[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
1. A unique technique of primary repair of ruptured patella tendon after TKA which gives satisfactory functional outcome for the patient.
2. An early repair, with a good technique and correct rehabilitation protocols gives a good outcome without complications and without any residual disability.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 15-18 | Amyn M. Rajani, Meenakshi S. Punamiya, Kareena Rajani, Khushi Rajani. DOI: 10.13107/jocr.2020.v10.i09.1886
Authors: Amyn M. Rajani[1], Meenakshi S. Punamiya[1], Kareena Rajani[1], Khushi Rajani[1]
[1]Department of Orthopaedics, Orthopaedic Arthroscopy Knee and Shoulder Clinic, 707, Panchshil Plaza, Hughes Road, Mumbai, Maharashtra. India.
Address of Correspondence:
Dr. Amyn M. Rajani,
Department of Orthopaedics, Orthopaedic Arthroscopy Knee and Shoulder Clinic, 707, Panchshil Plaza, Hughes Road, Mumbai – 400 007, Maharashtra. India.
E-mail: dramrajani@gmail.com
Abstract
Introduction: Rupture of patellar tendon following total knee arthroplasty (TKA) is a rare but disabling complication. Results of the primary repair of the patellar tendon after the TKA are associated with higher complication rates and a poor outcome. We report a rare case of traumatic patellar rupture, 5 years after the TKA managed using a primary repair with good post-operative outcome.
Case Report: A 75-year-old female was operated for sequential bilateral Grade 4 osteoarthritis. Five years after the left-sided TKA, she sustained a fall while coming down the stairs and avulsed her patellar tendon on the left side. The management in our case was done by primary repair using two techniques with augmentation using autologous semitendinosus free graft.
Conclusion: Management of a patellar tendon rupture/avulsion after TKA is unpredictable and associated with poor functional outcomes. Various methods have been described with inconsistent clinical evidences. The operating surgeon must consider the potential advantages and disadvantages of these techniques.
Keywords: Total knee replacement, patella tendon rupture, total knee arthroplasty, primary repair, augmentation.
Introduction
Extensor mechanism of knee consists of a complex system of components such as quadriceps muscle, quadriceps tendon, patella, medial and lateral retinaculum, patellofemoral and patellotibial ligaments, patellar tendon, and tibial tubercle. Integrity of each and every component of the extensor mechanism is a must for proper functioning of the knee joint and disruption of any component can render a good total knee arthroplasty (TKA) futile. Post-TKA incidence of extensor mechanism rupture is around 0.17–1.4% [1] and of patellar tendon rupture is even low (<1%) [2]. Of these, patellar tendon ruptures, though rare, have worst prognosis and maximum morbidity [3]. Recent guidelines and research emphasize on reconstruction as a standard for patellar tendon rupture [4], but we present an exceptional case of ruptured patellar tendon treated with primary repair and excellent post-operative outcomes.
Case Report
A 75-year-old female underwent bilateral sequential TKA with patellar resurfacing for Grade 4 osteoarthritis. The patient had no comorbidities. Surgeries were uneventful with good post-operative recovery and rehabilitation. Five years after the surgery, the patient had a fall from stairs and sustained a direct injury on the left knee. The patient had immediate swelling around knee with inability to extend the knee and walk without support due to severe pain on weight-bearing. The patient sought medical advice immediately. On examination, patients left knee was warm, tender, and swollen. There were swelling and skin discoloration. She was unable to actively extend her knee and knee range of motion (ROM) was painful. The patella was mobile and high riding on clinical examination. X-ray of the knee joint revealed patella alta, along with comminution at the lower end of patella suggesting an avulsion of patella tendon from the distal pole (Fig. 1). Magnetic resonance imaging of knee joint suggested patellar tendon avulsion from the distal pole.
Surgical technique
Primary repair
The patellar tendon was primarily repaired by two techniques…
1. The distal portion of the patella tendon is sutured by two fiber tapes using the Krackow locking technique. The free end of the tapes which are four in number is then arranged as one medial, two central, and one lateral (Fig. 2).
Three parallel tunnels (medial, central, and lateral) (Fig. 2a) are drilled from distal to proximal in the patella using beath pin and 4.5 mm cannulated drill bit.
The lateral free edge of the fiber tape from the beath pin is passed through the lateral tunnel, two middle fiber tapes are passed through the central tunnel, and medial tape is passed through the medial tunnel. This brings the tendon close to its attachment from the inferior pole of the patella. The lateral and one central fiber tape are then tied with half hitches with knee in 60° of flexion, traction is given to the other two free tapes during this to maintain the approximity of the tendon with the inferior pole of patella.
The remaining central tendon and the medial tape are then tied with half hitches.
2. A 3.5 mm anchor is then put in the central patella and the sutures are taken from the soft tissue on the patella and through the tendon to approximate the ends tightly.
Augmentation
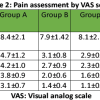
For additional strength and biological augmentation to the repair, an autologous free semitendinosus graft and a fiber tape were used (Fig. 3). The semitendinosus graft is whipped stitched on both ends. A 3.5 mm Siwel lock is used to fix the semitendinosus on the medial tibial side just close to the tibial tuberosity (Fig. 3a). The free edge of the semitendinosus is then passed through the quadriceps tendon from medial to lateral in a criss-cross fashion to increase the pull out strength. The free edge of the semitendinosus which is lateral now is fixed with a Siwel lock laterally close to the tibial tuberosity. Some tag sutures are taken between the repaired tendon and the graft both medially and laterally. She also had an associated medial collateral ligament tear avulsion on the tibial side which was repaired primarily using suture anchor. Immediate post-operative radiographs were done which were acceptable (Fig. 4, 4a). After the repair, knee was immobilized for 4 weeks in a long knee brace. Post-immobilization continuous passive movement machine was used to begin knee ROM with increments of 10–15°/week. At the end of the 8th week, the patient achieved a ROM of 90° (Fig. 5) with Grade 4/5 (MRC) power in quadriceps and extensor mechanism with no extensor lag (Fig. 5a). Radiographs repeated at 6th and 10th week show restored patellar position (Fig. 6, 7). At present, at 3 months follow-up, the patient walks without any walking aid and has no activity limitation or any participation restrictions.
Discussion
Disruption of the extensor mechanism of the knee following a TKA is an infrequent complication causing significant functional limitations. Due to inconsistent outcomes of the various surgical techniques available ranging from primary repairs with or without augmentations to reconstructions using autografts or allografts, the management of patellar tendon repair poses a great challenge to the operating surgeons. The goal of repair is to restore the functioning extensor mechanism, allowing good ROM. This can be achieved by judiciously selecting a surgical technique that allows stability as well as early mobilization. Our patient presented with a direct trauma to the patellar tendon after a fall, the first treatment of choice was primary repair. Primary repair is the best option in acute cases if the tendon tissue is long and durable enough for repair. Direct repair of patellar tendon rupture after TKA as reported by Rand et al. [5] had variable results in 18 knees: 25% of the patients had successful outcome. A semitendinosus graft was used for augmentation of the repair to add to its strength and allow early mobilization. Biological augmentation of primary repair reduces gap formation, decreases the strain across the repair site, and reduces the risk of rerupture [6]. A study by Larson and Simonia [7] showed that semitendinosus augmentation allows implementation of an aggressive rehabilitation protocol including immediate post-operative mobilization with excellent functional results. In our case, the proximal portion of tear did not have any stump and was more of an avulsion from the inferior pole of patella. Hence, a multimodal approach to patellar tendon repair and augmentation was used. First, a primary repair was achieved by through transosseous longitudinal tunnels which is familiar to most surgeons and has shown satisfactory results when used in isolation. We also used a 3.5 anchor placed on the patella and sutured the tendon with it, giving rise to an additional fixation. A semitendinosus autograft was used to augment the repair by passing it through quadriceps in zigzag manner and fixed on both the sides of tibia by Swivel lock. This construct provided additional strength and biological augmentation to the repair and a check-rein mechanism resulting in significantly less gap formation and the ability to withstand higher load to failure when compared with transosseous tunnels or suture anchor fixation alone [8]. A primary repair technique using a combination of transosseous sutures, suture anchors, and biological augmentation fixed with Siwel lock on both sides of the tibia has not been explored enough to our knowledge. A recent study by Jarret et al. [9] in 2017 used a similar augmentation technique using a hamstring autograft for an acute patellar tendon rupture after TKA managed by primary repair. The modification of the technique enabled early mobilization and weight-bearing which was crucial to our patient as it reduced the chances of adhesion formation, improved knee mobility, and promoted tendon healing. This reduced the disadvantages of prolonged immobilization including development of joint stiffness, muscle atrophy, and poor cartilage nutrition considering her age.
Conclusion
Patellar tendon rupture after a TKA poses a challenge due to wide variety of surgical procedures available but lack of clinical evidence to verify an optimal treatment method. Early detection of the condition, exact cause of rupture, and appropriate management strategies to use proper augmentation methods, fixation techniques, and rehabilitation protocols are crucial for overcoming the unexpected complication and obtaining good functional outcome. This report describes a meticulous surgical technique that strengthens the primary repair as well as allows early mobilization. We suggest that the surgeons should pay attention to weigh potential advantages and risk while choosing a particular technique to reduce the chances of rerupture and disadvantages of prolonged immobilization.
Clinical Message
Managing a patellar tendon rupture after a TKA can be challenging. Timely diagnosis, selection of surgical technique, and appropriate rehabilitation are essential for good functional outcomes.
References
1. Barrack RL, Stanley T, Butler RA. Treating extensor mechanism disruption after total knee arthroplasty. Clin Orthop Relat Res 2003;416:98-104.
2. Fan CH, Lo CK, Yung SH, Chan KM. A rare mode of extensor mechanism failure in total knee arthroplasty. J Arthroplasty 2011;26:338.e9-11.
3. Vaishya R, Agarwal AK, Vijay V. Extensor mechanism disruption after total knee arthroplasty: A case series and review of literature. Cureus 2016;8:e479.
4. Vajapey SP, Blackwell RE, Maki AJ, Miller TL. Treatment of extensor tendon disruption after total knee arthroplasty: A systematic review. J Arthroplasty 2019;34:1279-86.
5. Rand JA, Morrey BF, Bryan RS. Patellar tendon rupture after total knee arthroplasty. Clin Orthop Relat Res 1989;244:233-8.
6. Black JC, Ricci WM, Gardner MJ. Novel augmentation technique for patellar tendon repair improves strength and decreases gap formation: A cadaveric study. Clin Orthop Relat Res 2016;474:2611-8.
7. Larson RV, Simonian PT. Semitendinosus augmentation of acute patellar tendon repair with immediate mobilization. Am J Sports Med 1995;23:82-6.
8. Ode GE, Piasecki DP, Habet NA, Peindl RD. Cortical button fixation: A better patellar tendon repair? Am J Sports Med 2016;44:2622-8.
9. Woodmass JM, Johnson JD, Wu IT, Krych AJ, Stuart MJ. Patellar tendon repair with ipsilateral semitendinosus autograft augmentation. Arthrosc Tech 2017;6:e2177-81.
 |
 |
 |
 |
| Dr. Amyn M. Rajani | Dr. Meenakshi S. Punamiya | Ms. Kareena Rajani | Ms. Khushi Rajani |
| How to Cite This Article: Rajani AM, Punamiya MS, Rajani Kareena, Rajani Khushi. Modified Technique for Patellar Tendon Repair Post-Total Knee Arthroplasty: A Case Report. Journal of Orthopaedic Case Reports 2020 December;10(9): 15-18. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com