Anchor site fractures are a potential complication in rotator cuff repair. Anchor positioning, quantity and material should thus be chosen wisely and patients counselled accordingly.
Dr. Björn Birkner,
Stiftsstraße 3, 79618 Rheinfelden, Germany.
E-mail: bjoern-birkner@web.de
Introduction: Fractures at the anchor site following arthroscopic rotator cuff repair are rare and only a few case reports have been described. We report two additional well-documented cases of this uncommon post-operative complication and provide a review of the current literature.
Case Report: A 48-year-old male underwent arthroscopic rotator cuff repair (ARCR) due to a massive rotator cuff tear. Nine weeks postoperatively, the patient suffered a humeral head fracture at the anchor site of the ARCR after trauma. Despite subsequent surgical treatment with open reduction and internal fixation, the patient demonstrates with excellent functional outcome scores at 2-year follow-up.
Conclusion: Humeral head fractures are a rare complication after ARCR. The use of intraosseous anchors requires careful consideration regarding positioning and quantity used.
Keywords: Rotator cuff, arthroscopy, complication, anchor, Speed Bridge, fracture, osteochondral defect.
Rotator cuff pathologies are a common finding in the shoulder joint with an estimated incidence of 87/100,000 person-years. The annual incidence of full-thickness rotator cuff tears (RCTs) is reported to be at 16/100,000 persons aged 18–75 years [1,2,3,4]. RCTs can either be degenerative or traumatic and treatment varies depending on patient age and demand as well as type of tear and corresponding tissue quality [5]. In the young demanding patient, surgical treatment is usually recommended [5]. The current gold standard surgical treatment is the arthroscopic rotator cuff repair (ARCR) using intraosseous suture anchors [5,6]. With increasing patient age and demand as well as advancing surgical techniques, the annual incidence of performed ARCR is constantly increasing: From 23.5/100.000 persons in 1995 to 83.1 in 2009 [7]. With more arthroscopies are performed, anchor-related complications are rising [8,9]. While loosening or intra-articular migration is frequently reported, anchor site-related fractures have rarely been described in literature [10,11,12]. We report a case of a traumatic anchor site fracture 9 weeks following ARCR in a 48-year-old male patient and provide a review of the literature. The patient was informed about and consented before publication of data.
A 48-year-old male patient (186 cm, 88 kg) was referred to our orthopedic outpatient clinic with a history of atraumatic persisting left shoulder pain lasting for several months. Physiotherapy, oral analgesics, and subacromial infiltrations showed no lasting effect. Magnetic resonance imaging revealed an RCT of M. supraspinatus (Patte Grade I; Goutallier/Fuchs Type I) and M. subscapularis (Lafosse Type I) [13,14,15]. The patient underwent ARCR using a suture bridge-like construct (SpeedBridge™ [SB], Arthrex, Naples, Florida, USA) for rotator cuff repair as well as an LHB tenodesis through one BioComposite SwiveLock™ (Arthrex, Naples, Florida, USA). The cranial part of the partially torn subscapularis tendon was attached to the LHB anchor.
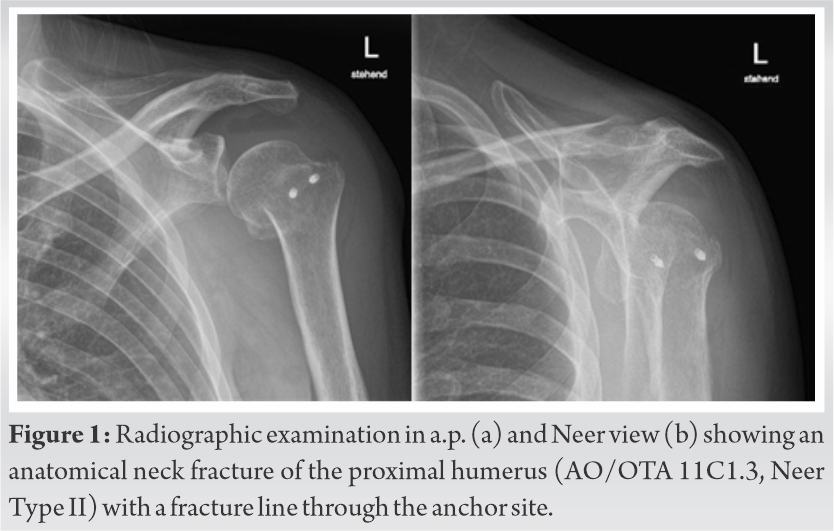
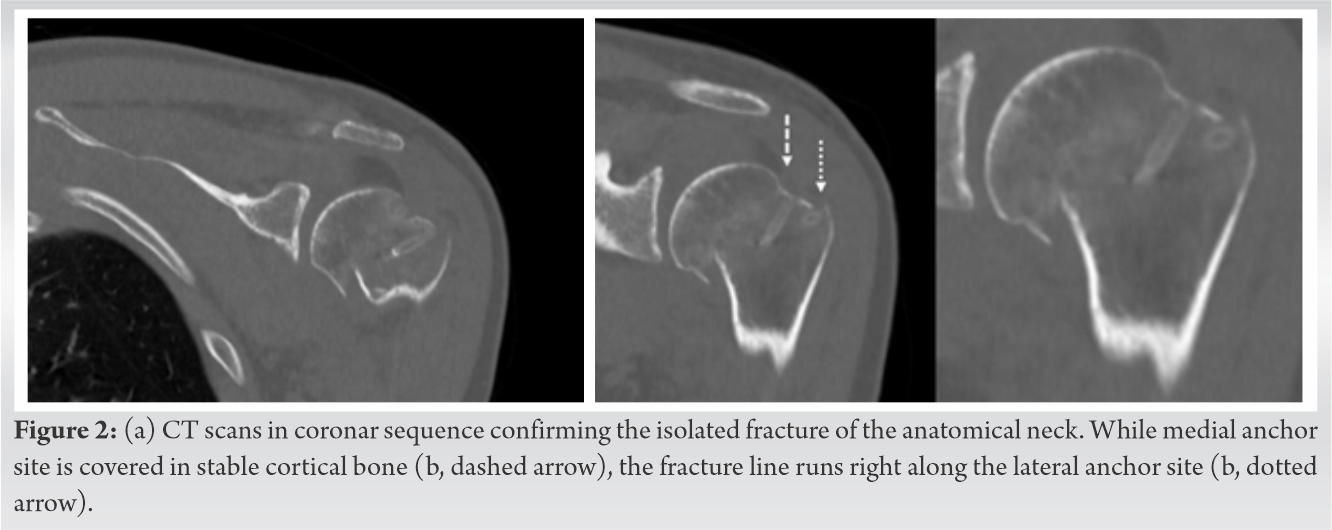
At 6-week follow-up, the patient showed an adequate range of passive motion and no signs of shoulder stiffness. Nine weeks postoperatively, the patient suffered a low-velocity trauma to his left shoulder. He presented to the emergency room with immobilizing pain rated 9/10 on the numeric analog scale. Radiographic examination (Fig. 1a, b) and a computer tomography scan (CT, Fig. 2a, b) revealed an isolated fracture of the proximal humeral head (AO/OTA fracture and dislocation classification 11C1.3) [16]. The fracture line was located right at the lateral site of the suture bridge construct close to the anatomic neck (Neer Type II, [17]). Due to a displacement of 1 cm, surgical refixation was advised. Under general anesthesia, the fracture site was exposed using a delta split approach.
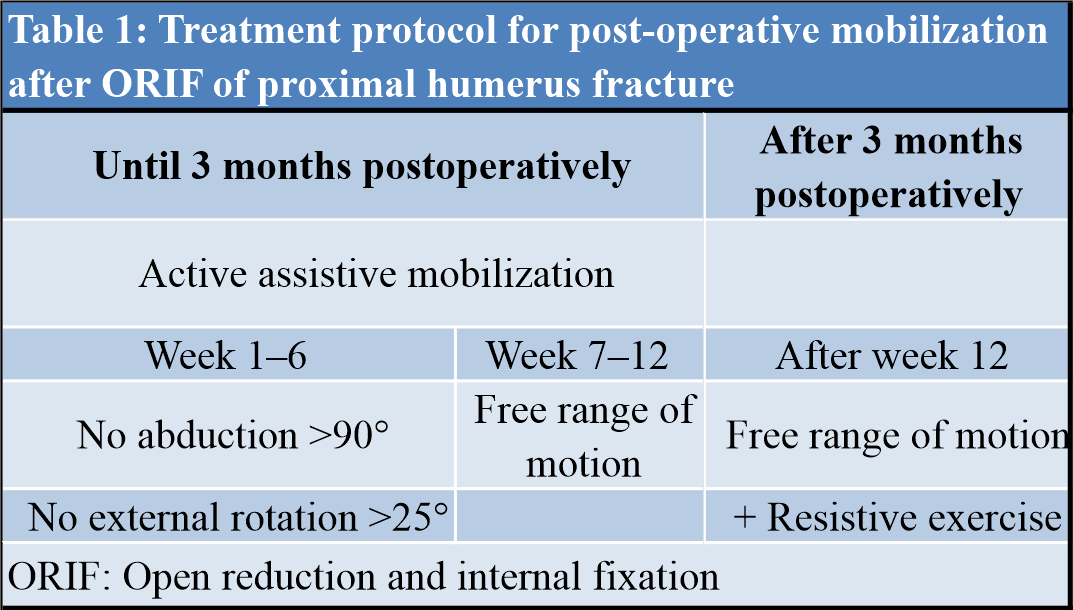
Total reruptures of previously reconstructed rotator cuff tendons were detected, and anchor material was removed. The fracture was reduced, and definitive fixation was performed with a PHILOS™-Plate system (DePuy Synthes, Warsaw, Indiana, USA). Rotator cuff tendons were reconstructed and additionally attached to the plate through Ethibond® fibers (Ethicon, Somerville, Massachusetts) in Mason-Allen technique. Post-operative radiographs showed good reduction of the fracture so that post-operative rehabilitation following a standardized protocol was initiated (Table 1).
At 3-month follow-up, the fracture healed anatomically with the patient’s passive range of motion already within normal limits. Constant score was 68 and improved to 92 points at 1-year and 2-year follow-up. Radiographic examination at 1-year follow-up revealed adequate fracture consolidation (Fig. 3a, b).

Rotator cuff injuries are common within the elderly [4]. While a substantial injury is rare in the young, it is seen in 50% of individuals over 80 years [2,3,4]. In most cases, the acute injury is based on chronic degenerative changes [3]. Surgical treatment is usually recommended in the young and conservative treatment in patients older than 65 years [7,8]. Due to the patient’s age and persisting symptoms, surgical treatment was advised. Over the past decades, various technical developments in rotator cuff repair have been reported. While open rotator cuff repair was the standard treatment in the 1990s [3], advances in arthroscopic surgery have led to the current gold standard of ARCR [7]. Various surgical techniques are described [18]: SB – as used in this case – is a technical variant of the SutureBridge™ (Arthrex, Naples, Florida, USA) which uses two BioComposite SwiveLock™ anchors (Diameter 4.75 mm, Arthrex, Naples, Florida, USA) at the medial site with attached FiberTape® (Arthrex, Naples, Florida, USA). Lateral attachment is achieved by sewing the muscle tendon and attachment of the FiberTape® through a pair of self-punching SwiveLock™ anchors (Diameter 5.5 mm, Arthrex, Naples, Florida, USA) of the same origin. Theoretically, a flat spread contact pressure is built to achieve a satisfying healing response of the reattached tendon. Tenodesis of the long head of the biceps is performed by inserting a SwiveLock™ anchor in the bicipital groove after tendon reinforcement through FiberWire® (Arthrex, Naples, Florida, USA). There were only 10 adverse events reported to the U.S. Food and Drug Administration concerning comparable anchor systems (Keyword Arthrex, Naples, Florida, USA) between January 1, 2010, and March 17, 2020 [19]. Reported events consisted of breakage (8 events) and intra-articular remnants (2 events).
Since absorbable suture anchors showed similar pull-out strengths as transosseous fixation they became more common in orthopedic surgery. Their use decreased operation time as well as violated osseous surface [20]. In shoulder studies, Warme et al. found no significant differences in the functional outcome between absorbable and non-absorbable anchor material [20]. However, improper use of both anchor types led to articular compromise if implants migrate: The post-operative radiographic assessment showed a doubling of anchor holes’ size after 6 months and focal osteonecrosis at drilling site [21]. There is some normalization using absorbable anchors where biodegradation can vary from 3 months to over 32 months [20,22]. Since trauma in our case occurred 9 weeks postoperatively and radiographic assessment showed that the anchor material was not degraded or migrated, long-term changes are unlikely to play an important role. If taking those into account (osteolysis, cystic resorption, etc.), we doubt a full return of stability even years after anchor repair [8,21,23,24,25]. Partly these complications are likely not anchor – but technique related (e.g., focal necrosis due to drilling) [8,21,24,25].
Furthermore, since rotator cuff anchors were not implanted after drilling but pushing a punch into the bone, thermic osteonecrosis cannot explain the osseous instability at the anchor site. In osteosynthesis studies, a drill hole of 20% of the diameter of the bone is reported to reduce the bony stability by 40% [26]. In the presented case, the fracture lines accurately passed through the anchor site. Conveniently, the use of two anchors at lateral site of the SB combines to a ratio of >20% of the bone dimension just below fracture line ((2 mm × 5.5 mm)/39.3 mmCT-coronar = 0.28; (2 mm × 5.5 mm)/33.7 mmCT-sagittal = 0.33). The lateral anchor site seems to be weaker than its medial counterpart at least in SutureBridge technique [10]. While changes of the individual osseous structure unlikely play a role – the patient was younger than 50 years and male [27] – biomechanically, two factors may contribute to osseous damage even in younger patients: Strauss et al. reported that anchor positioning in Deadman’s angle (45° to bone surface) not only leads to lesser pull-out strength and this may have contributed to an unfavorable force transmission in our case [28]. Considering correct position, bone quality and cortical thickness were best 15–21 mm below the summit of the greater tubercle in a CT microanalysis study of 13 specimens and therefore offer highest stability for anchor implantation. One may argue that this was not achieved in our case (approx. 8–10 mm below summit) and may have favored instability at a much weaker site [29]. Interestingly, the anchors with a larger diameter were used within the lateral row in our patient (5.5 mm vs. 4.75 mm, read above). Fractures around the anchor site following ARCR are rare, and in literature, there are only a few cases described: Shah et al. reported on a fracture to the humeral anchor site following repair of the musculus pectoralis major [12]. Fritsch et al. reported glenoid rim fractures after arthroscopic Bankart repair that fractured again after low-velocity trauma in sports right at the anchor site [30] and Park et al. described the case of a 47-year-old woman with a fracture along the anatomical neck of the humerus following ARCR [10].
Overall, ARCR seems to be a favorable evolution of orthopedic shoulder surgery. However, there are possible complications that differ in origin and severity. Fractures around the anchor site are severe complications but seem to be rare [8,9]. Our reported case strengthens that rotator cuff anchors need to be chosen wisely regarding quantity, quality, and exact positioning. Furthermore, patients need to be sensitized for this rare, but possible post-operative risk before surgery.
Fractures at anchor site are a rare complication after arthroscopic rotator cuff repair. Nevertheless, patients need to be informed about this post-operative event due to its severe impact on overall outcome.
References
- 1.Aagaard KE, Abu-Zidan F, Lunsjo K. High incidence of acute full-thickness rotator cuff tears. Acta Orthop 2015;86:558-62. [Google Scholar | PubMed]
- 2.Berhouet J, Collin P, Benkalfate T, Le Du C, Duparc F, Courage O, et al. Massive rotator cuff tears in patients younger than 65 years. Epidemiology and characteristics. Orthop Traumatol Surg Res 2009;95:13-8. [Google Scholar | PubMed]
- 3.Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med 2012;31:589-604. [Google Scholar | PubMed]
- 4.White JJ, Titchener AG, Fakis A, Tambe AA, Hubbard RB, Clark DI. An epidemiological study of rotator cuff pathology using The Health Improvement Network database. Bone Joint J 2014;96-B:350-3. [Google Scholar | PubMed]
- 5.Favard L, Berhouet J, Colmar M, Boukobza E, Richou J, Sonnard A, et al. Massive rotator cuff tears in patients younger than 65 years. What treatment options are available? Orthop Traumatol Surg Res 2009;95:S19-26. [Google Scholar | PubMed]
- 6.Lin CL, Yeh ML, Su FC, Wang YC, Chiang CH, Hong CK, et al. Different suture anchor fixation techniques affect contact properties in humeral greater tuberosity fracture: A biomechanical study. BMC Musculoskelet Disord 2019;20:26. [Google Scholar | PubMed]
- 7.Ensor KL, Kwon YW, DiBeneditto MR, Zuckerman JD, Rokito AS. The rising incidence of rotator cuff repairs. J Shoulder Elbow Surg 2013;22:1628-32. [Google Scholar | PubMed]
- 8.Audigé L, Blum R, Müller AM, Flury M, Durchholz H. Complications following arthroscopic rotator cuff tear repair: A systematic review of terms and definitions with focus on shoulder stiffness. Orthop J Sports Med 2015;3:2325967115587861. [Google Scholar | PubMed]
- 9.Audigé L, Flury M, Müller AM, Durchholz H, ARCR CES Consensus Panel. Complications associated with arthroscopic rotator cuff tear repair: Definition of a core event set by Delphi consensus process. J Shoulder Elbow Surg 2016;25:1907-17. [Google Scholar | PubMed]
- 10.Park KJ, Kim YM, Kim DS, Choi ES, Keum SW, Kil KM, et al. Fracture of proximal humerus in the lateral anchor site after suture bridge repair: A case report. Clin Shoulder Elbow 2014;17:134-7. [Google Scholar | PubMed]
- 11.Banerjee S, Weiser L, Connell D, Wallace AL. Glenoid rim fracture in contact athletes with absorbable suture anchor reconstruction. Arthroscopy 2009;25:560-2. [Google Scholar | PubMed]
- 12.Shah J, Marson BA. A case report of periprosthetic fracture left proximal humerus with radial nerve palsy following pectoralis major repair. Clin Case Rep 2015;3:468-71. [Google Scholar | PubMed]
- 13.Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202. [Google Scholar | PubMed]
- 14.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;304:78-83. [Google Scholar | PubMed]
- 15.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res 1990;254:81-6. [Google Scholar | PubMed]
- 16.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma 2018;32 Suppl 1:S1-170. [Google Scholar | PubMed]
- 17.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077-89. [Google Scholar | PubMed]
- 18.Burkhart SS, Lo IK. Arthroscopic rotator cuff repair. J Am Acad Orthop Surg 2006;14:333-46. [Google Scholar | PubMed]
- 19.Medsun Reports. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/medsun/searchreport.cfm. [Last Accessed on 2020 Mar 17]. [Google Scholar | PubMed]
- 20.Warme WJ, Arciero RA, Savoie FH, Uhorchak JM, Walton M. Nonabsorbable versus absorbable suture anchors for open Bankart repair. A prospective, randomized comparison. Am J Sports Med 1999;27:742-6. [Google Scholar | PubMed]
- 21.Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med 2012;40:1424-30. [Google Scholar | PubMed]
- 22.Willcox N, Roberts S. Delayed biodegradation of a meniscal screw. Arthroscopy 2004;20 Suppl 2:20-2. [Google Scholar | PubMed]
- 23.Athwal GS, Shridharani SM, O’Driscoll SW. Osteolysis and arthropathy of the shoulder after use of bioabsorbable knotless suture anchors. A report of four cases. J Bone Joint Surg Am 2006;88:1840-5. [Google Scholar | PubMed]
- 24.Gunja NJ, Athanasiou KA. Biodegradable materials in arthroscopy. Sports Med Arthrosc Rev 2006;14:112-9. [Google Scholar | PubMed]
- 25.Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy 2009;25:788-93. [Google Scholar | PubMed]
- 26.Pandey RK, Panda SS. Drilling of bone: A comprehensive review. J Clin Orthop Trauma 2013;4:15-30. [Google Scholar | PubMed]
- 27.Iqbal M. Osteoporosis: Epidemiology, diagnosis, and treatment. South Med J 2000;93:2-18. [Google Scholar | PubMed]
- 28.Strauss E, Frank D, Kubiak E, Kummer F, Rokito A. The effect of the angle of suture anchor insertion on fixation failure at the tendon-suture interface after rotator cuff repair: Deadman’s angle revisited. Arthroscopy 2009;25:597-602. [Google Scholar | PubMed]
- 29.Zumstein MA, Raniga S, Labrinidis A, Eng K, Bain GI, Moor BK. Optimal lateral row anchor positioning in posterior-superior transosseous equivalent rotator cuff repair: A micro-computed tomography study. Orthop J Sports Med 2016;4:2325967116671305. [Google Scholar | PubMed]
- 30.Fritsch BA, Arciero RA, Taylor DC. Glenoid rim fracture after anchor repair: A report of 4 cases. Am J Sports Med 2010;38:1682-6. [Google Scholar | PubMed]









