[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Avoid skirted femoral heads in Dual mobility hip system.
Case Report | Volume 11 | Issue 3 | JOCR March 2021 | Page 6-9 | Gur Aziz Singh Sidhu, Amit Kotecha, Sanjay Mulay, Neil Ashwood . DOI: 10.13107/jocr.2021.v11.i03.2062
Authors: Gur Aziz Singh Sidhu[1], Amit Kotecha[1], Sanjay Mulay[1], Neil Ashwood[1]
[1]Department of Trauma and Orthopaedics, Queens Hospital Burton, University Hospitals of Derby and Burton, United Kingdom.
Address of Correspondence:
Dr. Gur Aziz Singh Sidhu,
Department of Trauma and Orthopaedics, Queens Hospital Burton, University Hospitals of Derby and Burton, United Kingdom.
E-mail: gur.sidhu@nhs.net
Abstract
Introduction: There is a trend for increasing use of dual mobility hip designs for both primary and revision hip arthroplasty settings. It provides dual articular surfaces along with increased jump distance to increase the stability of construct. However, this design has some unique complications of its own which surgeons should be aware of especially intraprosthetic dislocation (IPD).
Case Report: A 76-year-old lady presented to clinic with painful hip hemiarthroplasty after fracture neck of femur. She underwent revision surgery with dual mobility uncemented acetabular cup and femoral stem was retained as it was well fixed. She was mobilizing well and around 5 weeks post her surgery, developed pain in hip region and difficulty in weight-bearing. Radiographs showed eccentric position of femoral neck in the socket. A diagnosis of IPD was established and revision surgery was planned. Intraoperatively, metal head had dislocated from the polyethylene head and both components were resting in the acetabular socket. No macroscopic erosion of acetabulum was noticed. The polyethylene component and femoral head were retrieved. With previous failed dual mobility, decision was made to achieve stability with larger head size and lipped liner posteriorly.
Conclusion: IPD is a rare occurrence and unique complication to dual mobility implants. This report highlights that patients can have IPD without fall or trauma.
Keywords: Intraprosthetic dislocation, dual mobility cup, dislocation, total hip replacement.
Introduction
In 1974, Bousquet introduced the concept of dual mobility hip articulation in an attempt to reduce hip dislocations and improve joint stability post-hip replacement surgery [1, 2]. Over the recent years, there has been an increase in use of dual mobility cups in total hip replacement (THR) due to design, lower dislocation rates, and surgeon’s enthusiasm [3]. A dual mobility bearing consists a large polyethylene head (bearing) which articulates with a metal inside surface of a one-piece acetabular component and a smaller femoral head that articulates with the inside of the larger polyethylene head, thus comprising of two articulating surfaces. This constructs increases jump distance and range of motion, thus theoretically decreases the risk of dislocation [4]. Intraprosthetic dislocation (IPD) is a well-known complication which is specific to dual mobility designs [1, 2, 3, 4, 5]. Practically, it is dissociation of the femoral head from the outer polyethylene head in a dual mobility acetabular component. In majority cases, the smaller femoral head remains in the metal acetabular component; therefore, the term IPD is commonly used [2, 3, 5]. Although published studies showed an association of IPD with femoral head size [5, 6, 7, 8]. Larger the femoral head diameter is associated with reduced dislocation rates due to increase in jump distance. There are no reported cases of IPD in head size smaller than 28 mm. The literature has not shown any dislocations in skirted head groups too. Although most common cause of IPD is iatrogenic, that is, closed reduction of dislocated dual mobility total hip arthroplasty (THA) in emergency, spontaneous IPD of dual mobility implant has not been mentioned [6]. A classification system for IPD has been devised by Philippot et al. [2]. Although the exact cause of such dislocation is not known, cup loosening, arthrofibrolysis, failure of head capture mechanism, blocked liner, and impingement of femoral neck against the constrained polyethylene insert are among the commonly postulated mechanisms in the literature [2, 9]. The diagnosis is mainly based on anteroposterior and modified Lowenstein lateral radiographs of the hip. Eccentricity of the femoral head against the concave inner surface of the acetabular shell is the key to diagnose such dislocations. However, few studies have reported the use of computed tomography (CT) scan to diagnose and locate dislocated polyethylene liner [6]. The treatment of such IPD is complex requires revision arthroplasty promptly, as delay leads to acetabular damage necessitating acetabular shell revision [6, 7]. Some authors reported intrapelvic position of polyethylene liner and left it as retrieval was thought to be more morbid than retention [6].
Case Report
A 76-year-old lady presented to clinic with painful hip hemiarthroplasty after fracture neck of femur. CT scans suggested acetabular erosion. She was American Society of Anesthesiologists 3 patient with concerns of balance issues and high BMI of 42. She underwent complex primary THR using standard posterior approach to the hip. The stem was well-fixed cemented JRI stem, to reduce the morbidity, stem was retained a dual mobility uncemented acetabular ACE cup was used with size 40 polyhead. Inside metal head used was 22 mm (+3) plus head to achieve optimum leg length and offset. Good range of movement and stability were achieved. The patient had an eventful recovery with satisfactory post-operative radiographs.
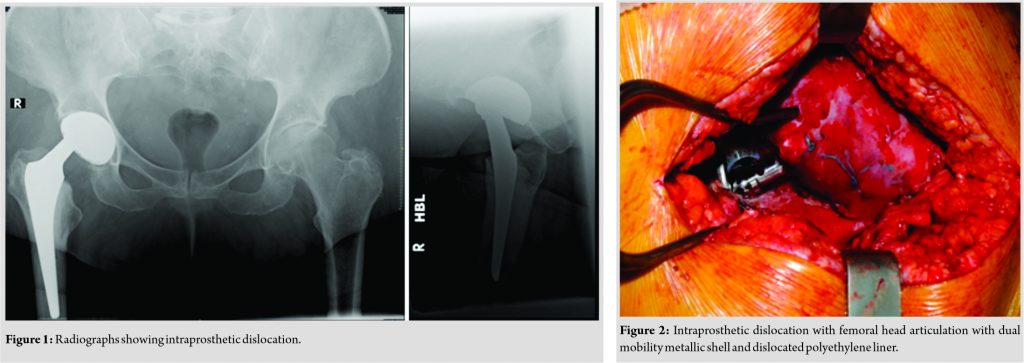
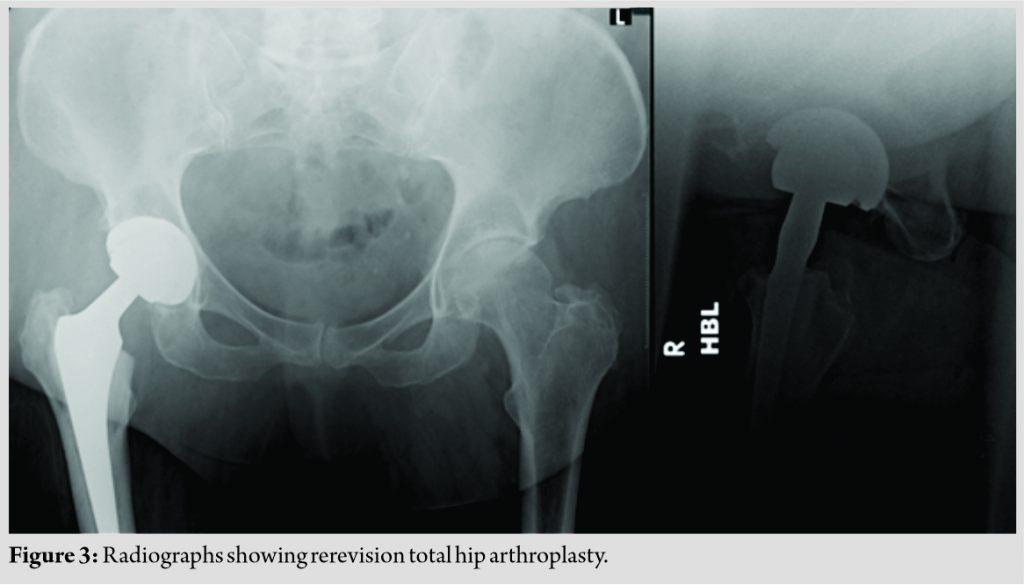
The patient had immediate relief of groin pain. The wound pain settled in 2 weeks. At 5 weeks, she was mobilizing with one stick and no pain. She woke up one morning with spontaneous onset pain in the groin region and difficulty in weight-bearing. She presented to the emergency department. Radiographs showed eccentric position of femoral neck in the socket (Fig. 1). A diagnosis of IPD was established and revision surgery was planned. She underwent exploration of her hip. The metal head had dislocated from the polyethylene head and both components were resting in the acetabular socket (Fig. 2). No macroscopic erosion of acetabulum was noticed. The components used were a 52 mm shell (ACE; JRI acetabular system) and dual mobility cup 40 mm outer and 22 mm inner small femoral component. The polyethylene component and femoral head were retrieved. The acetabular component and femoral stem were found stable and well-fixed intraoperatively, so a decision to revise only the liner and femoral head was taken. With previous failed dual mobility decision was made to achieve stability with larger head size and lipped liner posteriorly. The components placed at revision surgery were a hooded liner with 10° hood (ACE; JRI) and ceramic femoral head Biolox 36 mm (CeramTec, Germany). Post-operative radiographs confirmed that the femoral head was concentrically reduced in the acetabulum after the rerevision THA (Fig. 3). At 3 months follow-up, the patient is doing well clinically and radiographically.
Discussion
Recently, there is a shift to dual mobility implants in primary and revision THA owing to better stability due to increase in head-neck ratio and the jump distance. However, these components are prone to a unique and component specific complication – IPD which is well documented in literature. Theoretically, it is the uncoupling of inner femoral head from polyethylene head within the acetabular component and the reported incidence of such dislocations is 2–4% [2]. We report the first case of spontaneous IPD of dual mobility cup with a 22 mm skirted femoral head. The increased use of dual mobility implants may lead to a corresponding increase in the incidence of iatrogenic IPD. Most common cause of IPD is iatrogenic, that is, closed reduction of dislocated dual mobility THA in emergency [6]. This is the first report of spontaneous IPD without any trauma or warning signs or symptoms, which is quite unusual. The sequelae of missed iatrogenic IPD have been documented by Schirmers et al. [7]. They reported on a patient who was discharged from emergency because IPD was missed by surgeon and the patient had to undergo acetabular component revision due to severe damage to acetabular component [7]. Another worthy point about “Iatrogenic IPD” is association with the head size of the inner bearing. The usual diameter of the femoral head ranges from 28 mm to 36 mm. A larger head diameter increases the head-neck ratio at the inner articulation, thus increases the jump distance which may reduce component impingement and improves range of motion. After thorough search in the published literature, there were no cases of IPD occurring in patients with a femoral head smaller than 28 mm [5, 6, 7, 8]. However, we report first of IPD with a 22 mm femoral head in dual mobility prosthesis. It is hypothesized that skirted femoral heads may increase the risk of IPD because of decreased range of motion before impingement between the skirt and the PE liner [5, 10]. However, early IPD has not been reported in conjunction with a skirted femoral head in the published literature. This the first case report of skirted femoral head dislocation in dual mobility implant. Dual mobility implant is used to improve range of motion and decrease chances of dislocation. However, using skirted head instead of non-skirted can be counterproductive and may lead to spontaneous dislocation (Fig. 4). When treating a patient with a dislocated dual mobility bearing, it is important to recognize and keep in mind important facts of IPD.
1. The diagnosis of IPD may be missed routinely in emergency department. The key to diagnosis is eccentricity of the femoral head in the acetabulum. Although, CT scan can be used to localize the PE liner as migration of the free polyethylene intrapelvic/extrapelvic can occur. Surgeon’s decision regarding retrieval of polyethylene, if possible
2. Closed reduction attempt post-dislocation of dual mobility THA is most common cause of IPD. Closed reduction of such components is more difficult unless the PE liner fully clears the acetabular rim, otherwise PE rim impingement and iatrogenic IPD occur secondary to the “bottle-opener” effect
3. Mixing of dual mobility components with different manufacturer components is commonly an off-label practice and is not supported by the Food and Drug Administration and manufacturers. Literature supports mixing of components during primary or revision surgery is a cause of IPD. Hence, such clinical practice should be discouraged
4. Using a skirted head in dual mobility implants is not advisable as it increases the risk of dislocation due to impingement between the skirt and the PE liner.
Conclusion
IPD is a rare occurrence and unique complication to dual mobility implants. This significantly increases patient’s morbidity. This report highlights that patients can have IPD without fall or trauma. Clinical history, examination, and radiographs have to be performed and assessed carefully. Skirted heads should be avoided to reduce impingement.
Clinical Message
The diagnosis of IPD may be missed routinely in the emergency department. Mixing of dual mobility components with different manufacturer components is common and should be avoided. Finally, avoid use of skirted heads in dual mobility implants.
References
1. Philippot R, Adam P, Farizon F, Fessy MH, Bousquet G. Survival of cementless dual mobility sockets: Ten-year follow-up. Rev Chir Orthop Reparatrice Appar Mot 2006;92:326-31.
2. Philippot R, Boyer B, Farizon F. Intraprosthetic dislocation: A specific complication of the dual-mobility system. Clin Orthop Relat Res 2013;471:965-70.
3. Banzhof JA, Robbins CE, van der Ven A, Talmo CT, Bono JV. Femoral head dislodgement complicating use of a dual mobility prosthesis for recurrent instability. J Arthroplasty 2013;28:543.e1-3.
4. De Martino I, Triantafyllopoulos GK, Sculco PK, Sculco TP. Dual mobility cups in total hip arthroplasty. World J Orthop 2014;5:180-7.
5. Odland AN, Sierra RJ. Intraprosthetic dislocation of a contemporary dual-mobility design used during conversion THA. Orthopedics 2014;37:e1124-8.
6. Fehring KA, Berry DJ. Dissociation and intrapelvic entrapment of a dual-mobility polyethylene component. Clin Orthop Relat Res 2016;474:1072-6.
7. Schirmers J, Horazdovsky R, Marston S. Early intraprosthetic dislocation of dual-mobility total hip arthroplasty implant following attempted closed reduction: A case report. Reconstr Rev 2015;5:47.
8. Nich C, Vandenbussche E, Augereau B, Sadaka J. Do dual-mobility cups reduce the risk of dislocation in total hip arthroplasty for fractured neck of femur in patients aged older than 75 years? J Arthroplasty 2016;31:1256-60.
9. de Martino I, D’Apolito R, Waddell BS, McLawhorn AS, Sculco PK, Sculco TP. Early intraprosthetic dislocation in dual-mobility implants: A systematic review. Arthroplast Today 2017;3:197-202.
10. Swiontkowski M. Concern about early intraprosthetic dislocation in dual-mobility implants. JBJS Case Connect 2013;3 Suppl 9:e911-7.
 |
 |
 |
 |
| Dr. Gur Aziz Singh Sidhu | Dr. Amit Kotecha | Dr. Sanjay Mulay |
Dr. Neil Ashwood |
| How to Cite This Article: Sidhu GAS, Kotecha A, Mulay S, Ashwood N. Spontaneous early intraprosthetic dislocation of 22 mm skirted femoral head in dual mobility hip prosthesis: A case report. Journal of Orthopaedic Case Reports 2021 March;11(3):6-9. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com