Well functioning total knee arthroplasty cases can develop popliteal cysts after surgery, which can rupture and percolate into the soft tissue planes, leading to clinical picture resembling deep vein thrombosis; these require prompt diagnosis and treatment for good prognosis.
Dr. Prasoon Kumar,
Department of Orthopaedics,
Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh – 160 012, India.
E-mail: drprasoonksingh@gmail.com
Introduction: Implant wear and loosening with eluding metal/polythene debris are commonly implicated in the occurrence of Baker’s cysts in post-operative total knee replacement (TKR) patients, who present with post-operative pain and swelling, mimicking deep venous thrombosis. However, we present two symptomatic cases presenting with ruptured Baker’s cysts post-TKRs, with no evidence of implant loosening or wear.
Cases Report: The 1st patient was a 55-year-old male, who underwent TKR for Grade 4 bilateral knee osteoarthritis and presented with acute onset of pain and swelling over the left popliteal fossa, which progressed to involve the calf. Radiographs showed no sign of infection or loosening, and venous color Doppler and magnetic resonance imaging (MRI) showed a hy-poechoic collection in the intermuscular plane at the upper part of popliteal fossa. Histological examination of the aspirated fluid showed mixed features of cystic fluid and a resolving hematoma. There was complete resolution of the 4 months with rest and graduated physiotherapy. The 2nd patient was a 51-year-old female who developed the cystic swelling 2 years after the surgery, and the ultrasound showed hypoechoic echoes in a Baker’s cyst-like collection. Cytological findings were suggestive of hemorrhagic nature of the aspirate, without any evi-dence of polyethylene debris, and the cultures were sterile. She became asymptomatic over 4 weeks with conservative management; the swelling resolved after 3 months.
Conclusion: Majority of the cases in literature show implant loosening as cause of popliteal cysts after TKRs, however present cases highlight alternative mechanisms, and there are good chances of self-resolution of cysts with conservative treatment in such cases.
Keywords: Knee replacement, Baker’s cyst, deep vein thrombosis, ruptured popliteal cyst.
Popliteal cysts are associated with intra-articular knee pathologies such as meniscal degeneration, rheumatoid arthritis, or other granulomatous inflammatory diseases [1,2,3,4,5]. They constitute a rare complication of total knee replacements (TKR)/total knee arthroplasty (TKA) and are reported occasionally as indicators of implant malfunction as a result of polythene debris-induced osteolysis and foreign body reaction [6,7]. Therefore, they often relate to decreased longevity of TKR prosthesis. Symptomatically, these patients may present with pain and swelling in the calf, associated with a limp [8]. Katz et al. have named this as pseudothrombophlebitis, due to the similar nature of presentation of the two [8]. A ruptured popliteal cyst with percolation of fluid into the tissue planes can further present with symptoms mimicking deep vein thrombosis (DVT), compression of structures in posterior aspect of knee as well as compartment syndrome lower limb [9]. The fluid from these cysts have been found to contain polyethylene debris, indicating a strong relationship between osteolysis and popliteal cysts [6,10,11]. Majority of the popliteal cysts reported after TKRs have been associated with failed prosthesis. However, in rare cases where there is a symptomatic cyst formation without prosthesis malfunction, the diagnosis becomes difficult. The presentation could potentially mimic DVT, which itself is a possible complication in post-TKR patients. A positive Homan’s sign with pain on dorsiflexion of ankle can often be elicited, making it further difficult to differentiate from DVT. We present two cases of such ruptured cysts in patients who did not have any popliteal swellings in the pre-operative period, and post-operatively there was no evidence of any prosthesis loosening or polythene wear and tear. In addition, we reviewed the literature to tabulate the reported cases of Baker’s cysts formed after total knee replacements and discuss their presentation and management.
Case 1
A 55-year-old physician, suffering from Grade 4 bilateral knee osteoarthritis, was operated at our institute on April 29, 2009, with cruciate-sacrificing (CS) TKR (Oxinium; Smith and Nephew). Pre-operatively, the patient had bilateral flexion deformities; 150 on the left side and 100 on the right side, and tricompartmental osteoarthritis on radiographs (Fig. 1A-E). The patient was walking with a stick and was taking oral analgesics daily for pain and steroid replacement for pituitary hypoplasia. The surgery was uneventful, and there were no abnormal post-operative events. Physiotherapy and aided ambulation were started on post-operative day 2. At 6-week follow-up, the patient was walking comfortably, with flexion range of 0–1100 and he was undergoing regular physiotherapy.
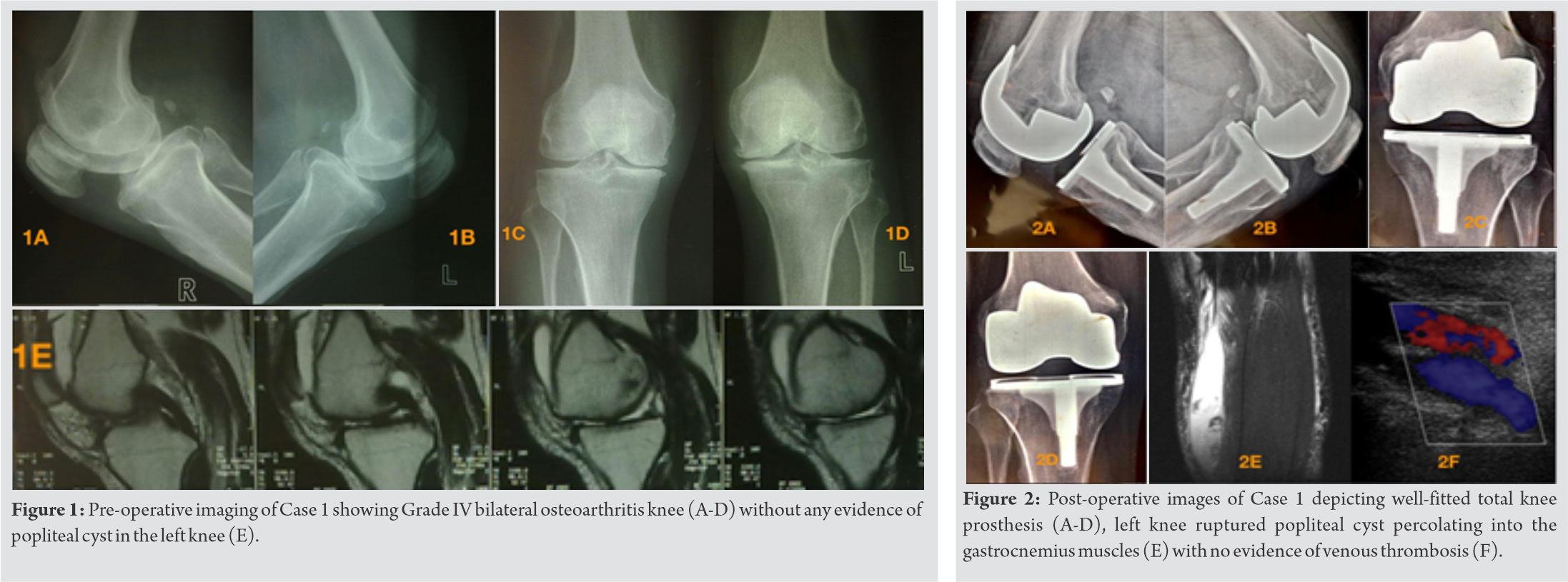
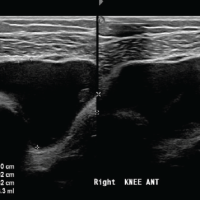
At 13 weeks, the patient presented with acute onset of pain and swelling over the posterior aspect of left knee, which progressed to involve the calf. On examination, there was no anterior knee tenderness, but tenderness was present along the posterior aspect of thigh extending to the calf. There was a cystic swelling at the popliteal fossa which was limiting knee flexion, and pain was aggravated with exercises, especially with dorsiflexion of the foot. Homan’s sign was also found to be positive. The initial suspicion was DVT and a diagnostic workup including radiographs of bilateral knee joints, color venous doppler to rule out DVT, and ultrasound (USG) of the popliteal fossa to look for any collection were done. Radiographs showed a well-fixed implant and did not show any signs of infection or loosening (Fig. 2A-D). Doppler showed a 2.7 cm ×1.8 cm ×6.0 cm hypoechoic collection in the intermuscular plane at the upper part of popliteal fossa, along with internal septations with differential diagnosis of a resolving hematoma or a ruptured popliteal cyst (Fig. 2E, F). There was no evidence of DVT. A 1.5 Tesla contrast-enhanced magnetic resonance imaging (MRI), confirmed the findings of the Doppler study; it showed the fluid from the ruptured cyst extending distally along the intermuscular gastrocnemius plane. The blood workup including total leukocytes count (7600), erythrocyte sedimentation rate (ESR- 15 mm at 1st h), and quantitative C-reactive protein (CRP-6 mg/l) were all within normal limits. The D dimer level was also normal.

Ultrasonogram guided aspiration was done with all aseptic precautions from left calf; approximately 25 ml of serosanguinous fluid, posteroinferior to the knee joint, and 20 ml fluid from inferiorly along the medial aspect of thigh and calf were aspirated. Histological examination showed mixed features of cystic fluid and a resolving hematoma. No signs of polyethylene debris or infective foci were found. The patient was advised further rest and graduated physiotherapy and there was complete resolution of the cyst in 4 months; the patient remained asymptomatic thereafter. He was regularly followed up at intervals of 3 months for 3 years, followed by 6 monthly follow-ups to look for any evidence of implant loosening, but no such findings have been seen till the last follow-up in March 2020.
Case 2
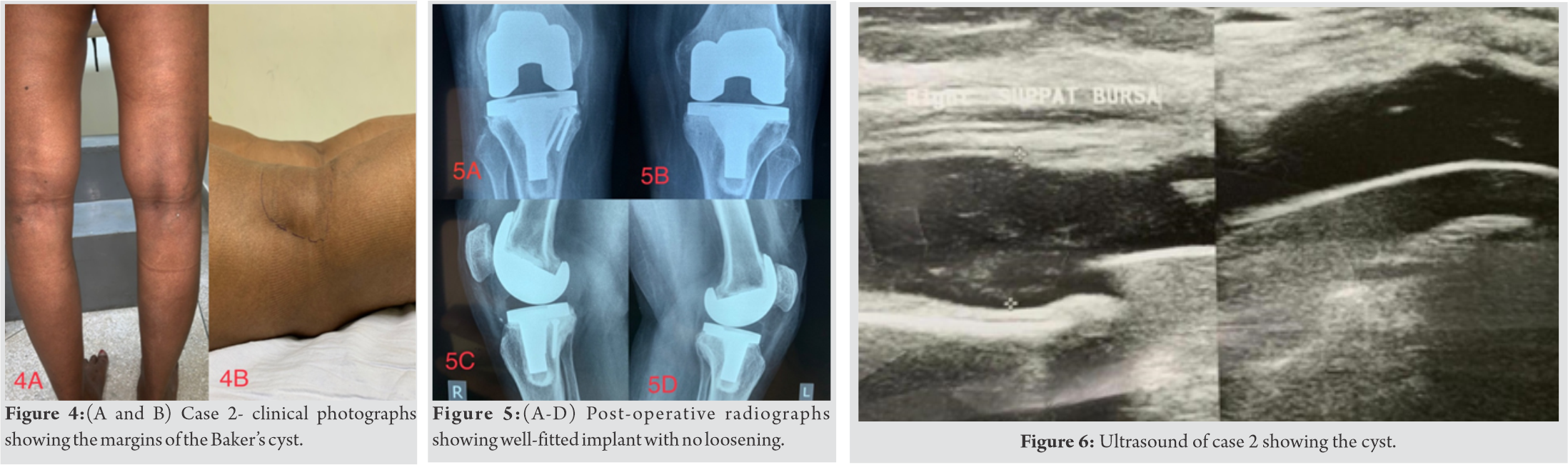
A 51-year-old female presented to our outpatient department with bilateral knee pain and difficulty in ambulation without aid. On examination, she had bilateral medial joint line tender-ness and an antalgic gait with bilateral varus thrust. Plain radiographs confirmed bilateral Grade 4 osteoarthritis (Fig. 3A-D). Bilateral TKA was done on July 27, 2015, using CS Genesis II from Smith and Nephew. The patient had an uneventful intraoperative and post-operative course with physiotherapy and aided ambulation initiated on the 2nd day after the surgery. On follow-up, the patient was pain free, was doing active physiotherapy exercises with knee flexion range of 0–1100 bilaterally, and was walking without support. Three years later, she had a fall in her bathroom and presented with pain and swelling in the left knee. She complained of the presence of a swelling in the left popliteal area for 1 year, for which she was consulting a local medical practitioner; after the fall, she developed pain in the knee for which she was referred to the primary operating surgeon. On examination, a tender swelling was palpable in the popliteal fossa, extending up to the mid-calf (Fig. 4A, B). Homan’s sign was negative and the knee flexion was restricted due to pain in the knee. All blood tests to rule out infection were within the normal range. The ESR was 12 mm at 1st hour and the quantitative CRP was 6 mg/l. The total white blood cells count was 9500 and the D- dimer levels were normal. Radiographs showed no evidence of osteolysis, fracture, or implant loosening (Fig. 5A-D). Color Doppler for DVT was negative. The USG of the cyst showed hypoechoic echoes in a Baker’s cyst-like collection (Fig. 6). Aspiration under all aseptic conditions was done, and cytological findings were suggestive of hemorrhagic nature of the aspirate, without any evidence of polyethylene debris. The cultures were sterile. The patient was advised rest, graduated physiotherapy, and minimal walking with stick. She became asymptomatic over the next 4 weeks; but a mild swelling persisted for 3 months. The patient has been asymptomatic with no complaints, and even at the last follow-up at 4-year post-TKR, there was no evidence of any implant-related issues.
Delayed pain around the knee joint following TKA is not uncommon and could be due to infection, DVT, osteolysis, loosening, or a periprosthetic fracture. Baker’s cysts as cause of pain and discomfort in the popliteal fossa after TKA are reportedly rare [6,7,9,10,11,12,13,14,15,16]. They could mimic the more common thrombophlebitis and DVT and this could further delay the diagnosis [8]. The reported prevalence of DVT after TKR has been between 40% and 80%, and any pain of sudden onset always arouses the suspicion of DVT. The rarity of Baker’s cyst makes it a difficult diagnosis. A primary PubMed search was done on 20th December 2020 with keywords; (“arthroplasty, replacement, knee”[MeSH Terms] OR (“arthroplasty”[All Fields] AND “replacement”[All Fields] AND “knee”[All Fields]) OR “knee replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “knee”[All Fields] AND “replacement”[All Fields]) OR “TKR”[All Fields]) AND (“popliteal cyst”[MeSH Terms] OR (“popliteal”[All Fields] AND “cyst”[All Fields]) OR “popliteal cyst”[All Fields] OR (“Baker’s”[All Fields] AND “cyst”[All Fields]) OR “Baker’s cyst”[All Fields]). It yielded only 22 hits. Of these, we identified 8 studies that had reported these cysts post-operatively in TKR patients (Table 1).
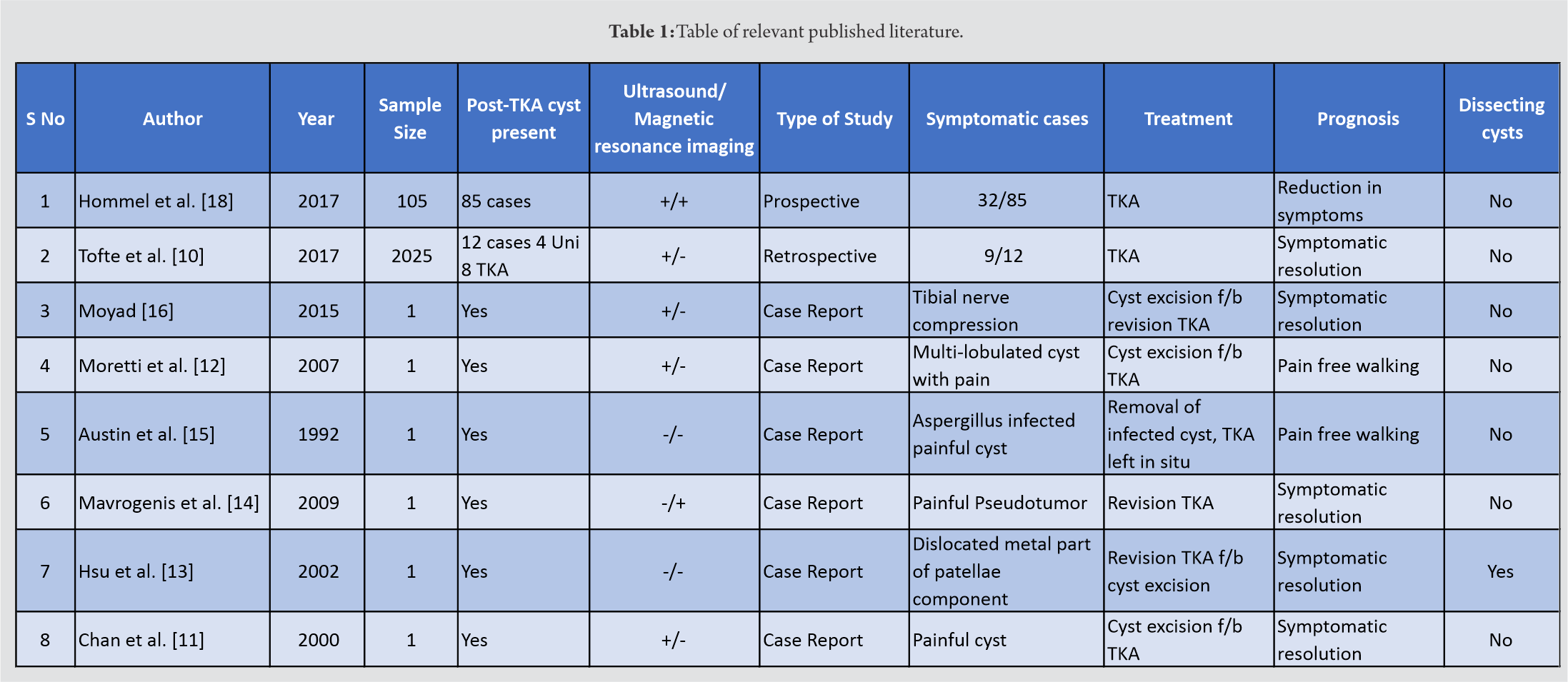
Both of our cases had ruptured cysts, and to ascertain their incidence and presentation, a secondary search was done with keywords; (“arthroplasty, replacement, knee”[MeSH Terms] OR (“arthroplasty”[All Fields] AND “replacement”[All Fields] AND “knee”[All Fields]) OR “knee replacement arthroplasty”[All Fields] OR (“total”[All Fields] AND “knee”[All Fields] AND “arthroplasty”[All Fields]) OR “TKA”[All Fields]) AND (“rupture”[MeSH Terms] OR “rupture”[All Fields] OR “ruptured”[All Fields]) AND (“popliteal cyst”[MeSH Terms] OR (“popliteal”[All Fields] AND “cyst”[All Fields]) OR “popliteal cyst”[All Fields]). This yielded 3 hits with no relevant additions to the search. Dirschl et al. reported 4 cases, where dissecting popliteal cysts were actually presenting symptoms of malfunctioning TKA prosthesis, and were managed by treating the intra-articular pathology and excision of popliteal cysts at a later stage, if and when the symptoms persisted [7]. Tofte et al. reported a prevalence of 0.6% for post-TKA cysts, most of them presenting within the 1st post-operative year [10]. They also noted that 75% patients had pre-operative symptomatic cysts that often resolved after arthroplasty. They advised observation for these Baker’s cysts, followed by USG-guided aspiration and steroid injection, if conservative management failed; surgery can be considered as the last option and includes cyst excision. Chan et al. reported a case presenting 7 years after TKA with symptoms of pain and swelling in popliteal fossa and used a two-staged management technique; they first excised the popliteal cyst to relieve the pain and at a later stage revised the loosened prosthesis with good results [11]. Hsu et al. reported a case of popliteal cyst due to dislocation of patellar prosthesis that needed revision surgery [13]. The majority of these reported cases involved implant issues. Only Pavlov et al. in one of the earliest studies described two TKR cases with rheumatoid arthritis who presented with symptoms mimicking thrombophlebitis after 2-3 years of surgery, with pain and calf swelling and a positive Homan’s sign. All the findings were pointing toward venous pathology and the diagnosis of a Baker’s cyst seemed improbable. They performed arthrography, which showed popliteal cyst dissecting into the thigh, without any evidence of implant loosening [6]. The diagnosis of these cysts become even more difficult when they rupture and the material percolates through the tissue planes, leading to soft tissue swelling and inflammation. In both of our cases, this was what happened and led to the cysts presenting with the symptoms of DVT; only on conducting all the hematological, radiological, and cytological investigations, the diagnoses of Baker’s cysts could be done. In addition, there were no prosthesis-related radiological issues that would have led to suspicion of a cyst. With our experience from the 2 cases, ruptured Baker’s cysts should be kept in the differentials of patients presenting with swelling and pain around the knee joint after TKA, especially in those patients who have associated risk factors such as a cyst in pre-operative period, hypertrophic synovium intra-operatively or who are known cases of inflammatory arthritis. TKR is considered as a stimulus for the persistence of these cysts, especially if patellar resurfacing is not done [17]. Radiographs of such patients should be scrutinised closely for any evidence of loosening, and any doubts should be further investigated with USG-guided aspiration and biopsy. A symptomatic ruptured Baker’s cyst would need aspiration and histopathology for confirmation. Furthermore, cultures should be sent from this aspirate, including fungal and tubercular cultures in immunocompromised patients [15]. If no improvement is seen with conservative management, steroid injection or excision are viable options [10]. Niki et al. mentioned the use of flow cytometry as a diagnostic tool to find macrophage containing wear debris, which can actually act as a screening method for osteolysis and early intervention [9]. In cases of loosening, staged revision surgeries have been described by some studies in patients presenting with knee pain along with ruptured/dissecting cysts, with possible usage of constrained or semi-constrained implants in 2nd stage, 4–6 weeks after primary aspiration or excision of the cyst [11,12]. On the other hand, Dirschl et al. have recommended management of the failed prosthesis primarily, with cyst excision at a later stage if symptoms persist [7]. Overall, the size of the dissecting cyst and the associated posterior pain in popliteal area and/or the calf should dictate the approach and need of initial cyst aspiration/excision. It is important to note that Baker’s cyst after TKRs, rarely present without concurrent symptoms of prosthesis failure, and they should be considered as harbingers of loosening and osteolysis of TKA [6,9]. However, in our cases, there was no implant loosening or polythene wear. Both our cases did not undergo patellar resurfacing which has been previously advocated as having a protective role against the formation of cysts and could have been the mechanism involved [18]. Overall, patients presenting with popliteal cysts post-TKR should be explained the possibility of loosening and probable need for a revision surgery; they should be kept in regular follow-ups for assessment of osteolysis.
Ruptured popliteal cysts, although very rare, can develop in the early years after TKRs. Differential diagnoses like thrombophlebitis as well as deep vein thrombosis should be kept in mind in patients presenting with posterior knee pain and swelling. Long-term regular follow-ups with radiographic examination of the prosthesis should be done keeping in mind the issues of wear, osteolysis and loosening.
Ruptured popliteal cysts in TKR patients presenting with calf pain and swelling could closely mimic DVT and they require careful diligence to diagnose and manage them. These cysts can appear even in the absence of any implant-related wear and tear and in such scenarios rest and physiotherapy can give adequate recovery.
References
- 1.Adams R. Chronic rheumatic arthritis of the knee joint. Dublin J Med Sci 1840;17:520-2. [Google Scholar | PubMed]
- 2.Baker WM. On the formation of synovial cysts in the leg in connection with disease of the knee-joint 1877. Clin Orthop Relat Res 1994;299:2-10. [Google Scholar | PubMed]
- 3.Childress HM. Popliteal cysts associated with undiagnosed posterior lesions of the medial meniscus. The significance of age in diagnosis and treatment. J Bone Joint Surg Am 1970;52:1487-92. [Google Scholar | PubMed]
- 4.Jayson MI, Dixon AS, Kates A, Pinder I, Coomes EN. Popliteal and calf cysts in rheu-matoid arthritis. Treatment by anterior synovectomy. Ann Rheum Dis 1972;31:9-15. [Google Scholar | PubMed]
- 5.Perri JA, Rodnan GP, Mankin HJ. Giant synovial cysts of the calf in patients with rheumatoid arthritis. J Bone Joint Surg Am 1968;50:709-19. [Google Scholar | PubMed]
- 6.Pavlov H, Steinbach L, Fried SH. A posterior ascending popliteal cyst mimicking thrombophlebitis following total knee arthroplasty (TKA). Clin Orthop Relat Res 1983;179:204-8. [Google Scholar | PubMed]
- 7.Dirschl DR, Lachiewicz PF. Dissecting popliteal cyst as the presenting symptom of a malfunctioning total knee arthroplasty. Report of four cases. J Arthroplasty 1992;7:37-41. [Google Scholar | PubMed]
- 8.Katz RS, Zizic TM, Arnold WP, Stevens MB. The pseudothrombophlebitis syndrome. Medicine (Baltimore) 1977;56:151-64. [Google Scholar | PubMed]
- 9.Niki Y, Matsumoto H, Otani T, Yoshimine F, Inokuchi W, Morisue H. Gigantic popliteal synovial cyst caused by wear particles after total knee arthroplasty. J Arthroplasty 2003;18:1071-5. [Google Scholar | PubMed]
- 10.Tofte JN, Holte AJ, Noiseux N. Popliteal (Baker’s) cysts in the setting of primary knee arthroplasty. Iowa Orthop J 2017;37:177. [Google Scholar | PubMed]
- 11.Chan YS, Wang CJ, Shin CH. Two-stage operation for treatment of a large dissecting popliteal cyst after failed total knee arthroplasty. J Arthroplasty 2000;15:1068-72. [Google Scholar | PubMed]
- 12.Moretti B, Patella V, Mouhsine E, Pesce V, Spinarelli A, Garofalo R. Multilobulated popliteal cyst after a failed total knee arthroplasty. Knee Surg Sports Traumatol Ar-throsc 2007;15:212-6. [Google Scholar | PubMed]
- 13.Hsu CH, Hsu RW, Huang TJ, Lee KF. Dissecting popliteal cyst resulting from a frag-mented, dislodged metal part of the patellar component after total knee arthroplas-ty. J Arthroplasty 2002;17:792-7. [Google Scholar | PubMed]
- 14.Mavrogenis AF, Nomikos GN, Sakellariou VI, Karaliotas GI, Kontovazenitis P, Papagel-opoulos PJ. Wear debris pseudotumor following total knee arthroplasty: A case re-port. J Med Case Rep 2009;3:9304. [Google Scholar | PubMed]
- 15.Austin KS, Testa NN, Luntz RK, Greene JB, Smiles S. Aspergillus infection of total knee arthroplasty presenting as a popliteal cyst. Case report and review of the literzture. J Arthroplasty 1992;7:311-4. [Google Scholar | PubMed]
- 16.Moyad TF. Massive baker cyst resulting in tibial nerve compression neuropathy sec-ondary to polyethylene wear disease. Am J Orthop (Belle Mead NJ) 2015;44:E113-6. [Google Scholar | PubMed]
- 17.Ruban P, Yeo SJ, Seow KH, Tan SK, Ng SC. Deep vein thrombosis after total knee re-placement. Ann Acad Med Singap 2000;29:428-33. [Google Scholar | PubMed]
- 18.Hommel H, Perka C, Kopf S. The fate of Baker’s cyst after total knee arthroplasty. Bone Joint J 2016;98-B:1185-8. [Google Scholar | PubMed]