Wrong entry of locking bolt from lateral to medial end may cause pseudoaneurysm of an anterior tibial artery.
Dr. Nishant D Goyal,
Department of Orthopaedics, Deenanath Mangeshkar Hospital and Research Centre, Pune, Maharashtra, India.
E-mail: nishantdgoyal@gmail.com
Introduction: Interlocking tibia nail fixation for tibia shaft fracture treatment is one of the most commonest procedures performed in orthopedic trauma practices. We report one such case of a rare complication of anterior tibial artery (ATA) pseudo-aneurysm caused by the proximal coronal locking bolt performed by an unusual entry from lateral to medial side during shaft of tibia fracture fixation.
Case Report: A 86- years old female sustained a road traffic accident and was diagnosed with a closed tibia shaft fracture of the right leg for which she underwent intramedullary interlocking nail IMIL nailing elsewhere. She presented to us three 3 weeks after primary surgery with persistent pain and swelling in the right leg proximally. We investigated and diagnosed her as having a pseudoaneurysm of the Anterior Tibial Artery on color Doppler and magnetic resonance imaging (MRI) angiography. The pseudoaneurysm of ATA was clipped without any complications. To avoid the rupture of the pseudoaneurysm during manipulation of nail and bolts, their positions were not changed as they were supporting the fracture well and the fracture was also not united at that time.
Conclusion: Though Although interlocking nailing of tibia shaft fracture is a commonly performed procedure, it can lead to disastrous vascular complications if the procedure is not performed with utmost care. ATA injury by proximal locking bolts of the tibia nail mandates the need for reconsideration of the nail design with better screw hole positions. We recommend preferring standard AO manual instructions for proximal tibia locking bolt direction.
Keywords: Pseudo-aneurysm, tibia nail, locking bolt, anterior tibial artery.
Orthopaedic procedures such as proximal tibia pin insertion and proximal locking of the the intramedullary interlocking nail (IMIL) is are a routinely performed procedure on proximal tibia. Many complications are related to this procedure such as infection at the site of pin tract, loosening of the pin, and foot drop due to incorrect placement of pins or screws injuring the common peroneal nerve [1]. Vascular injury during intramedullary interlocking (IMIL) tibia nail surgery is one of such potentially disastrous complications [2, 3]. In the literature, these injuries are usually under-reported. Till now, there is only one case of anterior tibial artery (ATA) injury caused by the proximal locking bolt of the IMIL tibia nail [4]. We hereby report a case of a rare complication of ATA pseudo-aneurysm caused by the proximal coronal locking bolt performed by an unusual entry from lateral to medial side during shaft of tibia fracture fixation using IMIL nail.
A 86- years old lady sustained a road traffic accident and was diagnosed with a closed tibia shaft fracture of the right leg for which she underwent IMIL nailing elsewhere. She presented to us three 3 weeks after primary surgery with persistent pain and swelling in the right leg proximally as shown in (Fig. 1). We investigated and diagnosed her as having a pseudoaneurysm of the Anterior Tibial Artery on color Doppler and magnetic resonance imaging (MRI) angiography as shown in (Fig. 2). We hypothesized that the unusual position of the proximal locking bolt from the lateral to the medial side can be a potential cause of it. Initially, we tried to treat her conservatively with anti-inflammatory and analgesics but her symptoms did not improve. A vascular surgeon was called to clip her ATA to manage the patient’s symptoms. To avoid the rupture of the pseudoaneurysm during manipulation of nail and bolts, their positions were not changed as they were supporting the fracture well and the fracture was also not united at that time. 8 Eight months following the indexed surgery, the patient was completely asymptomatic and was walking full weight-bearing without any support. The X-ray confirms fracture union. Unusual proximal bolts entry from lateral to medial and clips of ATA are also noted in X-rays as shown in (Fig. 3).
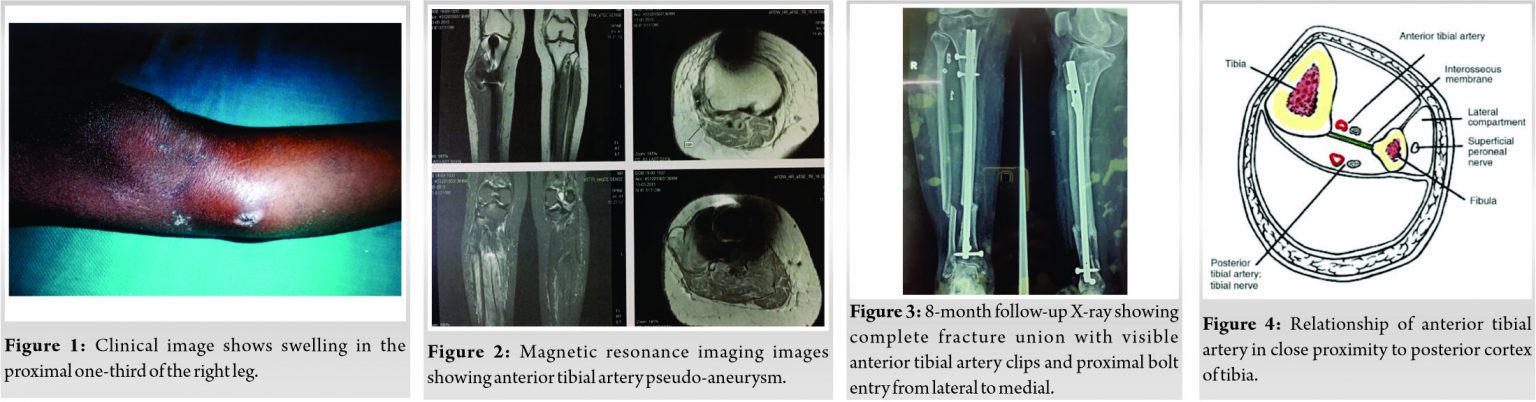
Pseudoaneurysm of the ATA following IMIL tibia nail is a very rare complication, although pseudoaneurysm following femoral interlocking nailing has been reported [5]. The ATA is a branch of the popliteal artery arising at the distal border of the popliteus muscle. It then enters the anterior compartment by hooking over the proximal border of the interosseous membrane, approximately at the level of the fibular head. This peculiar course makes the artery relatively fixed, reducing its mobility, and making it more prone to injury [6]. High origin anterior tibial artery ATA is the one where it branches proximal to popliteus muscle and courses anterior to this muscle in close proximity to the posterior cortex of tibia, such variations will pose increased risk for injury during procedures performed at the level of proximal tibia such as high tibial osteotomy, total knee replacement surgeries when performing tibial cuts [7]. Other anatomic variation in anterior tibial artery ATA origin can be a trifurcation of the popliteal artery simultaneously which normally gives anterior tibial artery ATA first and then posterior tibial and peroneal arteries arising from the common tibial-peroneal trunk. False aneurysms with a fibrous tissue wall instead of the regular artery wall found in true aneurysms are known as pseudoaneurysms. They develop when a rent forms in the artery wall and progressively bleeds out into the surrounding tissues. An expanding hematoma occurs as a result of this [8]. Most of the time, blood flow is maintained through the parent artery, which is why physical examinations reveal patent pulses. The symptoms of a traumatic aneurysm are caused by pressure on the surrounding tissues, which causes pain, numbness, or muscular weakness distal to the lesion due to nerve pressure. Such pseudo aneurysms are known to occur in rare incidence following trauma to the leg leading to fracture of tibia, arthroscopy of ankle joint and injury by the ilizarov pins during the application of the fixator. Tibia is a triangular shaped long bone in cross section and it is recommened to insert screws in posterior half to have a better purchase of the two cortices, but placing the screws too posterior makes it a risk factor for injury to the ATA as the artery is very close to the posterior cortex as depicted in (Fig. 4, 3). Various studies quoted that ATA passes near the neck of the fibula, [4, 9, 10, 11], which is approximately the level of the distal bolt out of the two proximal bolts of IMIL tibia nail, making it a potential source of injury during drilling or due to long screws lengths. Various precautions are to be taken to prevent such vascular complications which are discussed below.
• Entry of proximal locking bolt to be taken cautiously and it should be from medial to the lateral side.
• Ensuring the proper positioning of the jig by the surgeon.
• While drilling for a proximal locking bolt it is advisable to actively feel for the far cortex;, however, it is known that far cortex feel may not be there because of the cancellous nature of bone [12].
• Continuous C arm monitoring is advised. Due to the triangular shape of the proximal tibia in the cross-section, one can have a false impression of drill length. Thus, C arm image may be misleading and therefore it is suggested to check for drill and screw length in various degrees of internal and external rotation.
• The drill bit length should be kept short. The length of the drill outside the sleeve should not be more than the approximate diameter of the bone.
Depending on the site, size, and clinical signs and symptoms, the period from damage to discovery of the pseudoaneurysm has been observed to presnt present from hours to years. Pain, swelling, a pulsatile mass, an audible bruit, distant emboli, blood seeping from the surgical site, and neurological impairment are examples of the latter. They might look like abscesses, neoplasms, or ganglions in soft tissue [13,14,15,16]. In such instances, inadvertent surgery might result in uncontrollable bleeding. As a result, while dealing with swellings near a major vessel, a high index of suspicion is justified [17]. To avoid the consequences of rupture or fast enlargement with resulting pressure on the surrounding nerves, surgical repair of a pseudo aneurysm should be undertaken as soon as feasible once the diagnosis is confirmed. If neurological problems appear, immediate surgery is recommended [17]. For the treatment of a pseudoaneurysm, several techniques of repair have been reported in the literature, namely, excision of the aneurysmal sac and lateral wall repair, endoaneurysmorrhaphy obliterative or reconstructive, limited arterial resection, and end-to-end anastomosis, resection, and graft placement and ligation of the artery. [18,19,20,21,22]. The comparative studies regarding arterial pseusoaneurysms were are tabulated in (Table 1).
Literature is silent about the entry of proximal locking bolts during IMIL tibia nail fixation. ATA injury by proximal locking bolts of the tibia nail mandates the need for reconsideration of the nail design with better screw hole positions. We recommend preferring standard AO manual instructions for proximal tibia locking bolt direction. Any localized swelling in the proximal leg following the IMIL tibia nail should be dealt with carefully and appropriate investigations should be performed before any intervention to prevent disastrous complications. Various precautions as discussed earlier should be taken to prevent vascular complications.
Though Although routinely performed, IMIL tibia nails should always be done with utmost care to avoid potential complications. Diagnosing vascular injuries after tibia nails can be confusing clinically. One should always have an eagle’’s eye and give a benefit of doubt to such injuries and call for appropriate investigation before performing any intervention to prevent disastrous complications.
References
- 1.Koval KJ, Clapper MF, Brumback RJ, Ellison PS, Poka A, Bathon GH, et al. Complications of reamed intramedullary nailing of the tibia. J Orthop Trauma 1991;5:184-9. [Google Scholar | PubMed]
- 2.Fanter NJ, Inouye SE, Beiser CW. The risk of iatrogenic injury to anterior tibial artery variations during tibial nail distal interlocking. J Orthop Surg (Hong Kong) 2017;25:???. [Google Scholar | PubMed]
- 3.Zelle BA, Boni G. Safe surgical technique: Intramedullary nail fixation of tibial shaft fractures. Patient Saf Surg 2015;9:40. [Google Scholar | PubMed]
- 4.Inamdar D, Alagappan M, Shyam L, Devadoss S, Devadoss A. Pseudoaneurysm of anterior tibial artery following tibial nailing: A case report. J Orthop Surg (Hong Kong) 2005;13:186-9. [Google Scholar | PubMed]
- 5.Dickson JW. False aneurysm after intramedullary nailing of the femur. J Bone Joint Surg Br 1968;50:144-5. [Google Scholar | PubMed]
- 6.Starling S, Ellis H. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 42nd ed. Edinburgh: Churchill Livingstone; 2005. Available from: https://www.elsevier.com/books/grays-anatomy/standring/978-0-7020-7705-0. [Google Scholar | PubMed]
- 7.Tindall A, Shetty AA, James KD, Middleton A, Fernando KW. Prevalence and surgical significance of a high-origin anterior tibial artery. J Orthop Surg (Hong Kong) 2006;14:13-6. [Google Scholar | PubMed]
- 8.Suri T, Dabas V, Sural S, Dhal A. Pseudoaneurysm of the anterior tibial artery: A rare complication of proximal tibial steinman pin insertion. Indian J Orthop 2011;45:178-80. [Google Scholar | PubMed]
- 9.Day CP, Orme R. Popliteal artery branching patterns–an angiographic study. Clin Radiol 2006;61:696-9. [Google Scholar | PubMed]
- 10.Bono CM, Sirkin M, Sabatino CT, Reilly MC, Tarkin I, Behrens FF. Neurovascular and tendinous damage with placement of anteroposterior distal locking bolts in the tibia. J Orthop Trauma 2003;17:677-82. [Google Scholar | PubMed]
- 11.Gahlot N, Kanojia RK. Anterior tibial artery pseudoaneurysm due to interlocking bolt of tibial nail: A case report and review. Acta Orthop Traumatol Turc 2017;51:77-83. [Google Scholar | PubMed]
- 12.Dominguez R, de Santos LA. Traumatic pseudoaneurysm of the anterior tibial artery simulating soft tissue malignancy. Skeletal Radiol 1986;15:622-4. [Google Scholar | PubMed]
- 13.Gantz ED, Sweet MB, Jakim I. False aneurysm mimicking an aggressive soft-tissue tumor. A case report. J Bone Joint Surg Am 1988;70:1090-2. [Google Scholar | PubMed]
- 14.Albert S, Daniel S, Gouse M, Cherian VM. Case of pseudoaneurysm mimicking a soft tissue sarcoma: A diagnostic pitfall. Malays J Med Sci 2015;22:61-4. [Google Scholar | PubMed]
- 15.Dhal A, Chadha M, Lal H, Singh T, Tyagi S. Encounters with pseudoaneurysms in orthopaedic practice. Injury 2001;32:771-8. [Google Scholar | PubMed]
- 16.Bloom AI, Sasson T, Verstandig A, Wolf YG, Anner H, Berlatzky Y, et al. Ultrasound-guided thrombin injection for the treatment of iatrogenic pseudoaneurysm of the femoral artery. Israel Med Assoc J 2001;3:649-52. [Google Scholar | PubMed]
- 17.Tielliu IF, Verhoeven EL, Prins TR, Post WJ, Hulsebos RG, van den Dungen JJ. Treatment of popliteal artery aneurysms with the Hemobahn stent-graft. J Endovasc Ther 2003;10:111-6. [Google Scholar | PubMed]
- 18.van Rooij WJ, Sluzewski M. Endovascular treatment of large and giant aneurysms. Am J Neuroradiol 2009;30:12-8. [Google Scholar | PubMed]
- 19.Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics 2005;25:S173-89. [Google Scholar | PubMed]
- 20.Savolainen H, Baumgartner I, Schmidli J, Heller G, Do DD, Willenberg T. Femoral pseudoaneurysms requiring surgical treatment. Trauma Mon 2012;16:194-7. [Google Scholar | PubMed]
- 21.Williamson DM, Kershaw CJ. Serious vascular complication of locked tibial nailing. Injury 1989;20:310-2. [Google Scholar | PubMed]
- 22.Urban WP, Tornetta P. Vascular compromise after intramedullary nailing of the tibia: A case report. J Trauma 1995;38:804-7. [Google Scholar | PubMed]
- 23.Mehta S, Cumins C, Milgram R. Anterior tibial artery impingement by a distal interlocking screw: A case report. Univ Pa Orthop J 2003;16:35e37. [Google Scholar | PubMed]
- 24.Han KJ, Won YY, Khang SY. Pseudoaneurysm after tibial nailing. Clin Orthop Relat Res 2004;418:209-12. [Google Scholar | PubMed]
- 25.Hussain W, Balach T, Leland JM. Vascular injury involving proximal medial-to-lateral oblique locking screw insertion in tibial intramedullary nailing. Acta Orthop Belg 2011;77:414-8. [Google Scholar | PubMed]
- 26.Spencer FC, Imparato AM. In: Schwartz SI, Lillehei RC, Shires GT, Spencer FC, Storer EH, editors. Peripheral Arterial Disease. 2nd ed. New York: McGraw Hill; 1969. [Google Scholar | PubMed]