[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
The article highlights key radiological features to diagnose spinal SDH and the importance of imaging the brain in such cases.
Case Report | Volume 11 | Issue 4 | JOCR April 2021 | Page 75-79 | Swapnil Sanjay Hajare, B T Pushpa, Rishi Mugesh Kanna, Ajoy Prasad Shetty, Rajesh Babu, S Rajasekaran. DOI: 10.13107/jocr.2021.v11.i04.2160
Authors: Swapnil Sanjay Hajare[1], B T Pushpa[2], Rishi Mugesh Kanna[1], Ajoy Prasad Shetty[1], Rajesh Babu[1], S Rajasekaran[1]
[1]Department of Orthopaedics and Spine Surgery, Ganga Medical Centre and Hospitals Private Limited, Coimbatore, Tamil Nadu, India,
[2]Department of Radiodiagnosis, Ganga Medical Centre and Hospitals Private Limited, Coimbatore, Tamil Nadu, India.
Address of Correspondence:
Dr. Rishi Mugesh Kanna,
Department of Orthopaedics and Spine Surgery, Ganga Medical Centre and Hospitals Private Limited, Mettupalayam Road, Coimbatore, Tamil Nadu, India.
E-mail: rishiortho@gmail.com
Abstract
Introduction: Idiopathic spontaneous spinal subdural hematoma (ISSSDH) is uncommon in occurrence, and its association with concomitant intracranial subdural hematoma (ISDH) is very exceptional. Lack of recognition of ISDH in a patient with SSDH can lead to unanticipated events. We report a rare case of ISSSDH and unrecognized ISDH and treated surgically with a good outcome.
Case Report: A 71-year-old gentleman presented with features of spinal neurogenic claudication of 2 weeks duration and was diagnosed to have ISSSDH of the lumbar spine based on magnetic resonance imaging (MRI). In view of an impending cauda equina syndrome, he underwent an emergency decompression through a laminectomy, durotomy, and clot evacuation from L2 to L5. The next day, he developed sudden-onset hemiparesis and altered sensorium. The computed tomography (CT) scan of the brain demonstrated an ISDH, for which emergency burr hole evacuation was done. The patient improved rapidly after the surgery and regained his normal power, sensorium, and achieved comfortable ambulation within a week. Follow-up CT of the brain and MRI scan of the spine revealed adequate decompression. Since the CT features of ISDH were of acute on chronic nature, we presume that it had existed before the onset of spinal symptoms.
Conclusion: Through this very rare case, we highlight the importance of screening the brain pre-operatively in patients who present with sub-acute spontaneous spinal SDH.
Keywords: Sub-dural, hematoma, spinal, intracranial, spontaneous.
Introduction
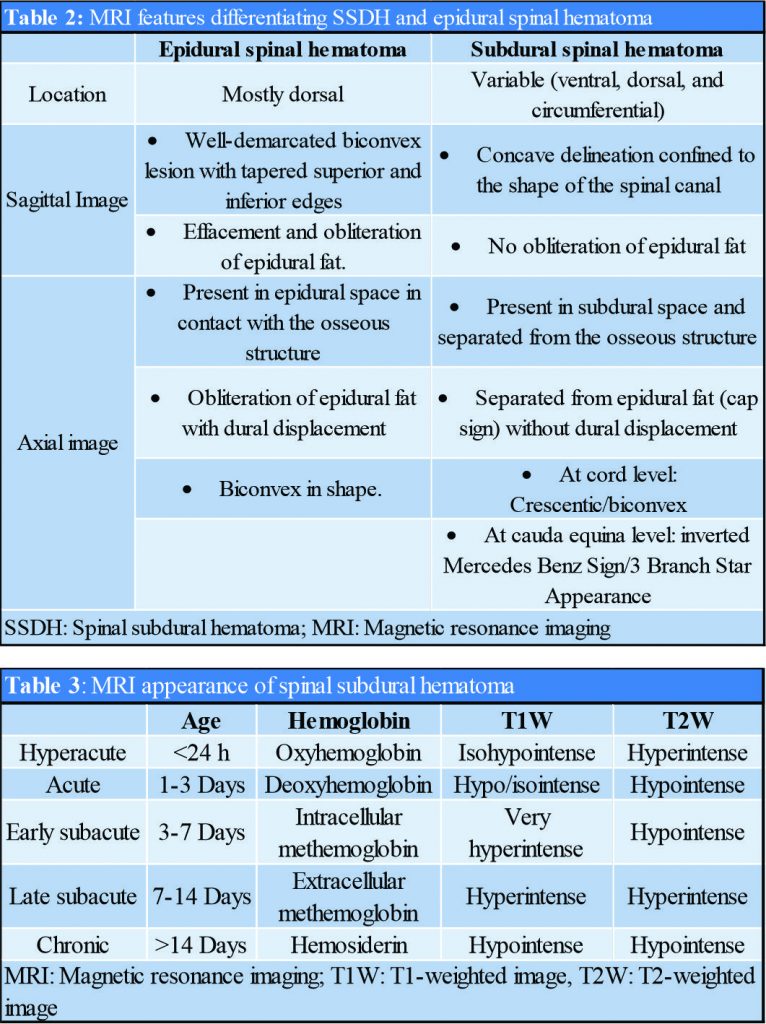
Spinal subdural hematoma (SSDH) is very rare in occurrence and represents 4.1% of total spinal hematoma when compared with epidural (75%), and subarachnoid spinal hematoma (15.7%) [1] Idiopathic Spontaneous SSDH (ISSSDH) is an infrequent phenomenon considering the absence of identifiable risk factors (trauma, spinal injection, anticoagulant, and coagulopathy) in these patients [2]. The coexistent ISSSDH with intracranial SDH (ISDH) is very exceptional, and only seven cases (Table 1) have been described [3, 4, 5, 6, 7, 8, 9]. We report the clinical and radiological features of a rare case of ISSSDH who developed ISDH a day after spine surgery and present a detailed review of the literature.
Case Report
A 71-year-old gentleman presented to us with complaints of bilateral lower limb radicular pain, more on the right side, with associated non-dermatomal patchy numbness in both lower limbs and minimal back pain. Symptoms were spontaneous in onset without a history of antecedent trauma, coagulopathy, or anticoagulant medication. It progressed over the 3 weeks, leading to incapacitating (visual analog scale [VAS] Score 9) pain in the lower limbs and difficulty in walking over the last 24 hours. He did not have other symptoms such as headache, nausea, vomiting, and related to intracranial hypertension. On clinical examination, the patient was fully conscious and oriented (Glasgow coma scale [GCS] 15/15). Gait was nonassessable due to severe radiculopathy, and straight leg raising test was restricted bilaterally. There was no local tenderness over the spine or paraspinal muscle spasm. He had mild weakness in the foot plantar and dorsi-flexors (3/5 grade) with bilaterally diminished ankle jerk, without any sensory deficit and bladder-bowel involvement.
Radiological features
The patient was further evaluated with magnetic resonance imaging (MRI) lumbosacral spine with whole spine sagittal screening (Fig. 1), which was suggestive of subacute subdural hematoma from T12 to S2 level [10] (Fig. 1).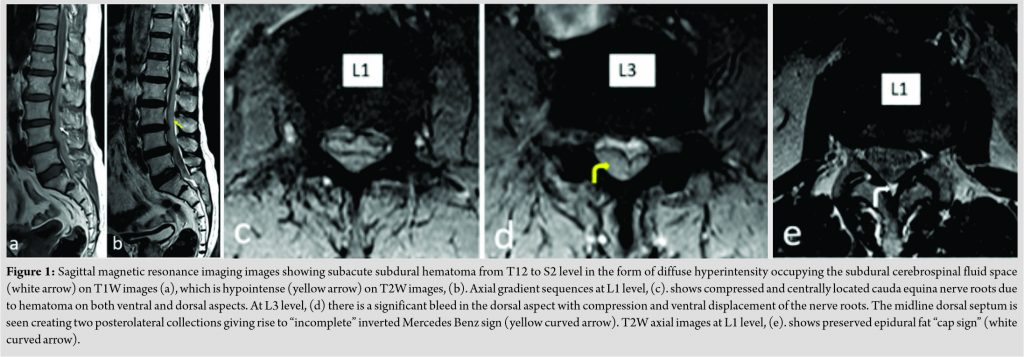
Surgical treatment
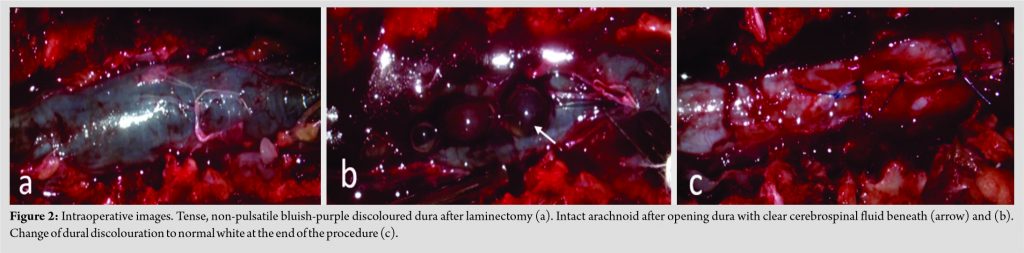
In view of the incapacitating pain and weakness in the distal muscles, the patient underwent emergency L1-L5 decompression and hematoma evacuation (Fig. 2). After hematoma evacuation, the dura was closed with 5-0 Prolene. There was no cerebrospinal fluid (CSF) leak, and the dural discolouration reversed to white at the end of the procedure (Fig. 2c). Post-operatively, the patient had stable vital and normal higher mental function without a sensory-motor deficit.
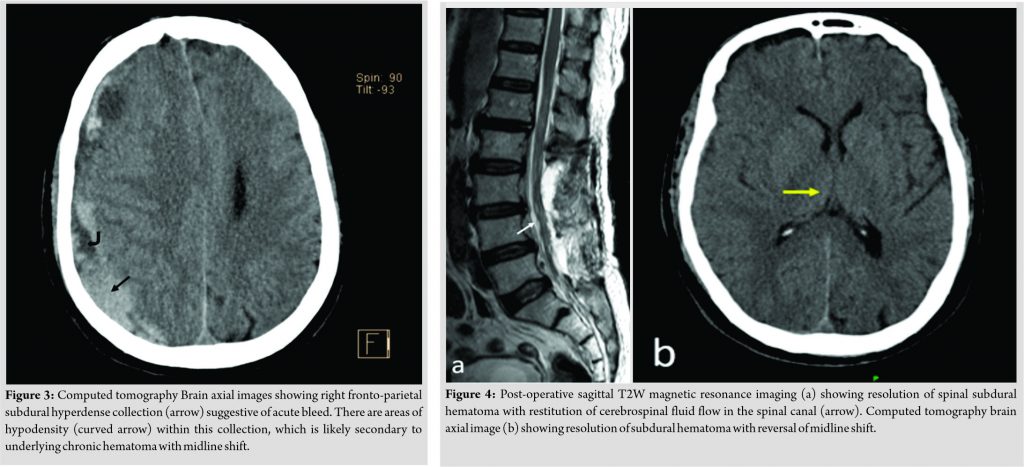
On the next day of surgery (18 hours later), the patient rapidly became drowsy and developed incoherent speech, nausea, and vomiting. On examination, he was partially conscious and disoriented (GCS 8/15). He had dilated right pupil with normal reaction to light in both the pupils and left hemiparesis. All the symptoms developed and worsened rapidly over 2 h. An emergency computed tomography (CT) brain (Fig. 3) showed acute on chronic right fronto-parietal ISDH with a midline shift of 8–9 mm to the left side. The patient underwent emergency right frontal and parietal burr hole decompression and subdural hematoma evacuation. The patient was ventilated electively for a day and on weaning showed improved mentation (GCS 15/15).
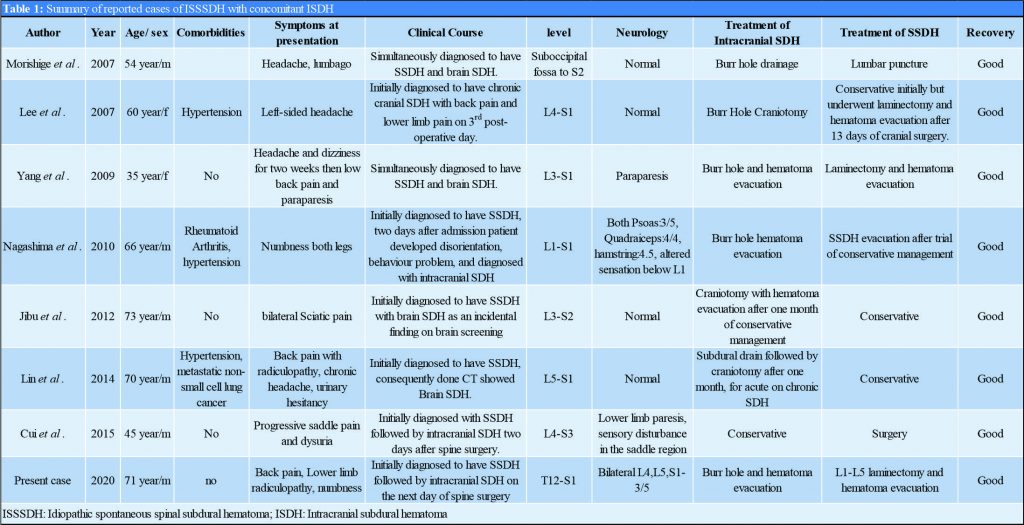
His neurology improved (4/5 Grade) gradually over the next 2 days, and he started to walk with support from the 6th post-operative day. Follow-up MRI (Fig. 4a), and CT scan (Fig. 4b) showed significant resolution of ISDH and SSDH, with reversal of midline shift, and a restituted CSF flow in the spinal canal. The patient was discharged on the 10th day after surgery and had complete resolution of symptoms and normal ambulatory capacity.
Discussion
Spinal hematoma, irrespective of its location, can be a catastrophe if not diagnosed and treated expediently. SSDH refers to a collection of blood between the layers of dura and arachnoid. It is commonly described after a traumatic event like spine injury, or spinal anesthesia (traumatic SSDH) or can develop after non-traumatic situations such as coagulopathy, anticoagulant medications, intra-spinal tumours, and arteriovenous (AV) malformations (spontaneous SSDH) [1, 10]. In the absence of these initiating factors, it is described as idiopathic SSSDH [2]. Although there are several case reports on SSSDH, the combination of idiopathic SSSDH with intra-cranial SDH is very rare (Table 1).
SSDH usually presents between the 4th and 6th decade without sex predilection [1]. Spontaneous SSDH has been shown to involve multiple segments and areas of the spine from almost the entire spine to a single segment. However, it most commonly involves the thoracolumbar region, followed by the cervical spine [12]. However, in patients with concomitant SSDH and ISDH, it has been mostly observed in the lumbosacral region, as in our case [13]. Clinically, SSDH can present with myriad symptoms and signs. It commonly presents with back pain, unilateral or bilateral radiculopathy, with varying degrees of a sensory-motor deficit. The neurological deficit may vary from completely normal neurology to complete paraplegia [1, 12, 14]. In patients of ISSSDH with ISDH, symptoms at presentation can vary greatly. Patients reported by Cui et al. [3], Jibu et al. [4], and Nagashima et al. [8] had initial symptoms related to the spine only, followed by the subsequent appearance of symptoms of ISDH. However, in the case reported by Lee et al. [5], the patient had no symptoms related to the spine at presentation but developed low back pain with lower limb radiculopathy on the third post-operative day of cranial surgery. Neurological deficit was reported in cases of Cui et al. [3], Nagashima et al. [8], and Yang et al. [9] Our patient had symptoms associated with the spine only at presentation and developed headache, nausea, incoherent speech, and hemiparesis on the next day of spine surgery.
The radiological diagnosis of SSDH is the most crucial step in the management of this pathology. MRI is the modality of choice for diagnosis, not only to differentiate subdural from an epidural hematoma but also best depicts the extent, location of hematoma in relation to cord or cauda equina, and can reveal underlying pathology. SSDH and epidural spinal hematoma can be differentiated based on MRI findings listed in Table 2 [1, 10, 11, 15, 16]. MRI is also important to diagnose the age of hematoma because the signal intensity of hematoma on MRI changes with time. It depends on the state of haemoglobin within hematoma and integrity of red blood cells [10, 15] (Table 3). The patho-mechanism of concomitant spinal and intracranial SDH is yet to be clearly defined. Few theories have been postulated, which include bleeding caused by increased shearing force between spinal subdural and subarachnoid spaces caused by raised intracranial pressure [17] or redistribution and migration of ISDH to the dependent lumbosacral spine [18]. Cui et al. [3] and Morishinge et al. [7] queried the redistribution hypothesis as chronic ISDH has an outer and inner membrane, and the mechanism of movement of hematoma out of these membranes is questionable. Cui et al. [19] noted that rebleeding or increased intracranial pressure might rupture the membrane, leading to redistribution of hematoma to the spine. In our case, considering the presence of acute on chronic ISDH and small non-compressing midthoracic SSDH, a possible mechanism could be the redistribution of ISDH. The acute exacerbation of the chronic ISDH can be explained by a sudden change in intracranial pressure caused by the loss of a substantial amount of CSF during spine surgery [19]. Since the possibility of ISDH tracking to the spinal sub-dural region exists in patients with idiopathic SSDH, we suggest a CT scan of the brain in all patients with SSDH to diagnose or rule out ISDH. This would help the surgeons to counsel the patients and plan the treatment accordingly. In idiopathic SSDH, even though treatment is limited to the hematoma management, as there is no underlying etiology to address, still controversy exists over preferred treatment. Those with coexistent ISDH have been managed differently in different studies, and it varies from simultaneous surgical evacuation to conservative management of SSDH/ISDH (Table 1). Lee et al. [5] considered conservative management initially but surgery on 13th post-operative day due to increased back pain, numbness, and radiculopathy in the lower limb, whereas Lin et al. [6] considered subdural drain for ISDH and conservative management for SSDH, but the patient developed gait instability after one month and underwent craniotomy for acute on chronic SDH. Our case considering severe, intractable radicular pain with bilateral foot muscle weakness, leading difficulty to walk; we decided to perform decompression with hematoma evacuation. The patient’s immediate post-operative period was uneventful until he developed incoherent speech and hemiparesis due to acute on chronic ISDH. As the patient developed an acute neurological deficit, he underwent emergency burr hole with hematoma evacuation.
Conclusion
The presentation of a rare case of SSSDH in the background of a possible pre-existing ISDH is clearly explained in this case report. Based on this report, we highlight the importance of the surgeon being aware of this possibility. Whenever a patient is diagnosed to have SSSDH without any predisposing factor or antecedent event, the patient should be considered for a pre-operative CT scan.
Clinical Message
Even though rare in occurrence, possibility of concurrent ISDH with SSSDH should be considered in the patient with ISSSDH and evaluated with a pre-operative CT scan.
References
1. Braun P, Kazmi K, Nogués-Meléndez P, Mas-Estellés F, Aparici-Robles F. MRI findings in spinal subdural and epidural hematomas. Eur J Radiol 2007;64:119-25.
2. Cui Z, Zhong Z, Wang B, Sun Q, Zhong C, Bian L. Coexistence of spontaneous spinal and undiagnosed cranial subdual hematomas. J Craniofac Surg 2015;26:e118-9.
3. Lee TH, Su TM, Wang KW, Lee HL, Ho JT. Lumbosacral spinal subdural hematoma following burr hole craniotomy: Case report and literature review. Clin Neurol Neurosurg 2007;109:282-6.
4. Jibu KJ, Pranesh MB, Prakash B, Saifudheen K. Bilateral intracranial and spinal subdural hematoma presenting as bilateral sciatica. J Neurosci Rural Pract 2012;3:97-8.
5. de Beer MH, Smeets MM, Koppen H. Spontaneous spinal subdural hematoma. Neurologist 2017;22:34-9.
6. Golden N, Asih MW. Traumatic subacute spinal subdural hematoma concomitant with symptomatic cranial subdural hematoma: Possible mechanism. World Neurosurg 2019;123:343-7.
7. Joubert C, Cungi PJ, Esnault P, Sellier A, de Lesquen H, Avaro JP, et al. Surgical management of spine injuries in severe polytrauma patients: A retrospective study. Br J Neurosurg 2019;34:370-80.
8. Post MJ, Becerra JL, Madsen PW, Puckett W, Quencer RM, Bunge RP, et al. Acute spinal subdural hematoma: MR and CT findings with pathologic correlates. AJNR Am J Neuroradiol 1994;15:1895-905.
9. Sciubba DM, Kretzer RM, Wang PP. Acute intracranial subdural hematoma following a lumbar CSF leak caused by spine surgery. Spine 2005;30:E730-2.
10. Morishige M, Abe T, Ishii K, Fujiki M, Kobayashi H, Karashima A, et al. Spontaneous chronic head and spinal subdural haematoma. Acta Neurochirurg 2007;149:1081-2.
11. Krishnan P, Banerjee TK. Classical imaging findings in spinal subdural hematoma-“Mercedes-Benz” and “cap” signs. Br J Neurosurg 2016;30:99-100.
12. Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: A literature survey with meta-analysis of 613 patients. Neurosurg Rev 2003;26:1-49.
13. Yang MS, Tung YW, Yang TH, Chai JW, Chen CC, Chan SW, et al. Spontaneous spinal and intracranial subdural hematoma. J Formos Med Assoc 2009;108:258-61.
14. Lin JC, Layman K. Spontaneous spinal subdural hematoma of intracranial origin presenting as back pain. J Emerg Med 2014;47:552-6.
15. Pierce JL, Donahue JH, Nacey NC, Quirk CR, Perry MT, Faulconer N, et al. Spinal hematomas: What a radiologist needs to know. Radiographics 2018;38:1516-35.
16. Hung KS, Lui CC, Wang CH, Wang CJ, Howng SL. Traumatic spinal subdural hematoma with spontaneous resolution. Spine 2002;27:E534-8.
17. Nagashima H, Tanida A, Hayashi I, Tanishima S, Nanjo Y, Dokai T, et al. Spinal subdural haematoma concurrent with cranial subdural haematoma: Report of two cases and review of literature. Br J Neurosurg 2010;24:537-41.
18. Joubert C, Gazzola S, Sellier A, Dagain A. Acute idiopathic spinal subdural hematoma: What to do in an emergency? Neurochirurgie 2019;65:93-7.
19. Bortolotti C, Wang H, Fraser K, Lanzino G. Subacute spinal subdural hematoma after spontaneous resolution of cranial subdural hematoma: Causal relationship or coincidence? Case report. J Neurosurg 2004;100:372-4.
 |
 |
 |
 |
 |
 |
| Dr. Swapnil Sanjay Hajare | Dr. B T Pushpa | Dr. Rishi Mugesh Kanna | Dr. Ajoy Prasad Shetty |
Dr. Rajesh Babu | Dr. S Rajasekaran |
| How to Cite This Article: Hajare SS, Pushpa BT, Kanna RM, Shetty AP, Babu R, Rajasekaran S. Missed Intracranial Subdural Hematoma in a Case of Spontaneous Subdural Spinal Hematoma: A Rare Case Report and Literature Review. Journal of Orthopaedic Case Reports 2021 April;11(4): 75-79. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com