knee replacement (TKR) has been suggested for fractures of the proximal tibia below an osteoarthritic knee in elderly patients [10]. The primary use of prosthesis has been recommended for the dislocated neck of femur fractures of the hip [11, 12] as well as for comminuted fractures of the proximal humerus [13] and of the distal humerus [14]. Cemented TKA total knee arthroplasty may produce excellent mid- and long-term results in patients younger than 40 years of age with end-stage arthrosis, if they are willing to modify their day to to day activities [15, 16]. In a series of 74 cases as reported by Duffy et al. [17] which had 54 patients under 55 years of age age a final Knee Society knee score of 84 points, and functional score of 60 points at 10-year follow-up was noted. The study had 18 patients only with with diagnosis of osteoarthrosis or post-traumatic arthrosis. Implant survivorship at 10 years was 99% and at 15 years was 95%. It was only after discussion and consent of the patient that TKA total knee arthroplasty was planned. The good early result was surprising. It might be that the patient before the accident was fit and had no knee arthritis, but he showed signs of gonoarthrosis from native splinting which was treated with TKR. When using this method, it is important to have at hand tibial prostheses with long shafts allowing for better fixation and cannulated cancellous screw for depressed fractures of the tibial plateau. The primary use of TKR might be considered an alternative treatment for patients with intra-articular fractures of the tibia not extending past the metaphysical area.
Conclusion
Post-traumatic osteoarthritis of the knee is common complication following proximal tibial plateau fracture. Early internal fixation and mobilization in the younger age group are is advised. Primary TKA total knee arthroplasty for proximal tibia fracture has been accepted mode of treatment in the elderly age group. In malunion with early osteoarthritis, TKA Total knee arthroplasty can be considered as an option to provide the patient with pain-free and stable mobile joint.
Clinical Message
Primary TKA total knee arthroplasty for proximal tibia fracture is an option for elderly patients Based on a clinical and radiological presentation the surgeon can opt for total knee arthhtroplasty even in younger individuals.
References
1. Larson AN, Hanssen AD, Cass JR. Does prior inasfection alter the outcome of TKA after tibial plateau fracture? Clin Orthop Relat Res 2009;467:1793-9.
2. Furman BD, Mangiapani DS, Zeitler E, Bailey KN, Horne PH, Huebner JL, et al. Targeting pro-inflammatory cytokines following joint injury: Acute intra-articular inhibition of interleukin-1 following knee injury prevents post-traumatic arthritis. Arthritis Res Ther 2014;16:R134.
3. Anderson DD, Marsh JL, Brown TD. The pathomechanical etiology of post-traumatic osteoarthritis following intraarticular fractures. Iowa Orthop J 2011;31:1-20.
4. Pickering RD. Posttraumatic arthritis. Can Fam Physician 1984;30:1511-3.
5. Saleh KJ, Sherman P, Katkin P, Windsor R, Haas S, Laskin R, et al. Total knee arthroplasty after open reduction and internal fixation of fractures of the Tibial plateau: A minimum five-year follow-up study. J Bone Joint Surg Am 2001;83-A:1144-8.
6. Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated Tibial Plateau fracture: A matched-population-based cohort study. J Bone Joint Surg Am 2014;96:144-50.
7. Softness KA, Murray RS, Evans BG. Total knee arthroplasty and fractures of the tibial plateau. World J Orthop 2017;8:107-14.
8. Ebied A, Zayda A, Marei S, Elsayed H. Medium term results of total knee arthroplasty as a primary treatment for knee fractures. SICOT J 2018;4:6.
9. Weiss NG, Parvizi J, Trousdale RT, Bryce RD, Lewallen DG. Total knee arthroplasty in patients with a prior fracture of the tibial plateau. J Bone Joint Surg Am 2003;85-A:218-21.
10. Wilkes RA, Thomas WG, Ruddle A. Fracture and nonunion of the proximal tibia below an osteoarthritic knee: Treatment by long stemmed total knee replacement. J Trauma 1994;36:356-7.
11. D’Arcy J, Devas M. Treatment of fractures of the femoral neck by replacement with the Thompson prosthesis. J Bone Joint Surg Br 1976;58:279-86.
12. Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg Br 2002;84:183-8.
13. Gambirasio R, Riand N, Stern R, Hoffmeyer P. Total elbow replacement for complex fractures of the distal humerus. An option for the elderly patient. J Bone Joint Surg Br 2001;83:974-8.
14. Levine WN, Connor PM, Yamaguchi K, Self EB, Arroyo JS, Pollock RG, et al. Humeral head replacement for proximal humeral fractures. Orthopedics 1998;21:68-73.
15. Chandler HP, Reineck FT, Wixson RL, McCarthy JC. Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am 1981;63:1426-34.
16. Dorr LD, Takei GK, Conaty JP. Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg Am 1983;65:474-9.
17. Duffy GP, Trousdale RT, Stuart MJ. Total knee arthroplasty in patients 55 years old or younger 10-to 17-year results. Clin Orthop Relat Res 1998;356:22-7.
 |
 |
| Dr. Santhosh Srinivasan S | Dr. D Gokul Raj |
| How to Cite This Article: Srinivasan S S, Thygarajan U, Gokul R D. Complex Proximal Malunited Tibial Plateau Fracture Treated Primarily by Total Knee Arthroplasty-A Case Report. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9(2):72-75. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com