 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
In borderline cases of salvage versus amputation, scoring system considers patients options. There is no unanimously accepted scoring system guiding management of the mangled extremity; therefore, a systematic and multidisciplinary approach that encompasses all factors must be employed.
Case Report | Volume 11 | Issue 2 | JOCR February 2021 | Page 119-127 | N Jambu, Sundar Suriyakumar, Sharandeep Singh Saluja, Muthumanickam Ramanujam, Muhammed Niyas Mancheri . DOI: 10.13107/jocr.2021.v11.i02.2052
Authors: Sundar Suriyakumar[1], Sharandeep Singh Saluja[1], Muthumanickam Ramanujam[1], Muhammed Niyas Mancheri[1], N Jambu[1]
[1]Department of Orthopaedic surgery, Sri Ramachandra Institute of Higher Education and Research Centre, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. N Jambu,
Department of Orthopaedic Surgery, Sri Ramachandra Institute of Higher Education and Research Centre, Porur, Chennai – 600 116, Tamil Nadu, India.
E-mail: doctorjambu@gmail.com
Abstract
Introduction: Severe open injuries of limbs, especially of the femur and tibia when associated with vascular injuries, present major challenges in management. The decision to amputate or salvage can often be a difficult one even for experienced surgeons. Mangled lower extremity results due to high-energy trauma, especially due to motor vehicle accidents, and is defined as injury to three of the four systems in the extremity that is soft tissues, bone, vascular, and nerve. Open fractures are classified by Gustilo and Anderson’s classification in which type 3B is an injury where soft-tissue loss and primary closure of the wound are not possible and type 3C is any open fracture with vascular compromise.
Case Report: We report a series of six ipsilateral fractures of the femur and the tibia treated at the Department of Orthopaedics, Sri Ramachandra Medical College and Hospital, Chennai, Tamil Nadu, over a 3-year period (2014–2017). The mean age of our patients was 30 years old, and there were five men and one woman. The right side lower limb was frequently involved (five cases), and the main etiology was road traffic accidents (six cases). Articular involvement was found in six cases. Skin wounds were noticed in all cases (type III C of the Gustilo classification). Urgent wound care, fluid replacement, and antibiotic therapy were undertaken for open fractures. According to modified Fraser classification, all six cases was classified under type II-C. Mangled extremity severity score for five cases was 7 and for one case it was 8. Ganga Hospital Open Injury Severity Score was also used which was found to be in borderline range of 16 score for three cases, 15 score for two cases, and 14 score for one case. All six cases were managed with serial wound debridement + Ilizarov fixator + soft-tissue repair with involvement of orthopedic, vascular, and plastic surgery team. Limb salvage was done for all six cases after considering all the factors. Postoperatively, rehabilitative care and physiotherapy in the form of non-weight-bearing mobilization with walker support was given to all patients. The patients were followed up for the period of 2 years and doing symptomatically better. Based on current literature guidelines and evidence-based medicine, management for borderline cases is proposed to aid clinical decision-making in these situations.
Conclusion: With great effort and good team work (like vascular and orthopedic surgeons), badly comminuted compound injuries (Type III C injury) can be managed well with Ilizarov fixation. Even though the decision of amputation versus salvage was based on more scientific/scoring system, patient’s option should be taken, especially in borderline cases considering the present medicolegal scenario.
Keywords: Amputation versus salvage, Gustilo and Anderson’s classification, mangled extremity severity score, open fractures.
Introduction
Mangled limb is defined as one that involves a combination of injuries affecting at least three out of the four components of the extremity: Vascular, nervous, soft tissues, and underlying bone. Basically, it is related to type IIIB and IIIC injuries within the Gustilo and Anderson’s classification. However, every work commonly uses criteria that do not always fit within this definition. It is a situation that can lead to amputation in 9% of the cases in the first 24 h and in 21% during the hospitalization [1]. The term “floating knee” was first described by Blake and McBride in 1975 [2]. It is an ipsilateral fracture of the femur and tibia that includes diaphyseal, metaphyseal, and intra-articular regions of the bone. Road traffic accidents are the most common cause of this type of complex injuries [3]. The incidence of road traffic accidents is on the rise and is often associated with complex life-threatening conditions and extensive soft-tissue damage. Management of these injuries varies according to the type and extent of bony and soft-tissue involvement.
The degree of severity of open fractures is often classified in accordance with the system of Gustilo and Anderson [5]. This takes into account the wound size, fracture pattern, and degree of soft-tissue contamination. Type III of this classification corresponds to fractures due to high-energy trauma, with extensive injury to soft tissues [4, 5]. The extensive damage seen in types IIIB and IIIC may be a veritable challenge, even for surgeons with greater experience. It may require a clinical decision between attempts to salvage the limb and amputation. Clinical advances within orthopedic, plastic, and vascular surgery have provided the means for reconstructing injuries to limbs that, around 20 years ago, would have resulted primarily in amputation. However, some studies have reported that limb salvage is not always the best solution and that early amputation with prosthetic treatment should be recommended in some cases [6, 7]. Helfet et al. [7] established the use of the mangled extremity severity score (MESS), which grades injuries based on the clinical findings and takes into consideration the characteristics of the injury, the duration of ischemia, the shock, and the patient’s age. Scores greater than or equal to 7 have predictive value for limb amputation [6]. In the past several decades, limbs with Gustilo type Grade IIIC injuries (open fractures of the lower limb associated with vascular injury) have been difficult to salvage and have been treated by primary amputation. With the advancement of surgical technique, especially the use of microsurgery, the salvage rate for Grade IIIC lower limb fractures is rising, and the rates of attempted limb salvage are also increasing [8]. Many patients have undergone successful limb salvage [9]. These fractures can be managed by reconstruction or amputation. The decision regarding which option to choose can be difficult for both physicians and patients. Complicating this decision is the young age of many of the patients. In the past, when there were few reliable options for lower limb reconstruction, amputation was the preferred choice because salvage attempts generally used skin grafting, which was inadequate to cover exposed bone [10]. This resulted in high rates of osteomyelitis and secondary amputation [10]. The advancement of microsurgical techniques allowed cooperative efforts between orthopedic and plastic surgeons to reconstruct severe open fractures and achieve predictable limb salvage [11]. Reconstruction is performed at a much higher rate than primary amputation, despite the lack of evidence indicating better outcomes associated with reconstruction [10]. It is understandable that both physicians and patients will want to salvage an injured limb. Suffering a serious injury, like an open tibial facture, will have grave physical, emotional, and financial consequences, regardless of the treatment method used. The choice of treatment ideally should be based on careful consideration of the available data.
Case Report
We report a series of six ipsilateral fractures of the femur and the tibia treated at the Department of Orthopaedics, Sri Ramachandra Medical College and Hospital, Chennai, Tamil Nadu, over a 3-year period (2014–2017). The mean age of our patients was 30 years old, and there were five men and one woman. The right side was frequently involved (five cases), and the main etiology was road traffic accidents (six cases). Articular involvement was found in six cases. Skin wounds were noticed in all cases (type III C of the Gustilo classification). Urgent wound care, fluid replacement, and antibiotic therapy were undertaken for open fractures. According to modified Fraser classification, all six cases was classified under type II C. MESS for 5 cases was 7 and for one case it was 8. Ganga Hospital Open Injury Severity Score (GHOISS) was also used which was found to be in borderline range of 16 score for three cases, 15 score for two cases, and 14 score for one case.
Case 1
A 27-year-old gentleman sustained an open Grade 3C Gustilo-Anderson fracture with the right floating knee that was initially treated with debridement and external fixator and advised amputation above knee in outside hospital and presented to us within 12 h of initial injury. On head to toe examination, no other musculoskeletal and organ injuries were present. On initial presentation, he was hypotensive (blood pressure – 90/70 mm of Hg) and was started on appropriate measures by emergency room team. All cases had no known medical comorbidities, non-smoker, non-alcoholic, and no drug addiction. 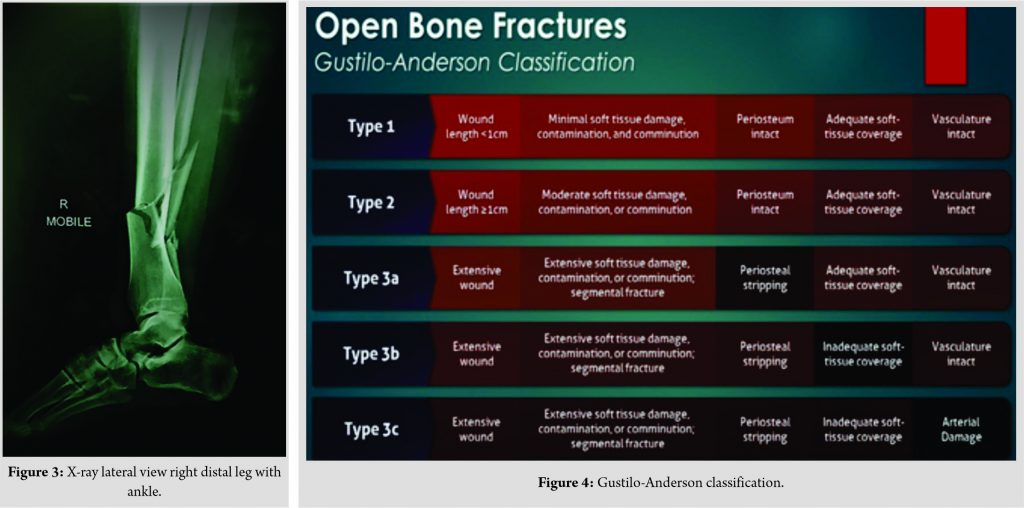
1. Right lower limb knee spanning external fixator present
2. Lacerated wound of size 20 cm ×10 cm extending from distal third of thigh to middle third of leg anteriorly. Wound contamination present (Fig. 1)
3. Both femoral condyle fractured fragments and proximal tibial fractured fragments exposed (Fig. 1)
4. Patella and lateral tibial condyle absent (Fig. 1)
5. Tendons and muscles were exposed (Fig. 1)
6. Dorsalis pedis artery pulsation – feeble
7. Posterior tibial artery pulsation – absent
8. Sensations over right lower limb were intact
9. Active dorsiflexion and plantar flexion present.
Examination of neurovascular functions-
Vascular–
Anterior tibial artery pulsation feeble.
Posterior tibial artery pulsation was not felt.
Local orthopedics severity were assessed using-
1. Gustilo-Anderson’s classification (Fig. 4)
2. Modified Fraser’s classification (Fig. 13).
Vascular surgeon opinion was sought and advised to do right lower limb computed tomography (CT) angiogram. CT study report shows posterior tibial vessel under spasm and anterior tibial sluggish blood flow. Vascular surgeon advised conservative treatment. According to modified Fraser classification, it was classified under type II C. The MESS (Table 1) was used to assist in the decision of injuries that also had a vascular component and the total score was found to be 7 (≥7 should be consider for amputation). In view of partial vascular injury (anterior tibial artery pulsation feeble and posterior tibial artery pulsation were not felt), GHOISS was also used which was found to be in borderline range of 16 score (Table 2). Scoring systems provided limited diagnostic benefit. 



All patients were followed up for the period of 2 years. Average range of motion for all patients was 0–40 degree with some instability and some extension lag.
Discussion
Floating knee injury (FKI) is uncommon injuries and its true incidence remains unknown. Patients with FKI are usually victims of high-speed trauma, mostly motor vehicle accident which involves fracture of femur and tibia. It is not just an extremity injury, several organ injuries and multiple fractures are often associated, which can be life threatening. The role of early total care (ETC) and orthopedic damage control (DCO) in polytrauma has always been a controversial issue. In stable patients, ETC is more appropriate and in unstable patients DCO is required. However, considerable doubt remains in borderline patients. The incidence of amputation was reported to 27% in FKI which had massive soft-tissue crushing, severe infection, and neurovascular injuries [12]. Blake and McBride [20] defined the FKI as the ipsilateral fractures of the femur and the tibia. Fraser et al. in 1978 classified floating knee in more detail [14]. This classification was again modified by Letts and Vincent [15] in 1986 which included soft-tissue injury associated with these injuries. Decision-making in clinical situation of mangled extremity in complex as number of factors is involved [18]. These factors are as follows:
a. Wound related:
(1) Fracture grade and type. (2) Compartment syndrome. (3) Possibility of immediate fixation. (4) Duration and severity of ischemia. (5) Loss of soft tissues of the foot.
b. Patient related:
(1) Associated systemic injuries. (2) Shock. (3) Coagulopathy. (4) Need for vasoconstriction. (5) Acute respiratory distress syndrome. (6) Age. (7) Comorbid conditions. (8) Hospital resources. (9) Transport time. (10) Mass/military casualty. (11) Patient cooperation.
c. Scoring systems:
d. Expected outcome:
Mandatory weight bearing • Protective sensations • Presence of durable skin and soft tissues.
e. Experience of surgeon availability of vascular and plastic surgeons.
All above factors have to be considered individually and collectively to decide on amputation versus salvage.
Patients who initially confront a threatening injury often focus on the loss of the extremity rather than on the consequences of the limb salvage. Patients undergoing this procedure, will require more complex operations, longer hospitalization, and will suffer more complications than primary amputees. Tornetta and Olson reported on patients who have undergone multiple operations over a period of several years to “heroically” save a leg only to render the patient depressed, divorced, unemployed, and significantly disabled [16]. Unfortunately, “salvage” of a mangled extremity is no guarantee of functionality or employability. It is crucial for the patient and his family to realize that both salvage and early amputation by no means can reassure the patient that will return to a previous normal, pain-free extremity [17]. In our study, all six patients are doing well after limb salvage surgery. Functional improvement has been seen during the follow-up periods (Fig. 12). Significant indicators of poor outcome results of floating knee injuries are intra-articular involvement of the fractures, severity of skeletal injury, and severity of soft-tissue injuries. In most of the patients, sepsis and other infection complications may be so severe and persistent that ultimately secondary amputation is required. Bondurant et al. [19] compared primary versus delayed amputations in 43 cases, including 14 primary and 29 delayed ones. Important findings included six deaths from sepsis in delayed amputation group compared with none in the early amputation group. In our study, no clinical and laboratory evidence of sepsis were noted. No secondary amputations were performed. Complication was seen in two cases which were resolved overtime. Although cost should not be a major deciding factor for limb salvage, many patients may be devastated by the cost not only of medical bills but also of time off work [19]. Fairhurst [20] retrospectively compared the functional outcome of patients who sustained traumatic below-knee amputations with that in patients who underwent limb salvage of Gustilo type III open tibial fractures. All patients in the early amputation group returned to work within 6 months of injury, while those who underwent late amputation and salvage returned to work an average of 36 and 18 months after injury, respectively. The authors recommend an early amputation when confronted with borderline salvageable tibial injury. In our study, all patients returned to their work after average duration of 12 months following injury. Fagelman et al. [21] evaluated the correlation between fractures of Gustilo and Anderson types IIIB and IIIC and the MESS index for exposed fractures of the lower limbs and found results that significantly predicted treatment, for 93%. On the other hand, Sheean et al. [22] did not find any significant difference in MESS values between amputees and patients whose limbs were salvaged. Both of these authors highlighted the importance of the presence of vascular lesions as a factor predictive of amputation. Slauterbeck et al. [23] reported that early use of a scoring system such as MESS would possibly reduce the morbidity associated with prolonged hospital stay and with the various surgical procedures performed in these cases. In our study, in spite of MESS score (Table 1) of 7 for five cases and 8 for one case which is suggestive of amputation, we have chosen the option of salvaging the limb after considering the patient factor. With MESS score of 7 or greater, amputation is the eventual result. No scoring system, however, can replace experience and good clinical judgment. It needs to be remembered that advances made in limb salvage surgery have been matched by advances in amputation surgery and prosthesis design. More often, however, the choice between limb salvage and amputation must be made on the basis of expectations and desires of individual patient and the family. Although scoring systems may be helpful, the patient’s status cannot simply be summarized by a score number. A closer look reveals that many questions remain unanswered. These systems fail to consider factors related to the patient’s quality of life, pain, occupation, age, wishes, social support system, family status, and financial resources. The training and experience of the surgical team may also influence the decision to amputate or reconstruct. Although these considerations are more subjective, undoubtedly they are very important. The true measure of successful limb salvage lies in the overall function and satisfaction of the patient. In our study, the main reason for limb salvage, despite the indication for amputation according to MESS and borderline Ganga scoring system (Table 2), it was patient and physician’s choice in relation to his occupation, condition, and psychology. The final decision regarding the treatment for patients with a diagnosis of an exposed fracture of the tibia needs to take into account future functionality, availability of recovery, the patient’s profile, and the surgeon’s expertise. The criteria for indicators such as the MESS score and the fracture classification need to be carefully analyzed so that the limb salvage can be done in an effective manner and so that amputation is done in precisely selected cases. There are many studies in literature suggesting internal fixation of both the fractures of floating knee should be done as early as possible [26]. Ratliff found that internal fixation of both fractures was less likely to cause the development of knee stiffness and lessen the duration of hospital stay [27]. Ostrum treated patients with retrograde femoral nailing and antegrade tibia nailing through 4 cm medial parapatellar incision [28]. The average time to union of femoral fracture was 14.7 weeks and for tibial fracture was 23 weeks. Theodoratos et al. [14] recommended intramedullary nailing as the best choice of treatment, except for grades IIIB and IIIC open fractures. In our study, all patients were treated with initially by application of external fixator followed by Ilizarov fixator application. Average time to union of femoral fracture was 8 months and for tibia fracture was 12 months. In literature, we found that outcome of FKI was often variable, some author reported 0 excellent result and other author reported excellent result up to 53%. These variable results might be due to associated neurovascular injury, open fracture, and variable fracture pattern with FKI [25]. Even though the predicted value for amputation of a MESS score higher than or equal to 7 appears to be very high, with larger numbers, there inevitably will be a limb with a score of higher than or equal to 7 that will be salvaged, or a limb with a score of lower than or equal to 6 that will require delayed amputation.
Conclusion
As a majority of cases represent a “gray zone” of unpredictable prognosis, and borderline cases are a dilemma, the decision to amputate or not amputate should not always be made during the initial evaluation. Although scoring systems and “cutoff points” are useful, the final decision for limb salvage should be based on team experience, technical skills, multidisciplinary consultation, tertiary care facility, and the profile of the patient. Scoring systems should be used only as guides to supplement the surgeon’s clinical judgment and experience. Excellent clinical and functional outcomes can be achieved with individualized planning of treatment which is dependent on the patient’s general condition, type of fracture, and severity of soft-tissue injury by an experienced multidisciplinary team instead of a fixed definite management for all patients. With great effort and good team work (like vascular and orthopedic surgeons), badly comminuted compound injuries (Type III C injury) can be managed well with Ilizarov fixation. Even though the decision of amputation versus salvage was based on more scientific/scoring system, patient’s option should be taken, especially in borderline cases considering the present medicolegal scenario.
Clinical Message
The treatment of mangled extremity treatment should be based on evidence-based literature along with a clinical evaluation of every individual patient. Scores are helpful, but should not be taken as the sole indication for amputation.
References
1. De Mestral C, Sharma S, Haas B, Gomez D, Nathens AB. A contemporary analysis of the management of the mangled lower extremity. J Trauma Acute Care Surg 2013;74:597-603.
2. Blake R, McBryde A Jr. The floating knee: Ipsilateral fractures of the tibia and femur. South Med J 1975;68:13-6.
3. Goel SA, Bhavsar NM, Makwana H, Lil NA, Patel PR. Epidemiology and patterns of lower limb injuries at a tertiary care hospital in Ahmedabad? Int J Med Res Rev 2015;3:490-6.
4. Kamath AF, Horneff JG, Esterhai JL, Lackey WG, Jeray KJ, Broderick JS. Open fractures. In: Bhandari M, editor. Evidence-Based Orthopedics. Oxford: Blackwell Publishing; 2012. p. 617-26.
5. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am 1976;58:453-8.
6. Busse JW, Jacobs CL, Swiontkowski MF, Bosse MJ, Bhandari M. Complex limb salvage or early amputation for severe lower-limb injury: A meta-analysis of observational studies. J Orthop Trauma 2007;21:70-6.
7. Helfet DL, Howey T, Sanders R, Johansen K. Limb salvage versus amputation. Preliminary results of the mangled extremity severity score. Clin Orthop Relat Res 1990;256:80-6.
8. Huh J, Stinner DJ, Burns TC, Hsu JR, Late Amputation Study Team. Infectious complications and soft tissue injury contribute to late amputation after severe lower extremity trauma. J Trauma 2011;71:S47-51.
9. Harris AM, Althausen PL, Kellam J, Bosse MJ, Castillo R, Lower Extremity Assessment Project (LEAP) Study Group. Complications following limb-threatening lower extremity trauma. J Orthop Trauma 2009;23:1-6.
10. Parrett BM, Matros E, Pribaz JJ, Orgill DP. Lower extremity trauma: Trends in the management of soft-tissue reconstruction of open tibia-fibula fractures. Plast Reconstr Surg 2006;117:1315-22.
11. Meyer M, Evans J. Joint orthopaedic and plastic surgery management of Types III and IV lower limb injuries. Br J Plast Surg 1990;43:692-4.
12. Dwyer AJ, Paul R, Mam MK, Kumar A, Gosselin RA. Floating knee injuries: Long-term results of four treatment methods. Int Orthop 2005;29:314-8.
13. Lichte P, Kobbe P, Dombroski D, Pape HC. Damage control orthopedics: Current evidence. Curr Opin Crit Care 2012;18:647-50.
14. Pal JD, Victorino GP, Twomey P, Liu TH, Bullard MK, Harken AH. Admission serum lactate levels do not predict mortality in the acutely injured patient. J Trauma 2006;60:583-7.
15. Pape H, Stalp M, Griensven M, Weinberg A, Dahlweit M, Tscherne H. Optimal timing for secondary surgery in polytrauma patients: An evaluation of 4,314 serious-injury cases. Chirurg 1999;70:1287-93.
16. Tornetta P 3rd, Olson SA. Amputation versus limb salvage. Instr Course Lect 1997;46:511-8.
17. MacKenzie EJ, Bosse MJ, Pollak AN, Webb LX, Swiontkowski MF, Kellam JF, et al. Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg Am 2005;87:1801-9.
18. Shawen SB, Keeling JJ, Brawstetter J, Kirk KL, Fickr JR. Foot Ankle Clin 2010;15:63.
19. Bondurant FJ, Cotler HB, Buckle R, Miller-Crotchett P, Browner BD. The medical and economic impact of severely injured lower extremities. J Trauma 1988;28:1270-3.
20. Fairhurst MJ. The function of below-knee amputee versus the patient with salvaged grade III tibial fracture. Clin Orthop Relat Res 1994;301:227-32.
21. Fagelman MF, Epps HR, Rang M. Mangled extremity severity score in children. J Pediatr Orthop 2002;22:182-4.
22. Sheean AJ, Krueger CA, Napierala MA, Stinner DJ, Hsu JR. Skeletal trauma and research consortium (STReC). Evaluation of the mangled extremity severity score in combat-related Type III open tibia fracture. J Orthop Trauma 2014;28:523-6.
23. Slauterbeck JR, Britton C, Moneim MS, Clevenger FW. Mangled extremity severity score: An accurate guide to treatment of the severely injured upper extremity. J Orthop Trauma 1994;8:282-5.
24. Gregory RT, Gould RJ, Peclet M, Wagner JS, Gilbert DA, Wheeler JR, et al. The mangled extremity syndrome (M.E.S.): A severity grading system for multisystem injury of the extremity. J Trauma 1985;25:1147-50.
25. Kao FC, Tu YK, Hsu KY, Su JY, Yen CY, Chou MC. Floating knee injuries: A high complication rate. Orthopedics 2010;33:14.
26. Bansal VP, Singhal V, Mam MK, Gill SS. The floating knee. 40 cases of ipsilateral fractures of the femur and the tibia. Int Orthop 1984;8:183-7.
27. Ratliff AH. Fractures of the shaft of the femur and tibia in the same limb. Proc R Soc Med 1968;61:906-8.
28. Ostrum RF. Treatment of floating knee injuries through a single percutaneous approach. Clin Orthop Relat Res 2000;375:43-50.
29. Hansen ST Jr. Overview of the severely traumatized lower limb. Reconstruction versus amputation. Clin Orthop Relat Res 1989;243:17-9.
 |
 |
 |
 |
 |
| Dr. Sundar Suriyakumar | Dr. Sharandeep Singh Saluja | Dr. Muthumanickam Ramanujam | Dr. Muhammed Niyas Mancheri | Dr. N Jambu |
| How to Cite This Article: Suriyakumar S, Saluja SS, Ramanujam M, Mancheri MN, Jambu N. Management of Grade 3C Compound Injury of Lower Limb with Floating Knee – Salvage versus Amputation (Case Series). Journal of Orthopaedic Case Reports 2021 February;11(2): 119-127. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com










